Early diagnosis of DDH, ultrasonography and treatment with Pavlik arnais have provided an improvement of the results. However, always appear children more than 3 months until 24-months old with late diagnosis or failure with Pavlik treatment requiring closed reduction and spica cast treatment as standard management.
Material and methodThe authors reviewed retrospectively DDH cases treated all patients treated with spica cast in human position during 3 months. The minimum follow-up was 5 years. It was considered good result when DDH reduced, remained stable, concentric, without AVN and not required surgery for sequels. All demographics, clinical and radiological parameters were statistically analyzed.
ResultsOf a total 152 hips were treated, 24 (15.8%) required surgery. In 6 cases (4%) was observed AVN. According IHDI/Tönnis displacement severity, types I and II were success treated in 98.9% and types III/IV in 64%. As bad prognosis factors were identified Ortolani test (+), alfa angle minor than 44°, acetabular index higher than 44° or IHDI/Tönnis types III/IV and factors for a good prognosis types I/II and the early recovery of the acetabular index more than 10° after 5 months of treatment. The age and early treatment of the patients was only important for the hips type III/IV (64 hips), the mean age of patients treated successfully was 5.1 months (64%), comparing with 8.8 months of the surgery group (36%). The incidence of AVN was 4% (6 cases) and in all cases the nucleus of ossification was not present in the X-ray pre-treatment. We cannot find relationship between AVN with previous skin traction, adductor tenotomy or severity of displacement.
ConclusionsConservative management of DDH with spica cast provide excellent results in almost all cases in types I and II hips (98.9%) and in 64% of types III/IV. An improvement of the acetabular index more than 10°, 5 months after the treatment is the best prognosis factor for a good result.
El diagnóstico precoz de la displasia del desarrollo de la cadera (DDC), la ultrasonografía y el tratamiento con el arnés de Pavlik han supuesto una mejora de los resultados. No obstante, siguen apareciendo casos de detección tardía, que sumados a aquellos en los que el arnés de Pavlik fracasó, nos encontremos con pacientes mayores de 3 meses con una DDC. En estas situaciones en las que fracasó el arnés de Pavlik u otros dispositivos ortopédicos y, hasta los 24 meses de edad, la reducción cerrada e inmovilización con yeso pelvipédico sigue siendo el tratamiento de elección.
ObjetivoEvaluar el tratamiento de la DDC en los niños mayores de 3 meses, en los que se les realizó reducción cerrada bajo anestesia general, artrografía y posterior inmovilización con yeso pelvipédico durante 3 meses, analizándose los resultados y los factores pronóstico de riesgo clínicos y/o radiológicos.
Material y métodoSe revisan los casos tratados de DDC con yeso pelvipédico. La duración media de la inmovilización fue de 3 meses. Se consideraron buenos resultados cuando tras 5 años de seguimiento, la cadera se encontraba reducida, era estable, concéntrica, sin signos de necrosis avascular (NAV), no habían requerido cirugía para el tratamiento. Se analizaron estadísticamente los datos demográficos, clínicos y radiológicos de los pacientes.
ResultadosDe las 152 caderas tratadas, 24 requirieron cirugía adicional (15,8%) y 6 presentaron NAV (4%). Según la clasificación IHDI/Tönnis, las caderas tipos I y II fueron tratadas con éxito el 98,9%, comparado con el 64% de las tipos III/IV. Se consideraron factores de mal pronóstico el grado III/IV, casos que al nacimiento presentaron test de Ortolani (+), ángulo alfa menor de 44°, o un índice acetabular mayor de 44° previo a la colocación del yeso pelvipédico. Se consideraron factores de buen pronostico las caderas tipo I (displasia acetabular) o tipo II (subluxación), o una mejora de >10° del índice acetabular 5 meses tras la colocación del primer yeso. La edad a la hora de iniciar el tratamiento no tuvo significación estadística cuando se estudió globalmente, aunque sí fue significativa en el grupo de 64 caderas tipos III/V. Las 41 caderas (64%) que no precisaron tratamiento quirúrgico presentaban una edad media de 5,1 meses, mientras los que requirieron tratamiento quirúrgico, 23 caderas (36%), la edad fue 8,8 meses. La incidencia de NAV fue del 4% (6 casos), y en todos ellos el núcleo de osificación no estaba presente al inicio del tratamiento. No se observó relación con la gravedad de desplazamiento, tracción previa o tenotomía de adductores.
ConclusionesLa reducción cerrada e inmovilización con yesos pelvipédicos proporciona una tasa de éxito cercana al 100% en las caderas tipos I y II, y del 64% en las caderas tipos III/IV. En este subgrupo de casos es donde hay que ser mas exigente para instaurar el tratamiento precoz, antes de los 6 meses. La mejoría radiológica del índice acetabular >10° en los primeros 5 meses es el factor pronóstico mas favorable para evitar la cirugía en los años siguientes.
