Hip arthroplasty is the treatment of choice for displaced femoral neck fractures among the older population. The hip prosthesis dislocation is one of the most pointed potential complications after hip arthroplasty, but there is a lack of updated information on the effect of dislocation on the survival of older hip fracture patients so treated by hip hemiarthroplasty. We aim to evaluate the standalone effect of hip prosthesis dislocation after hip fracture hemiarthroplasty on patients’ survival outcomes.
Materials and methodsWe conducted a retrospective multicenter study, including 6631 femoral neck fracture patients over 65 surgically treated by hemiarthroplasty. We made follow-up cut-offs 30-days, 6 weeks, 90-days, and one year after hospital discharge determining hip dislocation rate and patients’ survival.
ResultsThe women population represented 78.7%, and the mean age of the population was 85.2±6.7 years. Hip prosthesis dislocation incidence was 1.9% in the first 90-days after discharge, representing 91.54% of primary dislocations yearly noted. We reported statistically significant increased mortality rates of patients presenting at least one hip prosthesis dislocation event (from 16.0% to 24.6% at 90-day after discharge, and 29.5% to 44.7% at one year), and also significantly decreasing patient survival function at 90-day (p=0.016) and one-year follow-up (p<0.001). The recurrent dislocation events (26.15%) showed even higher mortality rates (up to 60.6%, p<0.001). The multivariate Cox regression model determined that prosthesis dislocation was the only significant variable (p=0.035) affecting patient survival, increasing the risk of dying before one year of follow-up by 2.7 times.
DiscussionOur study stands for the standalone hip prosthesis dislocation entailing a higher risk of death after hip fracture hemiarthroplasty in the older population.
La artroplastia de cadera es el tratamiento de elección para las fracturas desplazadas del cuello de fémur en la población de edad avanzada. La luxación de la prótesis de cadera es una de las complicaciones potenciales tras la artroplastia de cadera, pero falta información actualizada sobre el efecto de la luxación en la supervivencia de los pacientes mayores con fractura de cadera tratados mediante hemiartroplastia de cadera. Nuestro objetivo es evaluar el efecto de la luxación de la prótesis de cadera (hemiartroplastia) como factor aislado, en la función de supervivencia de los pacientes.
Materiales y métodosRealizamos un estudio multicéntrico retrospectivo, que incluyó a 6.631 pacientes mayores de 65 años con fractura de cuello de fémur tratados quirúrgicamente mediante hemiartroplastia. Se realizaron cortes de seguimiento a los 30 días, 6 semanas, 90 días y un año del alta hospitalaria, determinando la tasa de luxación de cadera y la supervivencia de los pacientes.
ResultadosLa población femenina representó el 78,7%, y la edad media de la población fue de 85,2±6,7 años. La incidencia de luxación de la prótesis de cadera fue del 1,9% en los primeros 90 días tras el alta, lo que representa el 91,54% de las luxaciones primarias observadas anualmente. Se registró un aumento estadísticamente significativo de las tasas de mortalidad de los pacientes que presentaban al menos un evento de luxación de la prótesis de cadera (del 16,0 al 24,6% a los 90 días del alta, y del 29,5 al 44,7% al año), y también una disminución significativa de la función de supervivencia de los pacientes a los 90 días (p=0,016) y al año de seguimiento (p<0,001). Los eventos de luxación recurrente (26,15%) mostraron tasas de mortalidad aún más altas (hasta el 60,6%, p<0,001). El modelo multivariante de regresión de Cox determinó que la luxación de la prótesis de cadera es la única variable significativa (p=0,035) que afecta a la supervivencia de los pacientes, aumentando el riesgo de fallecer antes de un año de seguimiento en 2,7 veces.
DiscusiónNuestro estudio defiende que la luxación de la prótesis de cadera como factor aislado conlleva un mayor riesgo de muerte después de la hemiartroplastia por fractura de cadera en la población de edad avanzada.
Hip fracture is a very common reason for hospital admission in Trauma and Orthopedic department. It mainly involves the older population, in which its incidence remains high for the last decades.1
Displaced femoral neck fractures in older patients are surgically treated by osteosynthesis or hip arthroplasty.2–5 Hip arthroplasty allows the early load and walking ability, and avoids the osteosynthesis disadvantages, like the higher revision rates.6,7
However, hip arthroplasty for the treatment of femoral neck fracture is not exempted from potential complications. One of the most frequent complications of the hip prosthesis, in its two forms, partial prosthesis or total hip replacement, is dislocation.3,8
Despite it, hip prosthesis dislocation rates are between 1% and 6%.9–11 Indeed,the incidence of this complication could seem low, but its appearance frequently can involve the need for a revision. Many studies have analyzed risk factors for hip prosthesis dislocation, like the type of prosthesis,12 the surgical approach,13,14 or other inherent-to-patient risk factors (such as neurological disabilities)9; but there is a lack of updated information on the effect of dislocation on the survival of older hip fracture patients so treated by hip arthroplasty.3,8,11
This multicenter study aims to analyze the effect of hip hemiarthroplasty dislocation itself, as an isolated factor, on older hip fracture patients’ survival undergoing hemiarthroplasty.
Materials and methodsWe conducted a retrospective multicentre study including all femoral neck fracture cases over 65 years treated by hemiarthroplasty in two tertiary teaching hospitals and one secondary teaching hospital, between January 1, 2000, and December 31, 2019.
