The SL-Plus cementless stem was introduced in 1993 as an evolution of the Alloclassic® stem with some modifications. The aim of this study was to analyse if these modifications have any influence in clinical and radiological outcomes at minimum 10-year follow-up.
MethodsSixty-eight consecutive implants (64 patients) were retrospective evaluated. The mean duration of clinical and radiographic follow-up was 12.2 years. There were 41 female and 23 male patients with a median age of 73.5 years. All complications and reinterventions were collected. Functional outcomes were assessed using the modified Harris Hip Score (mHHS). Radiographs were evaluated immediately after the operation, after a minimum 2-year follow-up and by the end of follow-up (time A, B and C, respectively).
ResultsTwo stems were revised, one due to periprosthetic fracture and one due to aseptic loosening with a cumulative probability of not having a stem revision for any reason of 97.2% at 12.2 years. Mean mHHS was 76.7 points at the latest follow-up. Significant differences were found in distal migration (time A: 5.9mm±6.7; B: 6.9mm±7.1 and C: 8.2mm±6.3; P=.000) and varus angulation (time A: 0.0°±2; B: 0.0°±2 and C: 1.0°±3; P<.001), although these stems showed radiographic signs of osseointegration. Thirty-three hips (48.5%) showed any radiolucent line around the stem, most of them located the proximal femur (Gruen 1 and 7). Multivariate regression analysis showed lower mHHS scores in older patients (P=.004) and female (P=.00).
ConclusionsThe modifications of the SL-Plus stem influence the long-term outcome of the implant regarding radiological results, particularly in progressive varus angulation and distal migration. However, our study has not been able to demonstrate any clinical repercussions: functional scores and survival free of all cause revision were favourable and comparable to previous reports.
El vástago cementado SL-Plus fue introducido en 1993 como una evolución del vástago Alloclassic® con algunas modificaciones. El objetivo es describir los resultados clínicos y radiográficos del vástago SL-Plus en una serie de casos con un seguimiento mínimo de 10 años.
MétodosSe evaluaron de manera retrospectiva 68 implantes consecutivos (64 pacientes). La duración media del seguimiento clínico y radiográfico fue de 12,2 años. Hubo 41 pacientes mujeres y 23 varones, con una edad media de 73,5 años. Se recogieron todas las complicaciones y la necesidad de cirugía de revisión. Los resultados funcionales se evaluaron utilizando la escala de Harris modificada. Las radiografías se evaluaron inmediatamente después de la operación, tras un seguimiento mínimo de 2 años y al final del seguimiento (tiempo A, B y C, respectivamente).
ResultadosDos vástagos necesitaron una cirugía de revisión, uno de ellos debido a una fractura periprotésica y otro debido a aflojamiento aséptico, con una supervivencia libre de revisión del vástago del 97,2% a los 12,2 años. La escala de Harris modificada media fue de 76,7 puntos en el último seguimiento. Se encontraron diferencias estadísticamente significativas en la migración distal del vástago (tiempo A: 5,9±6,7mm; tiempo B: 6,9±7,1mm y tiempo C: 8,2±6,3mm; p=0,000) y la angulación en varo (tiempo A: 0,0±2°; tiempo B: 0,0±2° y tiempo C: 1,0±3°; p<0,001), si bien estos vástagos mostraron signos radiográficos de osteointegración. Treinta y tres caderas (48,5%) mostraron alguna línea radiolúcida alrededor del vástago, la mayoría de ellas ubicadas en el fémur proximal (Gruen 1 y 7). El análisis multivariable mostró puntuaciones de escala de Harris modificada más bajas en pacientes más ancianos (p=0,004) y mujeres (p=0,00).
ConclusionesLas modificaciones del vástago SL-Plus influyen en el resultado a largo plazo del implante con respecto a los resultados radiológicos, particularmente en la angulación en varo y la migración distal del vástago. Sin embargo, nuestro estudio no ha podido demostrar ninguna repercusión clínica: las puntuaciones funcionales y la supervivencia libre de revisión fueron favorables y comparables con estudios previos.