Regardless of the timing or method used for treatment of developmental dysplasia of the hip (DDH), whether conservative or surgical, our goal is to achieve stable, concentric reduction without altering vascularisation or growth, allowing the proximal femur and acetabulum to develop properly and preventing deformities and degenerative phenomena in the future.1,2
Early clinical diagnosis based on neonatal examination and that performed by the paediatrician during the first trimester of life, the decades-long use of ultrasonography, and the widespread use of Pavlik harness treatment have led to undeniable improvements in the diagnosis and treatment of newborns and infants under six months of age with DDH, as reflected in numerous publications.2,3
At our centre, the hips of newborns are routinely examined within the first two days after birth. Those identified as being at risk are examined again in a specialist consultation with a paediatric orthopaedic surgeon and undergo an ultrasound scan of their hips.
However, despite the aforementioned advances, cases of late detection (>4 months – Ortolani –) continue to occur. When these cases are added to those in which the Pavlik harness was not as successful as expected, we find ourselves treating patients over 2 months old with DDH. In these situations, up to the age of 24 months, closed reduction and immobilisation with a spica cast remains the preferred treatment. There are few references to this treatment in the literature and success rates vary widely.4–8
This study aims to evaluate the treatment of DDH in children over 3 months old due to late diagnosis or failure of initial Pavlik harness treatment. The study will analyse the results of arthrography, closed reduction, and subsequent immobilisation with a spica cast performed under general anaesthesia, as well as clinical and/or radiological prognostic risk factors.
Material and methodsOf a total of 149 patients (197 hips), a retrospective review was conducted of 121 patients (152 hips) diagnosed with DDH who underwent arthrography, closed reduction, and spica cast placement in the ‘human position’ following the same treatment protocol between 2003 and 2020, both years included, with informed consent accepted.
Forty-five hips that required open reduction after arthrography (16 cases) and patients with less than 4 years of follow-up (9 cases) were excluded from the study. Twenty cases presenting with neurological disease and/or psychomotor disorder,9 arthrogryposis, or other syndromic conditions, or with postoperative CT scans showing irreducibility or re-dislocation requiring open reduction, were also excluded from the study.
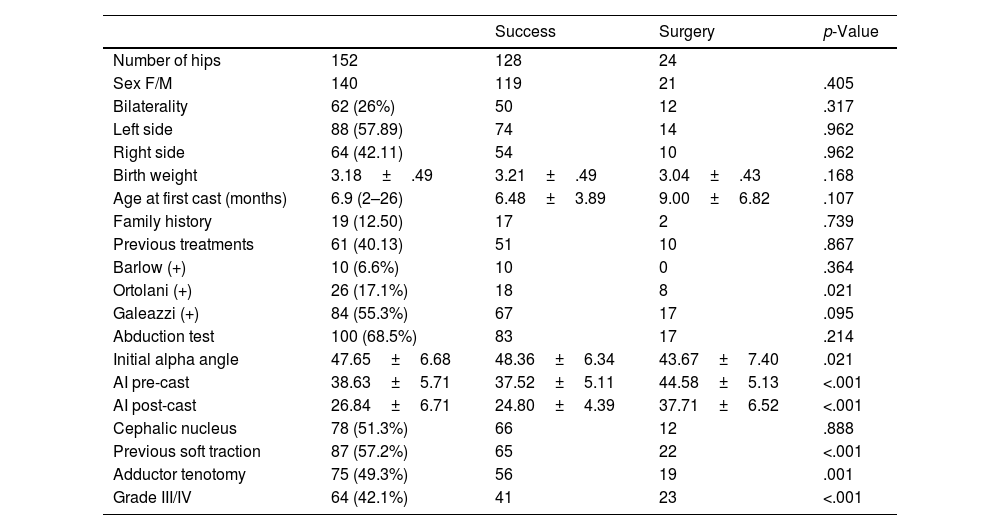
Demographic and clinical data were collected, such as family history, age, sex, birth weight, type of delivery, laterality, and degree of displacement (Table 1). In patients who underwent ultrasound, the alpha angle was quantified in the first study. In the anteroposterior radiograph of the hips, prior to treatment, the presence of cephalic nuclei and their position according to the Tönnis classification10 were recorded if they were visible; if they were not visible, the classification of the International Hip Dysplasia Institute (IHDI) was used.11 The evolution of the acetabular index (AI) was assessed before treatment, 5 months after the start of treatment, and at the last check-up. CE angle of Wiberg was also quantified at time of discharge or indication for surgery. Diagnosed cases of AVN were analysed to determine whether they were related to the degree of displacement, the use or non-use of traction prior to the application of the first spica cast, adductor tenotomy, previous treatment, or the presence of an ossification nucleus. Radiological measurements were performed by 3 unit staff members.