We included all patients over 65 with the main diagnosis of a femoral neck fracture, surgically treated by hip hemiarthroplasty. A total of 6331 patients treated by hip hemiarthroplasty for femoral neck fracture have been identified from the Minimum Basic Data Set (MBDS) codified by the Clinical Documentation Units following the ICD-9 (period from 2000 to 2016) and ICD-10 (period from 2016 to 2020) guidelines (100% codification rate). Hip fracture cases not surgically treated or surgically treated by osteosynthesis and THR were excluded.
The study registries included patients’ diagnosis, gender, age, time to surgery (TTS), and length of stay (LOS). Follow-up was determined until the patient's death or last hospital contact until December 2020. We made follow-up cut-offs 30-days after hospital discharge, 6 weeks, 90-days, and one year, determining hip dislocation rate and patients’ survival rate.
To analyze the effect on survival of variables other than dislocation, we performed a multivariate Cox regression model. Data were collected from the hospital with the highest number of hip fractures recorded between January 1, 2018, and December 31, 2019. The different comorbidities suffered by the patients, grouped into cardiac comorbidities, pulmonary comorbidities, renal comorbidities, digestive comorbidities, and tumor comorbidities, were collected; as well as the geriatric syndromes they present.
Statistical analysisExported data was analyzed by RStudio (v. 4.1.3) Qualitative variables were described by percentages and absolute count and analyzed by contingency tables. Statistical relevance was achieved by Chi-square tests. Quantitative variables were described by mean and standard deviation, and normality of sample distribution was defined by the Kolmogorov–Smirnoff test (Lilliefors corrected). We ascertain the statistically significant differences among groups by non-parametric tests. The cumulative patient survival analysis was performed by Kaplan–Meier tests and Cox regression with hazards ratio (HR) estimations with 95% confidence intervals. Group comparison by a factor on patient survival was estimated using the log-rank test. The analysis of confounding variables was carried out using a multivariate Cox regression model, previously performing a partial least-squares regression with cross-validation, using 10 random segments. A p-value ≤0.05 is the significance cut point.
EthicsThe present study has been approved by the Institutional Review Board (blinded for peer review), reference code: PI 2020 08 552.