Since its introduction, cementless fixation in total hip arthroplasty has progressively increased its use over the years.1 Registry data show that cementless fixation is more popular in most countries, especially for the acetabular component.2,3
Tapered stems have demonstrated excellent long-term follow-up results.4–6 The cementless Alloclassic® Zweymüller stem (Zimmer; Winterthur, Switzerland) has demonstrated a 94% survival rate at 10 years and durable fixation at 15, 20, and 25 years.6–8 The cementless SL-Plus stem (Smith and Nephew, Watford, LN, UK) was introduced in 1993 as a further development of the Alloclassic® stem, introducing some modifications. Some authors have suggested that the sharp edges and corners of a rectangular Alloclassic® stem within a rounded femoral canal could be responsible for thigh pain and thickening of the distal femoral cortex, as well as a higher incidence of distal migration.7,9,10 The SL-Plus stem was therefore surface-treated with machined edges and rounded to theoretically reduce these complications.9,10
The objective of this article is to describe the clinical and radiographic outcomes of the SL-Plus stem in a case series with a minimum follow-up of 10 years. We therefore analysed its radiographic outcome at two different time intervals to address stem distal migration, position, and bone remodelling in the proximal femur. Clinical and implant survival data were also obtained to correlate with the radiological data.
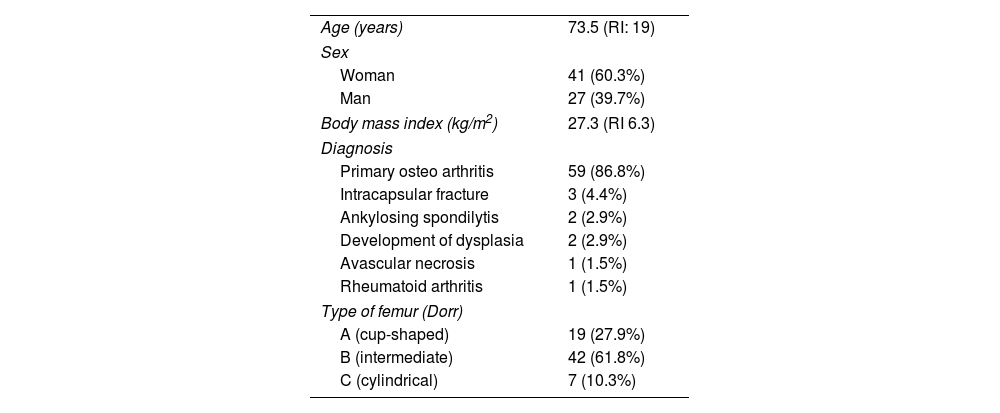
Material and methodsSeventy-eight uncemented SL-Plus stems were implanted consecutively in primary hip arthroplasties at our hospital between January 2010 and April 2012. The study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and Resolution 008430 of 1993 and was approved by our institution's Ethics Committee (internal code PI-2626). Informed consent was obtained from all patients who participated in the study. A minimum clinical and radiological follow-up of 10 years was required for inclusion in the study. The inclusion criteria included all SL-Plus stems implanted at our hospital, and there were no exclusion criteria. Five patients (5 hips) died of unrelated causes, and 5 were lost to follow-up. The remaining 68 hips (64 patients) formed the basis of the retrospective follow-up study. The mean clinical and radiographic follow-up was 12.2 years (standard deviation [SD]: 1.0). The preoperative characteristics of the patients are summarised in Table 1.
Epidemiological patient characteristics.
| Age (years) | 73.5 (RI: 19) |
| Sex | |
| Woman | 41 (60.3%) |
| Man | 27 (39.7%) |
| Body mass index (kg/m2) | 27.3 (RI 6.3) |
| Diagnosis | |
| Primary osteo arthritis | 59 (86.8%) |
| Intracapsular fracture | 3 (4.4%) |
| Ankylosing spondilytis | 2 (2.9%) |
| Development of dysplasia | 2 (2.9%) |
| Avascular necrosis | 1 (1.5%) |
| Rheumatoid arthritis | 1 (1.5%) |
| Type of femur (Dorr) | |
| A (cup-shaped) | 19 (27.9%) |
| B (intermediate) | 42 (61.8%) |
| C (cylindrical) | 7 (10.3%) |
The sandblasted, cementless SL-Plus stem is a straight, tapered stem with a rectangular cross-section forged from a titanium alloy. Two cementless designs were used for the acetabular component: the hemispherical R3 cup (Smith and Nephew, Watford, LN, UK) in 41 hips (60.3%) and the threaded BICON cup (Plus Orthopedics, Rotkreuz, Switzerland) in 27 hips (39.7%). Three different bearing pairs were used depending on the patient's age: metal on polyethylene in 51 cases, Oxinium™ on polyethylene in 3 cases, and ceramic (Biolox® delta) on ceramic in 14 cases.