Clinical and radiological characteristics of the hips based on whether or not they required surgery after orthopaedic treatment.
| Success | Surgery | p-Value | ||
|---|---|---|---|---|
| Number of hips | 152 | 128 | 24 | |
| Sex F/M | 140 | 119 | 21 | .405 |
| Bilaterality | 62 (26%) | 50 | 12 | .317 |
| Left side | 88 (57.89) | 74 | 14 | .962 |
| Right side | 64 (42.11) | 54 | 10 | .962 |
| Birth weight | 3.18±.49 | 3.21±.49 | 3.04±.43 | .168 |
| Age at first cast (months) | 6.9 (2–26) | 6.48±3.89 | 9.00±6.82 | .107 |
| Family history | 19 (12.50) | 17 | 2 | .739 |
| Previous treatments | 61 (40.13) | 51 | 10 | .867 |
| Barlow (+) | 10 (6.6%) | 10 | 0 | .364 |
| Ortolani (+) | 26 (17.1%) | 18 | 8 | .021 |
| Galeazzi (+) | 84 (55.3%) | 67 | 17 | .095 |
| Abduction test | 100 (68.5%) | 83 | 17 | .214 |
| Initial alpha angle | 47.65±6.68 | 48.36±6.34 | 43.67±7.40 | .021 |
| AI pre-cast | 38.63±5.71 | 37.52±5.11 | 44.58±5.13 | <.001 |
| AI post-cast | 26.84±6.71 | 24.80±4.39 | 37.71±6.52 | <.001 |
| Cephalic nucleus | 78 (51.3%) | 66 | 12 | .888 |
| Previous soft traction | 87 (57.2%) | 65 | 22 | <.001 |
| Adductor tenotomy | 75 (49.3%) | 56 | 19 | .001 |
| Grade III/IV | 64 (42.1%) | 41 | 23 | <.001 |
AI: acetabular index.
Under general anaesthesia and radioscopic control, arthrography was performed by inserting the needle below the long adductor tendon while the hip was flexed and abducted. Then, 3–5cm3 of a 30%–40% diluted iodinated contrast medium was injected to allow visualisation of any impediments to adequate reduction and to assess the shape of the femoral head and the stability of the hip in relation to the degrees of abduction according to the Ramsey test.12,13
According to the contrast medium pooling in the acetabulum, arthrographies were classified as reduced hips, docking hips, or non-reduced hips.14 The latter two arthrographic categories were excluded from the study. In cases with a reduced Ramsey arc (<25°), an open or percutaneous adductor tenotomy was performed.
The spica cast was applied in human position (100°–110° of flexion and 30°–50° of abduction)15 after the patient was placed in a pelvic frame by one of the 4 members of our paediatric orthopaedic trauma unit. For IHDI or Tönnis type III–IV hips, a control CT scan was performed 1–2h after applying the cast to assess the position of the femoral head in relation to the acetabulum; hips that remained dislocated were excluded from the study. Immobilisation with spica cast took 3 months (range: 2.6–4.6), with changes made every 5 weeks under general anaesthesia. Following removal of the final cast, 76 hips (50%), including some type II and all type III–IV hips, were fitted with a full-time or night-time thermoplastic abduction splint for an additional 3 months.
Patients were followed up clinically and radiologically on an outpatient basis every three months during the first year after completing treatment and subsequently annually until clinical discharge or if surgery were indicated to treat residual acetabular dysplasia or associated femoral deformity.
A good treatment outcome was considered to be when the patient was discharged without sequelae, with a concentric hip, well covered, without physeal injury, without AVN, and with an AI of less than 22° at 4–5 years of age or at time of discharge. Poor outcomes were considered when further surgical treatment was required.1
The collected data were analysed statistically. Qualitative variables are presented as numbers and percentages, and quantitative variables are expressed as the mean±standard deviation. Differences between groups were analysed using the χ2 test or Fisher's exact test, where appropriate, for qualitative variables and the non-parametric Mann–Whitney U test (two-sample Wilcoxon rank-sum test) for quantitative variables. A multivariate logistic regression model was adjusted using a backward stepwise procedure to determine the predictors of the need for surgery after treatment. Initially, the logistic regression model included variables that were significant in the univariate analysis (those with a p-value <.100).
ResultsOf a total of 149 patients (197 hips), 152 hips with DDH were analysed in 121 patients (31 bilateral, 26% of patients) who met the criteria for the study. The mean follow-up time was 5.1 years (range: 4–11). The left side was affected in 88 cases (58%) and the right side in 64 (42%). In terms of gender, 110 were female and 11 were male (10:1). The mean birth weight was 3.18kg (range: 2.30–4.52). There was a family history of DDH in 19 patients (12.5%). The Pavlik harness or thermoplastic abduction splint was used previously in 61 cases (40%). Diagnosis was delayed (after 3 months) in 57% of cases.