ResultsOver the 20-year study period, 6331 older patients undergoing a hip fracture so-treated by hemiarthroplasty were included in the study. We registered a total of 130 (2.05%) patients suffering at lets one hip prosthesis dislocation episode during the first year of follow-up, and 26.15% (34/130) of them noted a recurrent hip prosthesis dislocation.
The women population represented 78.7% (4981 6331), and the mean age of the population was 85.2±6.7 years. The very-old population – over 80 years old – stood for 77.2% (4879/6331). The mean in-hospital length of stay (LOS) was 11.2±5.7 days, and the mean waiting time for surgery was 3.7±2.7 days. Within the first 24h after hospital admission, 5.9% (371/6331) of cases were surgically treated, reaching 14.5% (909/6331) within 48h after hospital admission.
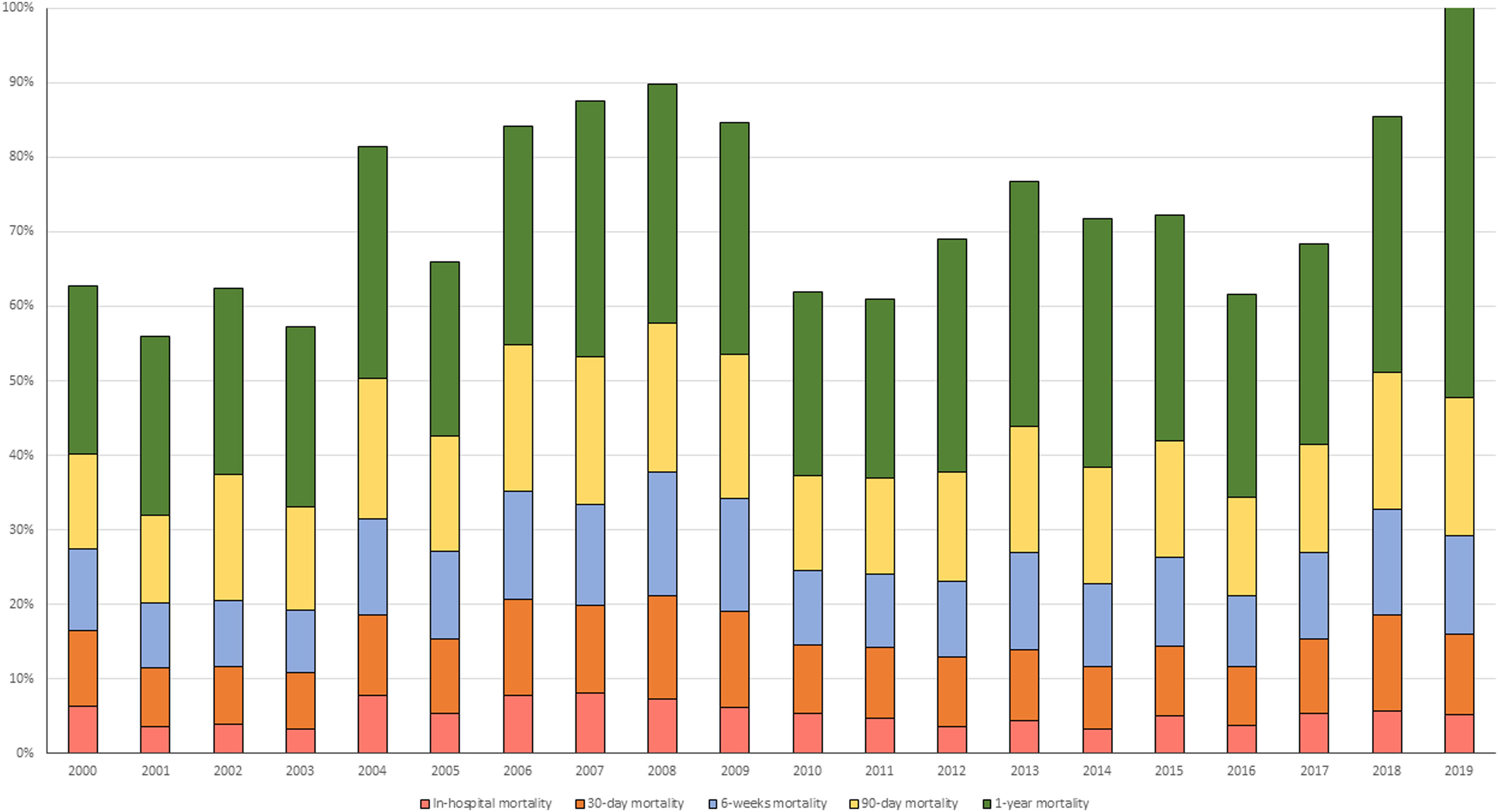
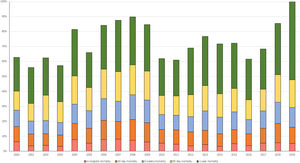
The in-hospital mortality rate was 5.2% (331/6331), and the 30-day mortality rate, 10.1% (605/6331). Six weeks after discharge the mortality rate reached 11.9% (694/6331), the 90-day mortality rate set at 16.0% (920/6331), and 29.5% (1600/6331) one year after hospital discharge. Yearly mortality rates over the 20 years covered by the study from early discharge to one-year follow-up are resumed in Fig. 1. We should bear in mind that the 2019 mortality rate after hip arthroplasty following a hip fracture would be influenced by the irruption of the Covid-19 pandemic during the yearly follow-up.
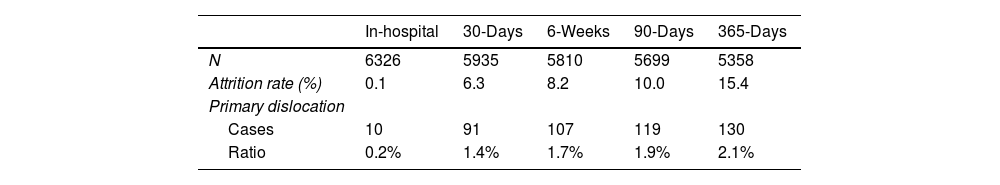
Table 1 shows the dislocation rates over the study period analyzed. It should be noted that 70.0% (91/130) of primary dislocations after arthroplasty for hip fracture detected yearly occurred within the first 30 days after hospital discharge, reaching 82.31% (107/130) in the first 6 weeks and 91.54% (119/130) in the first 90 days after hospital discharge.
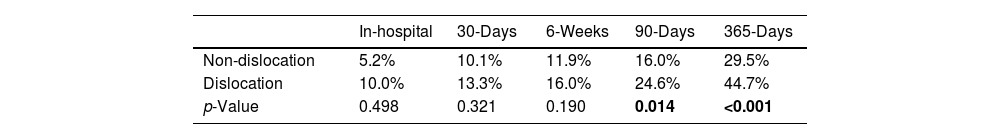
Mortality rates, from admission to one-year follow-up, regarding the hip prosthesis dislocation incidence are resumed in Table 2. We noted statistically significant increased mortality rates at both 90-day (p=0.014) and one-year (p<0.001) after hemiarthroplasty for femoral neck fracture patients presenting at least one episode of hip prosthesis dislocation. We also noted that for the 26.15% of patients (34/130) who suffered at least one further episode of hip prosthesis dislocation (recurrent dislocation) the mortality rate at one year reached 60.6% (p<0.001).
Mortality rates after hip fracture arthroplasty according to the hip prosthesis dislocation incidence.
| In-hospital | 30-Days | 6-Weeks | 90-Days | 365-Days | |
|---|---|---|---|---|---|
| Non-dislocation | 5.2% | 10.1% | 11.9% | 16.0% | 29.5% |
| Dislocation | 10.0% | 13.3% | 16.0% | 24.6% | 44.7% |
| p-Value | 0.498 | 0.321 | 0.190 | 0.014 | <0.001 |
Note: significant p-values are marked in bold.