The surgeries were performed by different hip surgeons at our hospital using a lateral Hardinge transgluteal approach (38 hips: 55.9%) or an anterolateral Watson Jones approach (30 hips: 44.1%). All patients received antibiotic prophylaxis (1g of cefazolin) intraoperatively and for 48h, following our institution's protocol. Patients received subcutaneous low-molecular-weight heparin to prevent thromboembolic events for 6 weeks after surgery. Weight-bearing with the use of two crutches was permitted from the first postoperative day, and after 6 weeks, the crutches were gradually withdrawn.
Clinical outcomes were assessed with the modified Harris Score (mHHS) at the final visit. All complications and the need for revision surgery were specifically sought and recorded.
Standard anteroposterior and lateral pelvic radiographs were obtained at each follow-up visit following the same protocol. Radiological measurements were calibrated using the known size of the femoral head implant as a reference. Radiographs were evaluated by two independent observers at three intervals: immediately postoperatively (time A), after a minimum follow-up of two years (time B), and at the final follow-up (time C).
Stem position was defined as neutral, varus (>3°), or valgus (<3°) using the angle between the femoral axis and the longitudinal stem axis. Migration was assessed by measuring vertical stem subsidence according to the method described by Callaghan et al.11 Femoral canal filling, measured as the ratio of stem width to medullary canal width, was determined at 3 levels: level A (femoral neck), level B (below the lesser trochanter), and level C (1cm proximal to the stem tip). The distribution of any radiolucent or radiopaque lines (<2mm) or osteolysis (≥2mm) was recorded in the areas described by Gruen et al.12 Proximal femoral disuse osteopenia was classified according to the system described by Engh et al.,13 Heterotopic ossification was classified according to the system described by Brooker et al.14 Cup position was determined by the angle of acetabular abduction, the vertical distance measured from the centre of the femoral head to the ipsilateral teardrop, and the horizontal distance of the cup, measured from the centre of the femoral head to the Köhler line.15
Statistical analysis was performed using standard software (SPSS® v. 21.0; IBM, Armonk, NY, USA). Normality analysis of quantitative variables was performed using the Kolmogorov–Smirnov test. Student's t test, Mann–Whitney U test, Kruskal–Wallis test, Friedman test, or Wilcoxon test were used depending on data distribution. Kaplan–Meier survival analysis was used to estimate the cumulative probability of not undergoing stem revision for any reason. Multivariate analyses using Cox survival regression, logistic regression, or multiple linear regression were performed to determine significant predictors of all-cause revision, periprosthetic fracture, and mHHS score. Statistical significance was set at p<.05.
ResultsThe mean mHHS score was 76.7 points (SD: 12.6) at the last follow-up. Ten patients (14.7%) reported mild pain, which did not affect their daily activities.
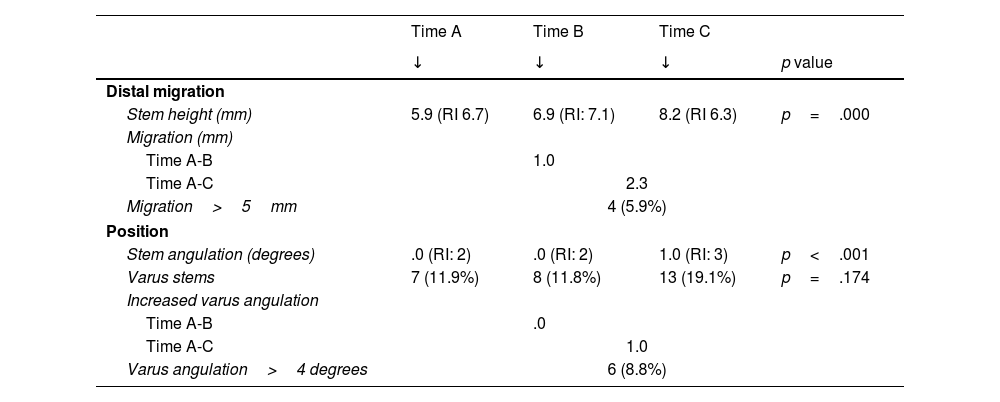
All stems except one showed radiographic evidence of bone in-growth. Femoral canal filling was greater at level C (76±12%) than at level B (71±9%) and level A (67±10%) (p=.000). The results of stem migration and position are shown in Table 2. Significant differences were found in stem migration and varus angulation (p<.05) (Fig. 1). Four hips (5.9%) had a pedestal sign at time B and 8 hips (11.8%) at time C. Thirty-three hips (48.5%) showed some radiolucent line around the stem. The distribution of radiolucent lines is presented in Fig. 2. Osteolysis was observed in only one hip; it was non-progressive and was located in the proximal femur (Gruen 1, 2, and 6). Proximal disuse osteopenia was grade 1 in 10 hips (14.7%), grade 2 in 16 hips (23.5%), and grade 3 in 5 hips (7.4%). Grade 1 heterotopic ossifications developed in 25 hips (36.8%) and grade 2 in 6 hips (8.8%).