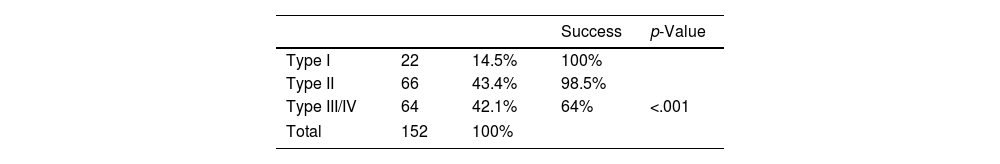
Patients were grouped according to the degree of displacement, using the IHDI and Tönnis classifications as a reference4,5: type I dysplastic hips, 22 cases (14.5%); type II subluxated hips, 66 cases (43.4%); and type III/IV dislocated hips, 64 cases (42.1%).
Gentle traction at the zenith and progressive abduction were used in 87 cases (57.2%) for an average of 9 days (range: 5–20) prior to closed reduction and immobilisation with spica cast. The mean age at which closed reduction and the initial plaster cast application were performed was 6.9 months (range: 2–26), and the mean duration of immobilisation was 3.2 months (range: 2–5).
In the radiograph prior to closed reduction, the ossification nucleus was present in 51.3% of cases (78/152). The mean AI prior to treatment was 38.6° (range: 25–51). In cases where an ultrasound study was available (79 hips), the mean initial alpha angle was 47.6° (range: 34–63). In 75 hips (49.3%), adductor tenotomy was performed to increase the Ramsey safe arc of motion.
Overall, plaster cast treatment was successful in 84.2% (128 hips) and 15.8% (24 hips) required subsequent surgery. We found a statistically significant relationship (p<.05) between poor outcomes and patients who had an Ortolani (+) at birth, an alpha angle of less than 44°, a pre-treatment AI of greater than 44°, and a Tönnis/IHDI displacement grade of III/IV. We found no correlation between good outcomes and prior use of traction, adductor tenotomy, the presence of ossification nuclei, or the placement of a posterior abduction splint after treatment with spica cast.
Regarding the timing of treatment initiation, 79 hips (52%) were treated before 6 months of age, with no significant overall differences observed compared to those treated later. We also observed no differences in the success rate in terms of sex, laterality, bilaterality, family history, or hips that had been previously treated with a Pavlik harness or thermoplastic abduction splint.
The initial alpha angle in hips that did not require secondary surgery was 48.4°, while in those that required subsequent surgery it was 43.7°, with statistically significant differences (p<.05). The mean initial AI of hips that did not require surgery was 37.5°, compared to 44.6° for those that did require surgical treatment, also showing statistical significance (p<.05).
With regard to the type and degree of displacement (Table 2), dysplastic or subluxated hips (Tönnis/IHDI types I and II) had better outcomes. No type I cases and only one (1.5%) type II case required additional pelvic surgery, compared with 36% (23 cases) of the type III/IV hip cases that required pelvic/femoral surgery with or without open reduction (p<.001). Tönnis/IHDI type I and II hips had a success rate of 98.9% of cases compared to 64% for type III/IV hips.
The mean improvement in AI observed before and after spica cast placement was 11.8° over a mean period of 5 months. In cases where secondary surgery was avoided, the improvement was 12.7°, while in those that required surgery, it was only 6.9°, which was statistically significant (p<.05). The mean final AI was 20.2°. The mean centre-edge angle of Wiberg at the end of follow-up was 25°.