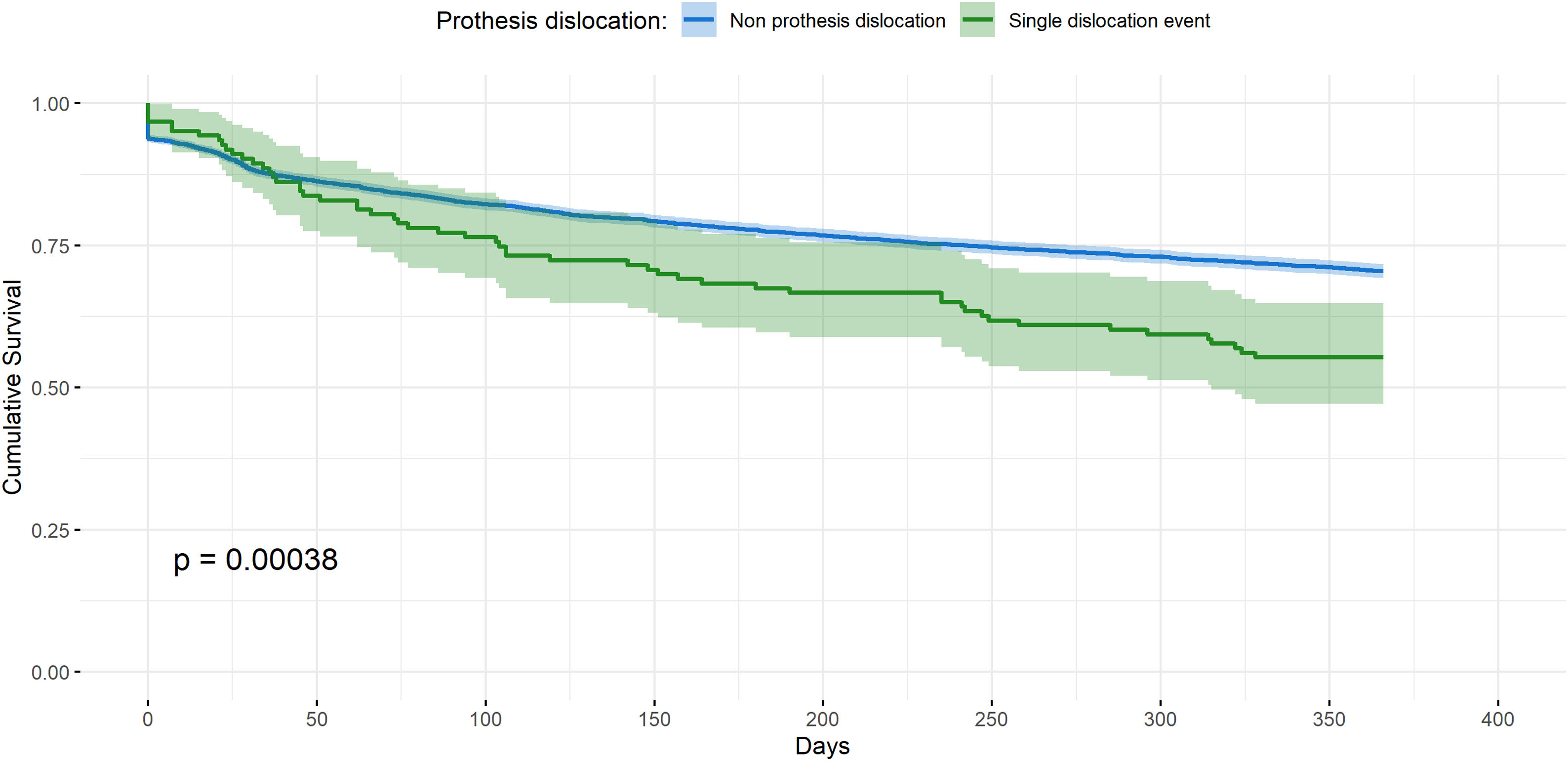
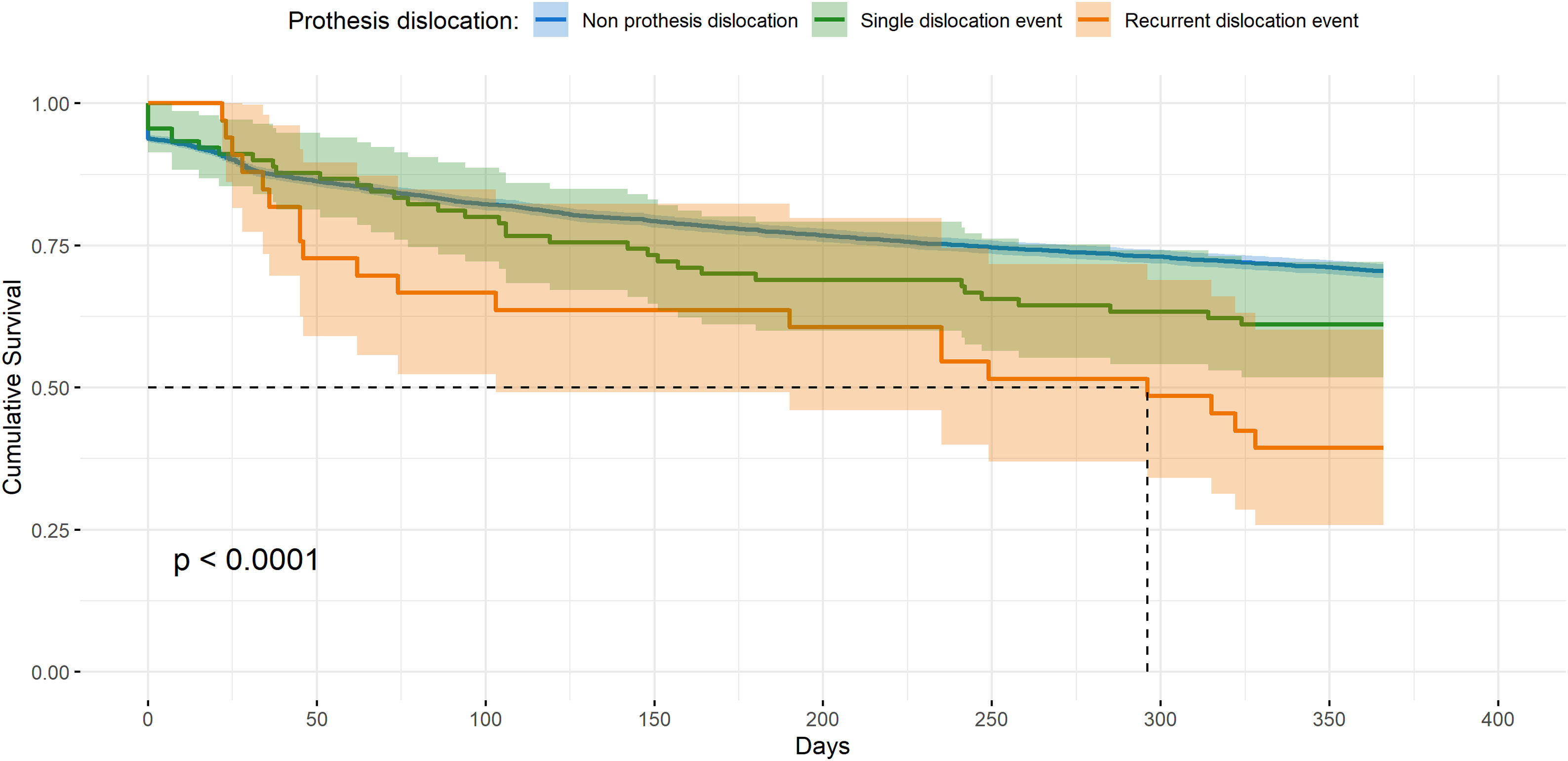
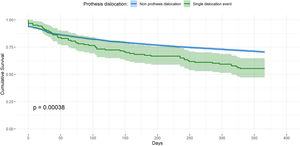
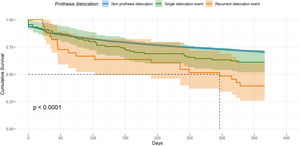
We also noted the cumulative patient survival for both dislocated and non-dislocated populations, attending the attrition rates. We noted statistically significant decreased patient survival function for hip prosthesis dislocation after hip fracture arthroplasty, Fig. 2, both in the 90-day follow-up the probability of survival is 75.44% (HR: 1.57 ? [1.079, 2.290], p=0.028), and at one-year follow-up, the probability of survival is 55.28% (HR: 1.62 ? [1.239, 2.121], p<0.001). This decreased patient survival noted was even lower for recurrent hip prosthesis dislocation population, both at 90-day follow-up (HR: 1.52 ? [1.168, 1.979], p=0.002) and at one-year follow-up (HR: 1.48 ? [1.229, 1.790], p<0.001), Fig. 3.
We further analyzed if demographic and stay-derived variables were noted to influence the hip prosthesis dislocation rate and therefore the increased mortality noted. We demonstrated that gender, LOS, and TTS do not influence the incidence of early hip prosthesis dislocation (over 90-day, follow-ups). However, we noted a discreet significant increase in the dislocation prosthesis incidence at 90-days for patients younger than 80 years old (p=0.050). We effectively verified that those demographic and stay-derived variables influenced the survival functions of hip fracture patients (p<0.050, in all cases), but the incidence of hip prosthesis dislocation, and therefore the increased mortality here noted, was not influenced by those potential confounding variables.