Migration and stem position during follow-up.
| Time A | Time B | Time C | ||
|---|---|---|---|---|
| ↓ | ↓ | ↓ | p value | |
| Distal migration | ||||
| Stem height (mm) | 5.9 (RI 6.7) | 6.9 (RI: 7.1) | 8.2 (RI 6.3) | p=.000 |
| Migration (mm) | ||||
| Time A-B | 1.0 | |||
| Time A-C | 2.3 | |||
| Migration>5mm | 4 (5.9%) | |||
| Position | ||||
| Stem angulation (degrees) | .0 (RI: 2) | .0 (RI: 2) | 1.0 (RI: 3) | p<.001 |
| Varus stems | 7 (11.9%) | 8 (11.8%) | 13 (19.1%) | p=.174 |
| Increased varus angulation | ||||
| Time A-B | .0 | |||
| Time A-C | 1.0 | |||
| Varus angulation>4 degrees | 6 (8.8%) | |||
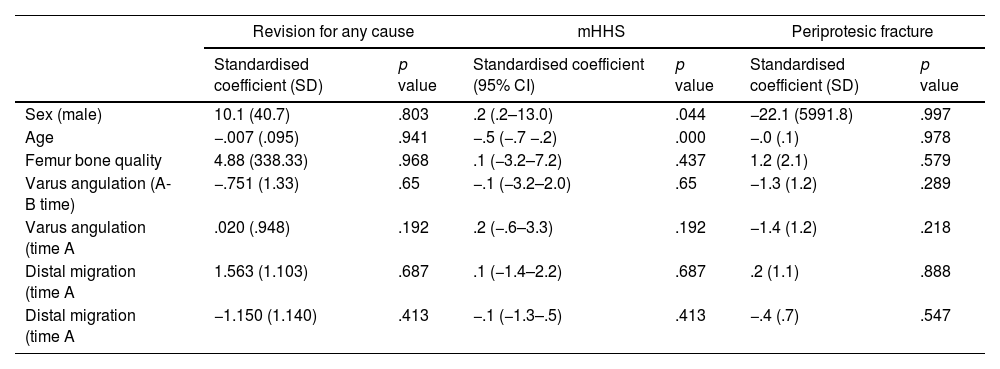
Multivariate analysis showed lower mHHS scores in older patients (p=.004) and in women (p=.000) (Table 3).
Multivariable regression for revision for any reason, mHHS and periprothesic fracture.
| Revision for any cause | mHHS | Periprotesic fracture | ||||
|---|---|---|---|---|---|---|
| Standardised coefficient (SD) | p value | Standardised coefficient (95% CI) | p value | Standardised coefficient (SD) | p value | |
| Sex (male) | 10.1 (40.7) | .803 | .2 (.2–13.0) | .044 | −22.1 (5991.8) | .997 |
| Age | −.007 (.095) | .941 | −.5 (−.7 −.2) | .000 | −.0 (.1) | .978 |
| Femur bone quality | 4.88 (338.33) | .968 | .1 (−3.2–7.2) | .437 | 1.2 (2.1) | .579 |
| Varus angulation (A-B time) | −.751 (1.33) | .65 | −.1 (−3.2–2.0) | .65 | −1.3 (1.2) | .289 |
| Varus angulation (time A | .020 (.948) | .192 | .2 (−.6–3.3) | .192 | −1.4 (1.2) | .218 |
| Distal migration (time A | 1.563 (1.103) | .687 | .1 (−1.4–2.2) | .687 | .2 (1.1) | .888 |
| Distal migration (time A | −1.150 (1.140) | .413 | −.1 (−1.3–.5) | .413 | −.4 (.7) | .547 |
SD: standard deviation; CI: confidence interval; mHHS: modified Harris scale.