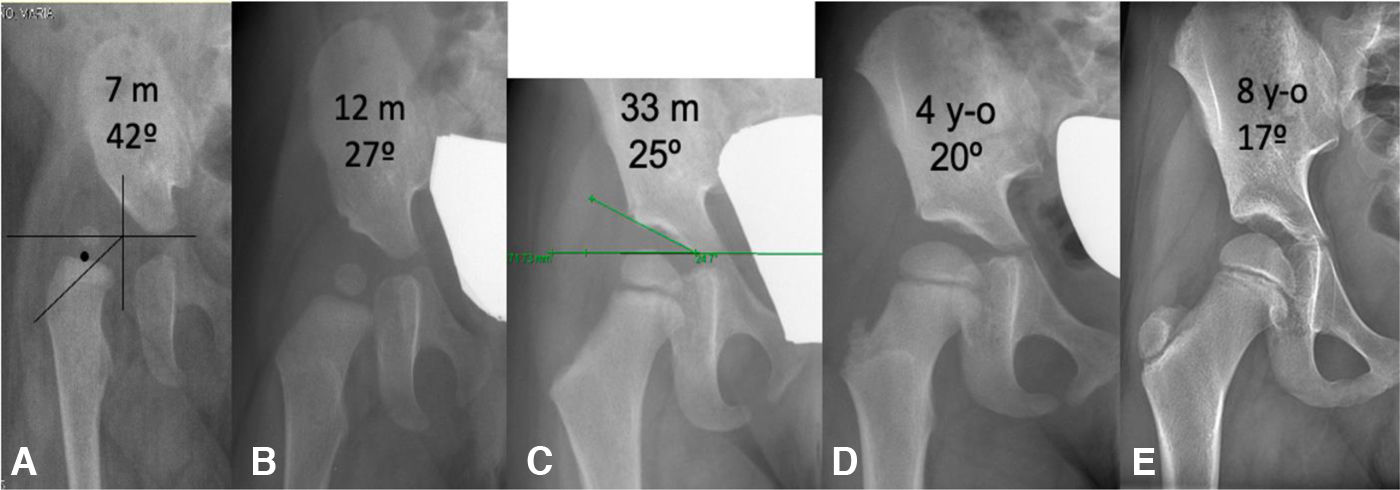
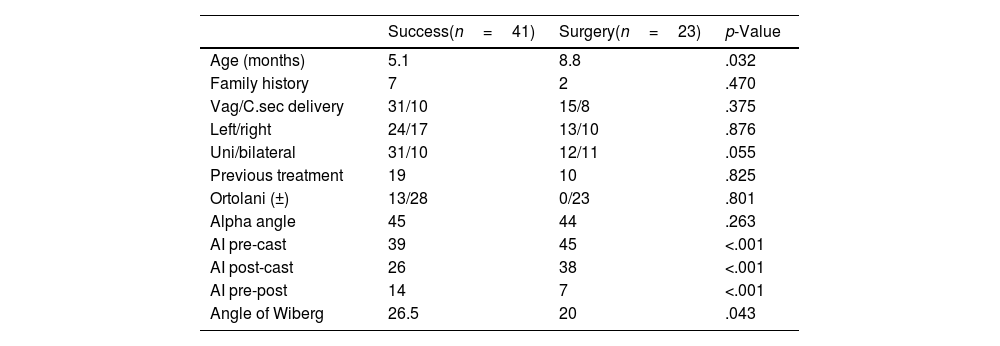
If we analyse only the type III/IV hips (64 cases) (Table 3), we find that, in this group, there are significant differences in age at the time of treatment initiation (p<.05). The 41 cases (64%) that did not require surgical treatment had a mean age of 5.1 months, while those that required surgical treatment had a mean age of 8.8 months. With regard to the previous AI, the successfully treated hips had an AI of 39.5° compared to 44.7° for those that required surgery. Five months after the first cast was applied, the angle was 25.6°, compared to 38°, and the final AI was 18°, compared to an average of 28° for the 23 hips that were treated surgically. There was also a significant improvement of 12° in the 5-month period after the first cast was applied, compared to only 6.7° in the AI of hips that required surgery, with no cases reaching 10° (Fig. 1).
Prognostic factors type III/IV hips (n=64).
| Success(n=41) | Surgery(n=23) | p-Value | |
|---|---|---|---|
| Age (months) | 5.1 | 8.8 | .032 |
| Family history | 7 | 2 | .470 |
| Vag/C.sec delivery | 31/10 | 15/8 | .375 |
| Left/right | 24/17 | 13/10 | .876 |
| Uni/bilateral | 31/10 | 12/11 | .055 |
| Previous treatment | 19 | 10 | .825 |
| Ortolani (±) | 13/28 | 0/23 | .801 |
| Alpha angle | 45 | 44 | .263 |
| AI pre-cast | 39 | 45 | <.001 |
| AI post-cast | 26 | 38 | <.001 |
| AI pre-post | 14 | 7 | <.001 |
| Angle of Wiberg | 26.5 | 20 | .043 |
AI: acetabular index; Vag/C.sec: vaginal delivery/caesarean section.
(A) Girl aged 7 months. Right type 3 DDH with acetabular index of 42°. (B) Follow-up 5 months after cast placement showing a reduced hip and rapid improvement in the acetabular index of 15° after treatment. (C–E) Radiological progression up to 8 years of age with stable, centred hip and normalised radiological parameters.
With regard to adductor tenotomy (49% of cases), prior use of soft traction (57%), presence of the ossification nucleus (51%), or placement of a full-time or part-time thermoplastic abduction splint (50%) after removal of the last spica cast, we found no statistical significance for treatment success or avoidance of subsequent surgery.
AVN appeared in 6 of the 152 (3.9%) hips during follow-up according to the criteria of Salter et al.15 and Burgos et al.16 In none of these cases was the ossification nucleus present prior to closed reduction (p<.05). Neither did we observe that the application of traction prior to reduction, performance of an adductor tenotomy, or prior treatment with a Pavlik harness or other device was related to the onset or development of AVN or the degree of displacement. Of the six AVN cases diagnosed, three corresponded to Tönnis/IHDI type III, one to type II, and two to type I.