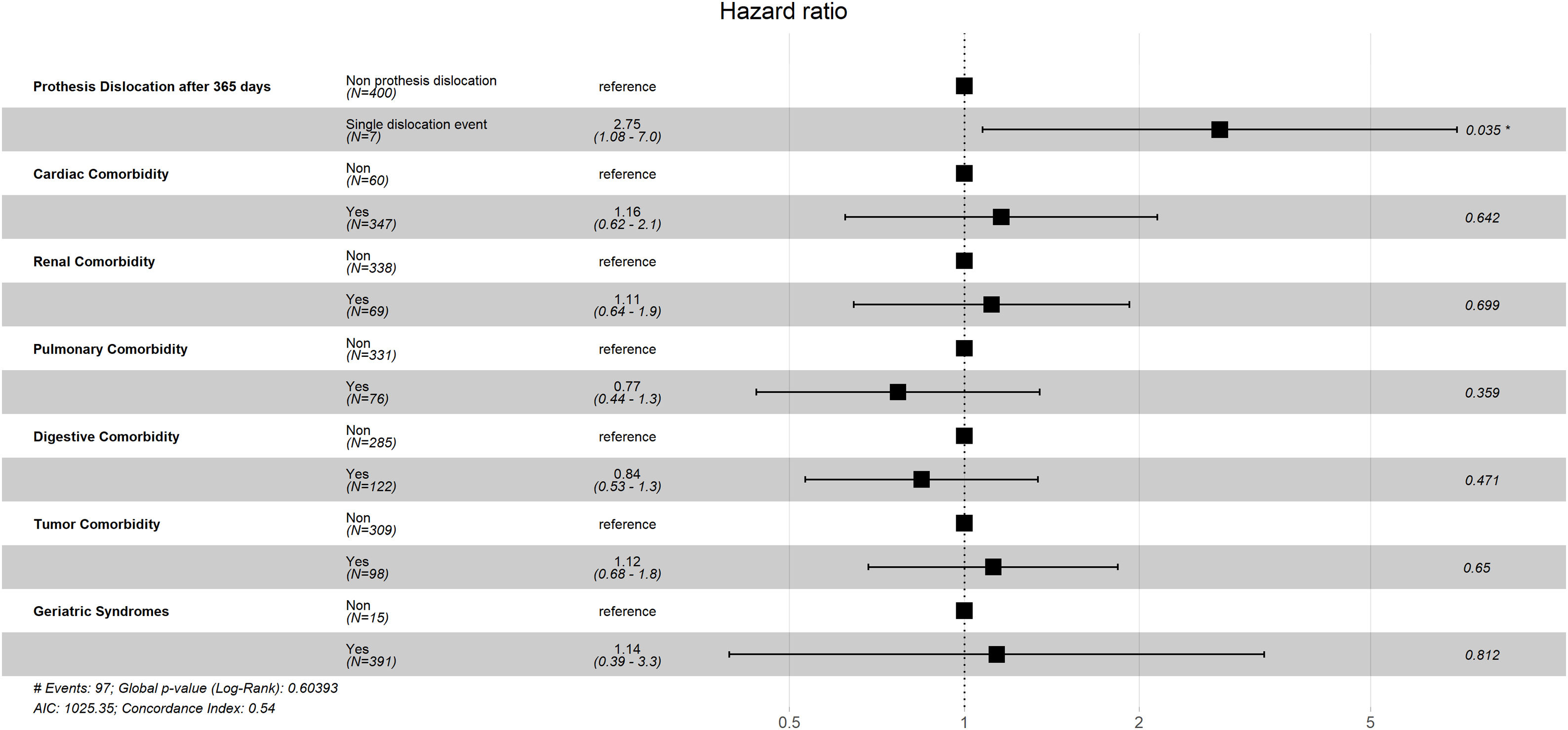
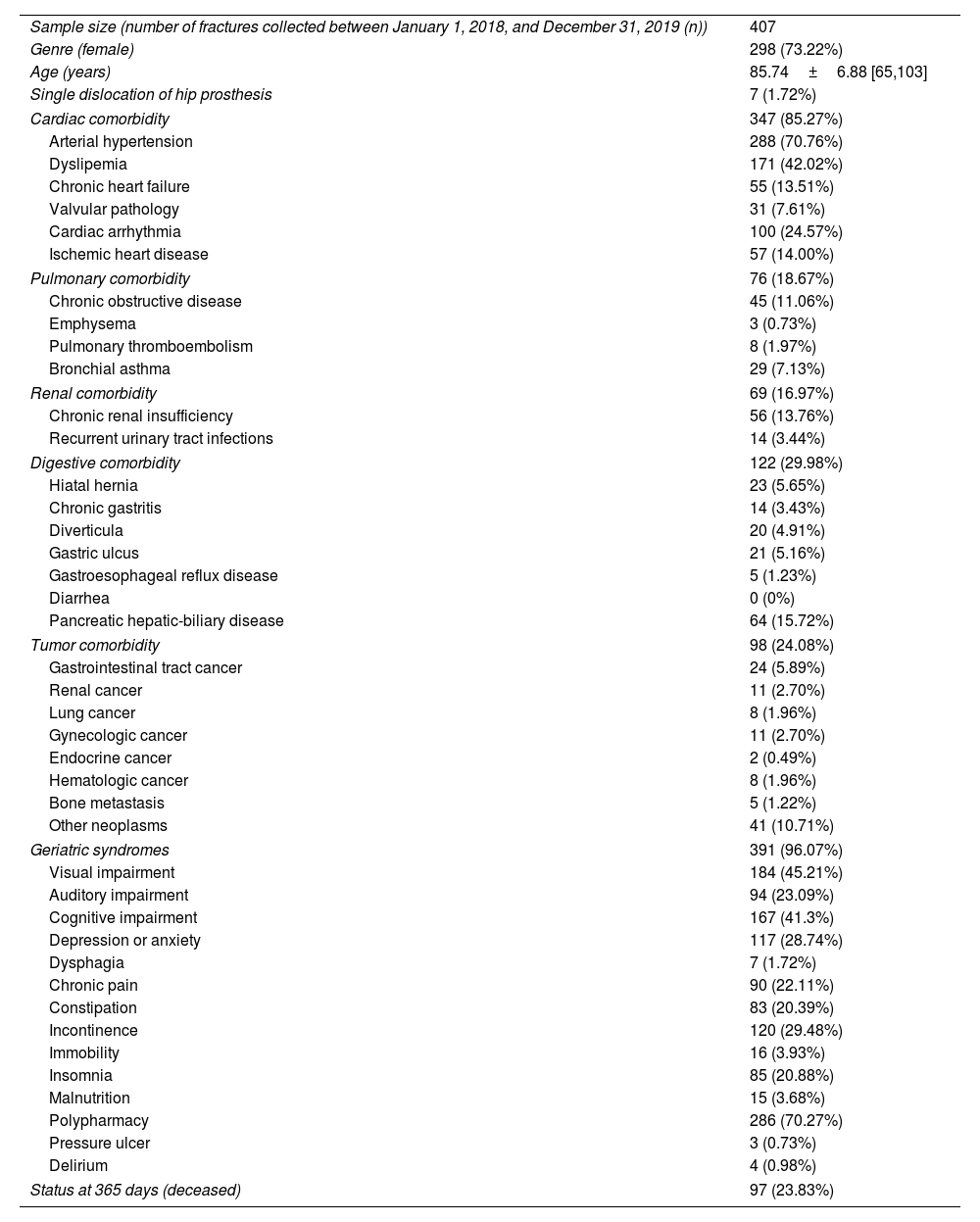
Finally, a multivariate Cox regression model was performed, the characteristics of the sample used in the model are shown in Table 3. Previously a partial least-squares regression was performed with cross-validation using 10 random segments, in which it was determined that a maximum of two variables would explain 64.22% of the variation in the response variable (mortality at one-year follow-up), and a single variable would explain 51.73% of the variation. In the multivariate Cox regression model performed (Fig. 4), it can be seen that the only significant variable that influences death at one year of follow-up is dislocation of the hip prosthesis, presenting the highest HR in comparison with other covariates (HR: 2.75 ? [1.08, 7.0], p=0.035).
Sociodemographic, and clinical characteristics of the sample taken from the hospital with the highest number of hip fractures recorded, between January 1, 2018, and December 31, 2019.
| Sample size (number of fractures collected between January 1, 2018, and December 31, 2019 (n)) | 407 |
| Genre (female) | 298 (73.22%) |
| Age (years) | 85.74±6.88 [65,103] |
| Single dislocation of hip prosthesis | 7 (1.72%) |
| Cardiac comorbidity | 347 (85.27%) |
| Arterial hypertension | 288 (70.76%) |
| Dyslipemia | 171 (42.02%) |
| Chronic heart failure | 55 (13.51%) |
| Valvular pathology | 31 (7.61%) |
| Cardiac arrhythmia | 100 (24.57%) |
| Ischemic heart disease | 57 (14.00%) |
| Pulmonary comorbidity | 76 (18.67%) |
| Chronic obstructive disease | 45 (11.06%) |
| Emphysema | 3 (0.73%) |
| Pulmonary thromboembolism | 8 (1.97%) |
| Bronchial asthma | 29 (7.13%) |
| Renal comorbidity | 69 (16.97%) |
| Chronic renal insufficiency | 56 (13.76%) |
| Recurrent urinary tract infections | 14 (3.44%) |
| Digestive comorbidity | 122 (29.98%) |
| Hiatal hernia | 23 (5.65%) |
| Chronic gastritis | 14 (3.43%) |
| Diverticula | 20 (4.91%) |