The mean acetabular angle was 48.8° (SD: 9.0), the mean hip centre height was 19.7mm (SD: 5.1), and the horizontal cup distance was 30.2mm (SD: 6.1). The mean abductor moment was 52.2mm (SD: 9.7), and the mean femoral offset was 38.7mm (SD: 8.0).
Among intraoperative complications, there was a greater trochanter fracture, which was managed with cerclage during the same surgery. This hip showed radiographic evidence of bone in-growth and a good clinical outcome during follow-up.
There were 3 periprosthetic fractures (4.4%), 2 type B1 fractures at 4 and 7 years of follow-up, treated with internal fixation, and one type B2 fracture after 7 years that required femoral stem revision. There were no dislocations or deep infections. Another stem (1.5%) was revised due to aseptic loosening after 4 years. The survival rate free of stem revision for any reason was 97.2% at 12.2 years of follow-up.
DiscussionPrevious studies have described an initial distal stem migration that stabilises at 2-year follow-up 16–18 between .40 and .73mm, which is lower than the 1.0mm found in our study.18 However, in our series, this distal stem migration was not stable and progressed to 2.3mm when assessed during long-term follow-up.
Regarding stem angulation, it has been reported to be .04° of varus at 2-year follow-up and 1.8° of varus at 13–15 years.17,19 It was similar in our series, with .0° of varus at 2 years and 1.0° of varus at 12.2 years. Along these lines, it is striking that 5.9% and 8.8% of the stems in our series presented subsidence greater than 8mm and varus angulation greater than 4°, respectively. Thus, it could be inferred that the SL-Plus stem migrates as early as the first years of follow-up, but that varus angulation occurs later.
The development of radiolucent lines described at 11 and 15 years of follow-up is 29% and 38%, respectively, primarily affecting zones 1 and 7.19,20 In our series, it is slightly higher (50%), also predominantly affecting zones 1 and 7. This could reflect that distal stem migration is due to radiolucent lines in the proximal femur, although implant stability does not appear to be compromised in our series.
Despite observing these progressive long-term radiological changes, we were unable to find any clinical correlation. Furthermore, our patients’ functional scores were good, and all-cause revision-free survival is very favourable compared with other series.16,21,22 These findings suggest that, although radiological changes in the implant may occur over time, they do not appear to significantly affect the clinical outcome or overall performance of the SL-Plus stem. However, further research and studies with longer follow-up will be needed to fully confirm and understand the implications of the observed radiological progression and its potential impact on clinical outcomes in the future. To better understand the potential impact of these design changes, it would be interesting to compare the SL-Plus with its previous stem design. The Alloclassic® Zweymüller cemented stem has shown excellent long-term results with 94% survival at 10 years and durable fixation at 15, 20, and 25 years.6–8
The high proportion of periprosthetic fractures in our series (4.4%) is striking when compared to series of the same stem with similar follow-up (0.6–1.3%), although no association with epidemiological or radiological factors could be found in the multivariate analysis.19,20,22 Furthermore, the infection and dislocation rate in our series (0%) is lower than that reported in similar series (.1–2.0% for infection and .9–1.3% for dislocation).19,210,22,23 The low dislocation rate in our series appears to be explained by the use of the lateral and anterolateral approaches.24
One of the main limitations of this study is its retrospective design. The lack of a comparative group reduces the ability to establish cause-effect relationships and limits the internal validity of the findings. The study's long-term follow-up provides valuable evidence. However, the inherent presence of patients lost to follow-up may bias the results and reduce the representativeness of the sample. The study relies on the use of plain radiographs to measure the degree of stem subsidence and varus angulation. Although plain radiography is a widely used tool in clinical practice, its accuracy is limited. It would be interesting to incorporate much more precise methods such as radiostereometric analysis in future studies to validate these results.17,25 Therefore, studies that overcome these limitations, with study designs of higher methodological quality, are needed.
The main conclusion of this study is that the SL-Plus stem undergoes varus angulation and progressive distal progression during the long-term follow-up of our sample, although without affecting functional outcomes compared to previous studies.
Level of evidenceLevel of evidence iv.
Ethical considerationsThis research was approved by the hospital's Ethics Committee. The authors obtained informed consent from the patients and/or subjects mentioned in the article. This document is in the possession of the corresponding author.
FundingNone of the authors received any funding for this research study.
Conflict of interestsThe authors have no conflict of interest to declare.