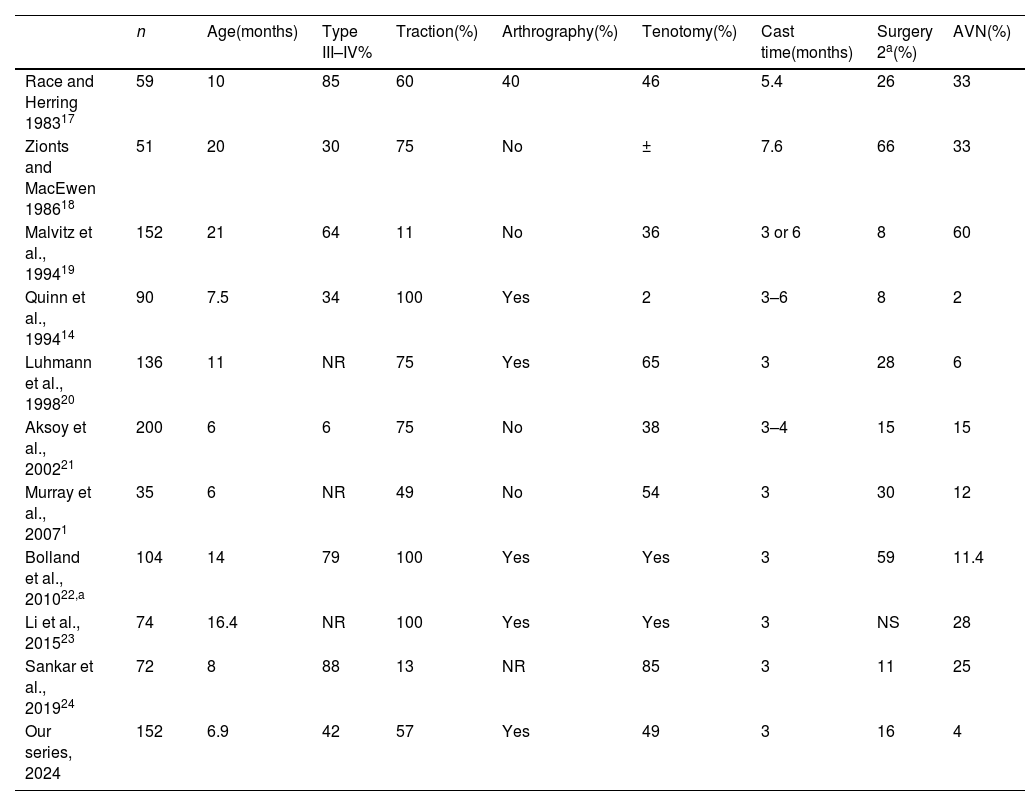
DiscussionClosed reduction and immobilisation with a spica cast is the treatment of choice for late-onset DDH, between 4 and 24 months, or after failure of treatment with a Pavlik harness or other devices.6–8 Its use has been widely accepted for decades, but the literature contains a wide variety of classic pre-ultrasound and/or pre-Pavlik studies. There is great variability in the duration of immobilisation and different criteria for analysing the results. Not all authors apply the same treatment protocol, including the need or not for arthrography for decision-making. Some studies are old, with a high mean age of patients, and the results obtained are assessed according to different criteria. Basically, two conditions characterise a poor outcome and do not necessarily go together: AVN and/or the need for additional surgery to improve congruence and/or residual dysplasia to avoid degenerative changes and a painful hip in the medium to long term (Table 4).1,14,17–24
Comparison with other series in the literature.
| n | Age(months) | Type III–IV% | Traction(%) | Arthrography(%) | Tenotomy(%) | Cast time(months) | Surgery 2a(%) | AVN(%) | |
|---|---|---|---|---|---|---|---|---|---|
| Race and Herring 198317 | 59 | 10 | 85 | 60 | 40 | 46 | 5.4 | 26 | 33 |
| Zionts and MacEwen 198618 | 51 | 20 | 30 | 75 | No | ± | 7.6 | 66 | 33 |
| Malvitz et al., 199419 | 152 | 21 | 64 | 11 | No | 36 | 3 or 6 | 8 | 60 |
| Quinn et al., 199414 | 90 | 7.5 | 34 | 100 | Yes | 2 | 3–6 | 8 | 2 |
| Luhmann et al., 199820 | 136 | 11 | NR | 75 | Yes | 65 | 3 | 28 | 6 |
| Aksoy et al., 200221 | 200 | 6 | 6 | 75 | No | 38 | 3–4 | 15 | 15 |
| Murray et al., 20071 | 35 | 6 | NR | 49 | No | 54 | 3 | 30 | 12 |
| Bolland et al., 201022,a | 104 | 14 | 79 | 100 | Yes | Yes | 3 | 59 | 11.4 |
| Li et al., 201523 | 74 | 16.4 | NR | 100 | Yes | Yes | 3 | NS | 28 |
| Sankar et al., 201924 | 72 | 8 | 88 | 13 | NR | 85 | 3 | 11 | 25 |
| Our series, 2024 | 152 | 6.9 | 42 | 57 | Yes | 49 | 3 | 16 | 4 |
AVN: avascular necrosis; n: number of cases; NR: not recorded.