| Gastric ulcus | 21 (5.16%) |
| Gastroesophageal reflux disease | 5 (1.23%) |
| Diarrhea | 0 (0%) |
| Pancreatic hepatic-biliary disease | 64 (15.72%) |
| Tumor comorbidity | 98 (24.08%) |
| Gastrointestinal tract cancer | 24 (5.89%) |
| Renal cancer | 11 (2.70%) |
| Lung cancer | 8 (1.96%) |
| Gynecologic cancer | 11 (2.70%) |
| Endocrine cancer | 2 (0.49%) |
| Hematologic cancer | 8 (1.96%) |
| Bone metastasis | 5 (1.22%) |
| Other neoplasms | 41 (10.71%) |
| Geriatric syndromes | 391 (96.07%) |
| Visual impairment | 184 (45.21%) |
| Auditory impairment | 94 (23.09%) |
| Cognitive impairment | 167 (41.3%) |
| Depression or anxiety | 117 (28.74%) |
| Dysphagia | 7 (1.72%) |
| Chronic pain | 90 (22.11%) |
| Constipation | 83 (20.39%) |
| Incontinence | 120 (29.48%) |
| Immobility | 16 (3.93%) |
| Insomnia | 85 (20.88%) |
| Malnutrition | 15 (3.68%) |
| Polypharmacy | 286 (70.27%) |
| Pressure ulcer | 3 (0.73%) |
| Delirium | 4 (0.98%) |
| Status at 365 days (deceased) | 97 (23.83%) |
The most relevant finding of this work is the demonstration that the single hip prosthesis dislocation event, and recurrent hip prosthesis dislocations, are statistically associated as single, and isolated factors, with the survival function over the following year after surgery for a femoral neck fracture.
The mortality rates after hip fracture surgery in the older population have been widely studied. Currently, the advanced age, the male sex, a greater surgical delay, and the higher comorbidity rates are accepted and considered worldwide as risk factors for surgically treated hip fracture mortality.15 There is a consensus on arthroplasty as the most effective surgical treatment for older patients with displaced femoral neck fractures. Even so, in the last years, there is some controversy over which cases would be better to perform total hip replacement (THR) instead of hemiarthroplasty (HA),12,16–18 despite,HA uses to be the most performed surgical option.