The classic method of grading the severity of displacement is that proposed by Tönnis in 4 groups,10 with types 3 and 4 being the most severe. However, this classification is difficult to apply in cases where the ossification nucleus is not yet radiologically visible. For this reason, the IHDI proposed a new classification using the relationship between the metaphyseal midpoint of the proximal femur and the Hilgenreiner line, unlike the classification proposed by Tönnis, which uses the centre of the ossification nucleus with a horizontal line passing through the superolateral acetabular rim.11 Both classifications can be useful and are not mutually exclusive, and were complementary and equivalent when reviewing our collected cases.
Furthermore, the distinction between what constitutes a good or poor outcome after treatment is also unclear. Although most authors agree that good outcomes are those in which a reduced, concentric, stable hip is achieved and in which the joint elements grow harmoniously and symmetrically with respect to the healthy contralateral side without requiring further surgical treatment,1 this condition does not take into account the sequelae caused by an AVN that does not alter the sphericity or stability of the hip but can cause a discrepancy in limb length, relative trochanteric overgrowth, or joint degeneration decades after treating a DDH, which may require additional surgeries unrelated to joint congruence.14
In our series, 15.8% of patients required secondary surgery. This falls within the wide range of poor outcomes reported in the literature, between 8% and 66% (Table 4). The authors attribute the need for secondary surgery to two factors: the degree of displacement and the patient's advanced age, which are related to late diagnosis and treatment. Fifty-eight per cent of the hips treated in our series were IHDI types I and II, which are associated with better long-term outcomes. Furthermore, 66.6% of the hips were treated before six months of age. In other words, the young age at which the spica casts were applied in our series accounts for a high percentage of cases, as diagnosis occurs earlier than it did decades ago when neonatal screening and ultrasound diagnosis programmes had not yet been developed. However, we cannot be satisfied with this data, as a significant proportion of our cases were diagnosed late (57% were over 3 months old), which requires improvement in the early detection protocols of our healthcare setting.
The age factor is clearly reflected in the historical series by Malvitz and Weinstein19 of cases treated between 1938 and 1969, with an average follow-up of 30 years. The average age of their patients was 21 months, and they observed a better prognosis in cases treated before 6 months of age. In the series by Quinn et al.14 only 7.7% required surgical treatment, attributable to the fact that 79% were treated before 6 months of age. Similarly, Li et al.23 observed better AI improvement rate in children under 12 months than in those over 18 months and Zionts and MacEwen,18 treating patients aged between one and three years, found that 66% required secondary surgical treatment. Similarly, Bolland et al.22 treated 104 hips and observed that 58% required secondary surgery, finding statistically significant differences between those hips treated at over 18 months of age. In our series, overall, age was not statistically significant, although when we analysed the most severe forms of displacement (grades III and IV), age was statistically significant. The age of the hips treated successfully was 5.1 months compared to 8.8 months for the hips that required surgery.
The degree of displacement prior to orthopaedic reduction is possibly the most important prognostic factor. Like Lerman et al.,4 who found that the failure rate was higher when using the Pavlik harness to treat Ortolani + patients, we have also found that those with true dislocation (types III or IV IHDI, Galeazzi +) have a worse prognosis. Aksoy et al.21 published one of the largest series of closed reduction and spica cast immobilisation. Of the 200 hips treated, 15% required secondary surgical treatment and statistical significance was found (p<.05) depending on the hip's position according to the Tönnis classification.10 Sankar et al.24 observed that 11% of the 72 hips treated in their study required surgery, the vast majority (88%) of which corresponded to Tönnis grades III and IV and were in children older than six month. Bolland et al.22 observed that 58% of the 104 treated hips required secondary surgery, 37.5% of which corresponded to grades III–IV.
Therefore, it is in the most severe cases that we must verify the quality of the reduction obtained. This emphasises the importance of arthrography in confirming the absence of soft tissue interposition and achieving correct reduction. Race and Herring17 examined 59 hips, 26% of which required further surgery, and 33% of which developed AVN. For Forlin et al.,25 the quality of reduction is the most important prognostic factor. While not all authors consider it particularly useful, Zionts and McEwen18 place greater value on clinical signs of stability after reduction. We consider arthrography to be an essential tool as it enables us to observe the reduction achieved, assess stability, determine whether the labrum is inverted or interposed, and establish whether the reduction is concentric or if there is excessive medial dye pool.13,14,25–27 However, in hips with marked instability, it is advisable to check that the reduction remains in the correct position after placing the spica cast, even if we observe adequate reduction. To do this, we perform a CT scan a few hours after placing the cast, while the patient is still sedated. Ideally, an MRI scan or inguinal ultrasound scan should be performed to check the reduction is correct, although we have no experience of using these techniques.28
AVN is arguably the most serious and unpredictable complication that can overshadow successful treatment. Some authors believe that the presence of the ossification nucleus acts as a protective factor against AVN.29 Luhmann et al.20 analysed 153 hips with DDH and found that 5.8% developed AVN. They found no statistical significance regarding the protective value of the ossified nucleus. The use of traction prior to reduction has also been linked to preventing AVN. Of the six cases of AVN that we observed (3.9%), three were Tönnis type III, one type II, and two type I; in none of these cases was the nucleus visible at the start of treatment. Although the incidence of AVN in our study was too low (six cases) to draw irrefutable conclusions, we feel more confident about starting treatment when the nucleus is present. Li et al.30 evaluated pre-reduction traction in 432 hips in patients aged over six months (54% Tönnis types III–IV). They observed 61 cases of AVN (14.1%) and concluded that hips treated with pre-reduction traction did not show better results.
Progression of the AI is the most common radiological parameter measured during short- and medium-term periodic check-ups. However, this index has no prognostic value when taken in isolation and without considering the position of the cephalic nucleus. Once the hip is reduced and stabilised with a healthy epiphyseal nucleus, normalisation of the AI is the most important radiological data and usually forms the basis for indicating pelvic surgery due to residual acetabular dysplasia, with or without femoral osteotomy. Pelvic surgery was only necessary in one case of types 1 and 2 hips in our series (88 cases). By contrast, 23 out of 64 cases of types 3 and 4 (36%) required surgical treatment (pelvic and/or femoral osteotomy), with a mean pre-treatment AI of 44.7° improving only to 38° at six months. Conversely, the 41 cases that progressed satisfactorily without requiring further surgery had a mean pre-treatment AI of 39.6°, improving to 25.6° at 5 months. We found this variation to be highly significant in indicating whether the patient will require surgery in the medium term. Race and Herring17 also point out that, when the reduction obtained is satisfactory, the AI improves rapidly, without quantifying the radiological improvement. We have quantified the improvement that should be observed 5 months after the start of treatment to avoid a Salter-type osteotomy or similar: 10° regardless of whether a part-time or full-time abduction splint is used, as proposed by Stanitski.31
ConclusionsThe study has limitations, such as the fact that it is retrospective, the sample size, and the small number of cases with AVN.
From the observed outcomes, we would highlight that treating DDH using closed reduction and immobilisation with a spica cast is a safe and effective procedure. In IHDI or Tönnis type I and II hips, the results were excellent in almost all cases treated (98.9%). In type III/IV hips, the method obtained good outcomes in 64% of cases, and in 36% of cases, surgery (pelvic and/or femoral osteotomy) was necessary to improve joint congruence.
Based on our study, the major unfavourable prognostic factors are the initial clinical and radiological presentation (type III/IV dislocated hips and Galeazzi + and Ortolani +) and late diagnosis and treatment, particularly in the most displaced hips.
Radiological improvement of more than 10° in the AI within the first 5 months after reduction and placement of the initial cast is considered the most reliable indicator for avoiding surgery.
Early diagnosis, improved screening of cases in our healthcare area and the use of non-ionising radiation methods (MRI/ultrasound) for our patients are aspects to be implemented in the short term to improve the care of patients with DDH.
Level of evidenceLevel III evidence.
Ethical considerationsJustification for journal editors regarding the publication of healthcare quality assessments without an IRB.
The guide for research ethics committee members, produced by the Council of Europe's Steering Committee on Bioethics, defines clinical audits as reviews carried out in healthcare to ascertain whether best practices have been adopted. These audits are not subject to prior evaluation by an IRB. Therefore, the publication of results from reviews of departmental or clinical service performance is not considered research studies subject to IRB evaluation.
We would also like to note that in Galicia, Instruction 7/2019 on the protocol for processing data complementary to medical records, publicised by the Technical General Secretariat of the Regional Ministry of Health on 15 January 2020, regulates the performance of healthcare quality assessments. These assessments evaluate the healthcare provided to patients and analyse healthcare protocols to identify any necessary modifications or improvements. These quality assessments must be authorised by the head of the relevant service or unit and the manager of the healthcare institution. The relevant documents are attached to this publication for verification purposes.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interestsThe authors have no conflict of interests to declare.