The low incidence of hip prosthesis dislocation hinders to study of it as a risk factor for mortality after hip fracture surgery. The onset of this complication requires a reduction and often enlarges the in-hospital stay. In some cases, the instability and/or the recurrent dislocation also implies revision arthroplasty. However, slight information is available on the effect of the prosthesis dislocation event itself on the survival of older patients with displaced femoral neck fractures.
The prosthesis dislocation has been related to different risk factors, like the surgical approach, the surgical delay, or the patient's neurological status. Firstly, some studies analyzed inherent-to-patients risk factors for prosthesis dislocation, such as cognitive impairment, Parkinson's disease, and other neurological disabilities.9,10,14,19,20 Succeeding, other authors have investigated the role that the surgical approach and prosthesis components could have in the onset of prosthetic dislocation2,13,21–24 concluding that the posterior approach could be related to higher dislocation rates.25 Another previously defined risk factor for prosthesis dislocation has been the surgical delay. Salem et al.,26 discussed the increased risk of prosthesis dislocation with extended waiting time to surgery, while our results (exposing a longer waiting time to surgery) do not point to the same conclusion.
All out, hip prosthesis dislocation used to come in about 2% of cases10,11 and it mainly occurs within the first three months after surgery.9,11,19,26,27 Our results agree with these statements and therefore support them. Our noted prosthesis dislocation rate is on the usual margins. Our study stands for the fateful outcome related to hip prosthesis dislocation after hip fracture surgery, regardless of the demographic features of the patients. While previous studies11 only found statistically significant differences between cases of patients without dislocation and those with dislocation of the prosthesis who were treated by excisional arthroplasty. Here we show that the event of dislocation, as an isolated factor, after one year of follow-up after hip HA implies a lower survival and a higher risk of death.
Furthermore, we noted that recurrent hip prosthesis dislocation is a key risk factor for patients’ survival after hip fracture surgery, increasing the risk of death after 90 days of follow-up by 1.52 times. The incidence of recurrent hip prosthesis dislocation has been also previously set up to 80%.28 However, those results 28 should prudently be considered due to the high rate of failure on the original dislocation reduction; the authors reported a high number of cases finally treated by hip resection arthroplasty. Our results established recurrent hip prosthesis dislocation in approximately one-fourth of cases (26.15%, n=34/130).
Hip prosthesis dislocation not only stands for an excess in mortality but also has been associated with a poorer patient-reported quality of life.29 To prevent hip prosthesis dislocation events, hip fracture patients treated with arthroplasty are often prescribed the use of assistive devices, but those rehabilitation precautions do not improve the results.30 It all added up to point toward the convenience of taking appropriate preventive surgical initiatives.
The main message we denote is to give an evidence base to what has previously passed as “common practice”. We have to do our best to avoid prosthesis dislocation after a hip fracture surgery, as it is related to the worst prognosis. We have to be more careful performing the surgical technic to first properly choose the size of prosthesis components, and subsequently well-direct the components. Moreover, the demonstrated influence of the posterolateral approach on the onset of prosthesis dislocation, and thereby, the here denoted relationship between the prosthesis dislocation and the poorer prognosis of hip fracture patients, all evidences the recommendation to use anterior capsular approaches, including direct anterior approach or anterolateral approach in hip hemiarthroplasty for femoral neck fractures.
Nonetheless, our study also has some limitations, mainly intrinsic limitations due to its retrospective design. We did not analyze the implant model, surgical approach used, or other risk factors for prosthesis dislocation (as neurologic conditions).. The multivariate Cox regression model analysis showing the relationship between patient death and multiple factors. This study was carried out on a population sample (n=407), demonstrating that dislocation, as an independent factor, is related to a decrease in survival function of patients suffering from this complication. Although this sample is a small part of the study population, its size is larger than other sample sizes used by other authors.11 We did not aim to validate previous results on risk factors for hip prosthesis dislocation, but we report, for the first time, the unique and isolated relationship between the early prosthesis dislocation and the patient's survival.
Our study stands for the early hip prosthesis dislocation entailing a higher risk of death after hip fracture hemiarthroplasty in the older population. The hip prosthesis dislocation itself, and therefore the recurrent hip prosthesis dislocation, were associated in isolation with worsening survival function, from the first 90-days and one year after hospital discharge of older hip fracture patients.
Ethical approvalThe present study has been approved by the Institutional Review Board (CEIm Area de Salud de Salamanca), reference code: PI 2020 08 552.
FundingNone declared.
Competing interestThe authors have no conflicts of interest to declare that relevant to the content of this article.
Authors’ contributionsConception and design: JFB, CdaC; Data collection: MAGI, LGG, IBA, SS, MGA; Data analysis: CdaC, HF; Writing and editing: JFB, CdaC, HF.
All authors read and approved the final version of the manuscript.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
We would like to thank Dr. A. Guerra-González from Hospital Universitario El Bierzo, Marta Esteban and Dr. M. Fernández-González from Hospital Universitario de León, Dr. J. Alarcón from Hospital Nuestra señora de Sonsoles (Ávila), Dr. J.M. Perales from Hospital Universitario de Burgos, and Dr. H.J. Aguado from Hospital Clínico de Valladolid for their arrangements.