Lymphatic insufficiency in extremities has been extensively dealt with.1,2 In contrast, chronic facial lymphedema is an uncommon disease. There are few published articles in the literature reviewed concerning the management of isolated facial lymphedema.1•3 The etiology could be a primary disease, whether dermatological and inflammatory, infectious or congenital (Morbihan disease, nephrotic syndrome, Hennekam syndrome, Melkersson•Rosenthal syndrome).1,2,4•7 On the other hand, it can be secondary to treatment for head and neck tumors (ablative surgery, neck dissection and locoregional radiotherapy (RT)).1,2,5 The etiology and pathogenesis consist of lymphatic blockage by scar tissue, trauma or repeated episodes of infection and inflammation.2 It is usually transitory because the flow is diverted to the collateral vessels. If the collateral flow is seen to be compromised, the inflammation may be progressive and require emergency treatment.2
It causes functional alterations (difficulty in swallowing and speaking) and visible disfigurement, and the patient has to cope with the psychological impact caused by the deformity and social isolation.1
The therapeutic options are pharmacological (diuretics, benzopyrones and flavonoids), rehabilitative (drainage and compression1) and surgical (local excision, liposuction, dermolipectomy, autologous lymph vessel transplantation, lymphaticovenous anastomosis and microsurgical flaps).1,5,8
We present a case of successful drainage of an unremitting facial lymphedema via the dermal lymphatic vessels of a deltopectoral flap.
Case reportThe patient was 67-year-old man who presented with unremitting facial lymphedema. He had undergone surgery for supraglottic epidermoid carcinoma, which had consisted of supraglottic laryngectomy with bilateral neck dissection and RT. As drug therapy, he had received amlodipine, mannitol, acetazolamide, furosemide and dexamethasone. This provoked unstable, fluctuating blood pressures, hyperglycemia and hyponatremia, which affected the patient's hemodynamic status. Rehabilitative treatment, liposuction and a hypobaric chamber were also used, but with no success.
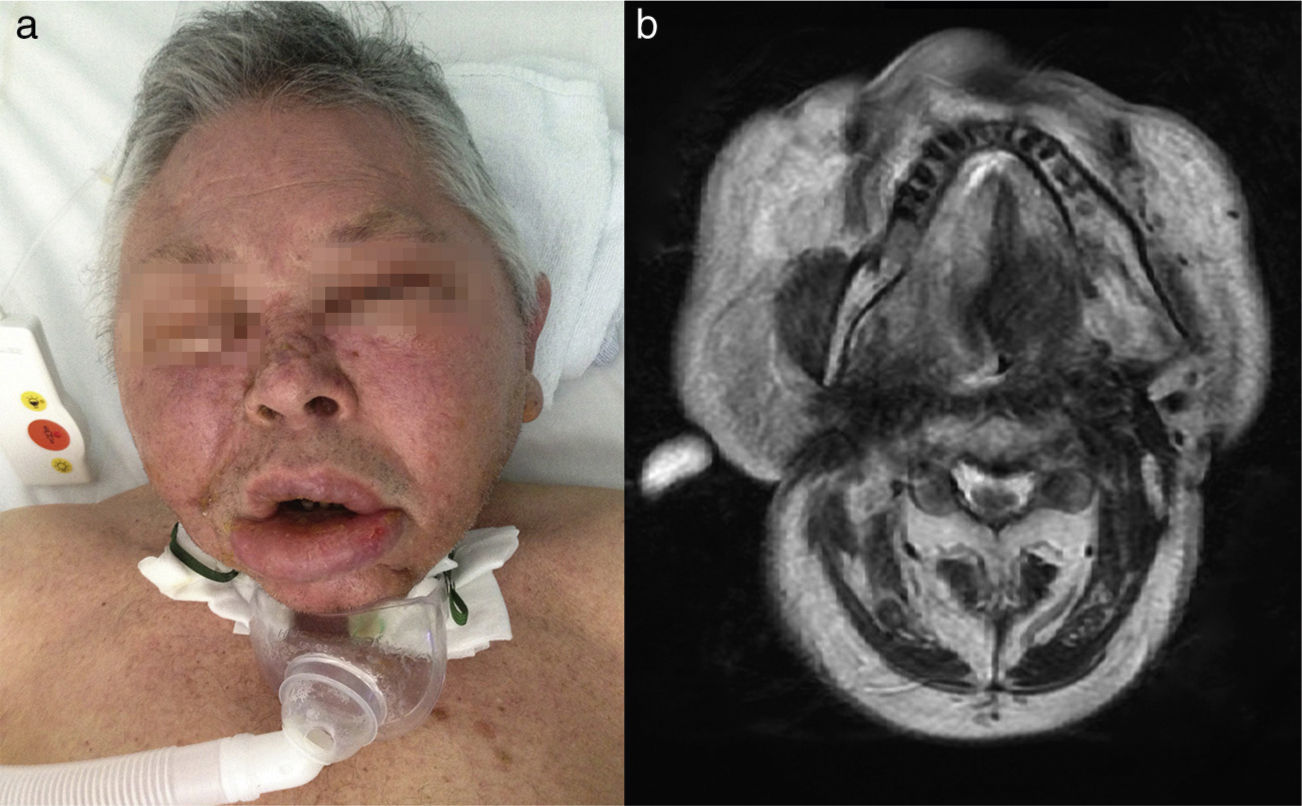
When he was referred to us, the patient had massive facial edema, extensive neck fibrosis, tracheotomy, gastrostomy, dyspnea with an oxygen saturation of 85%, edema of both eyelids that did not allow him to raise his eyelids voluntarily, conductive hearing loss, lip incompetence and inability to swallow (Fig. 1 a and b).
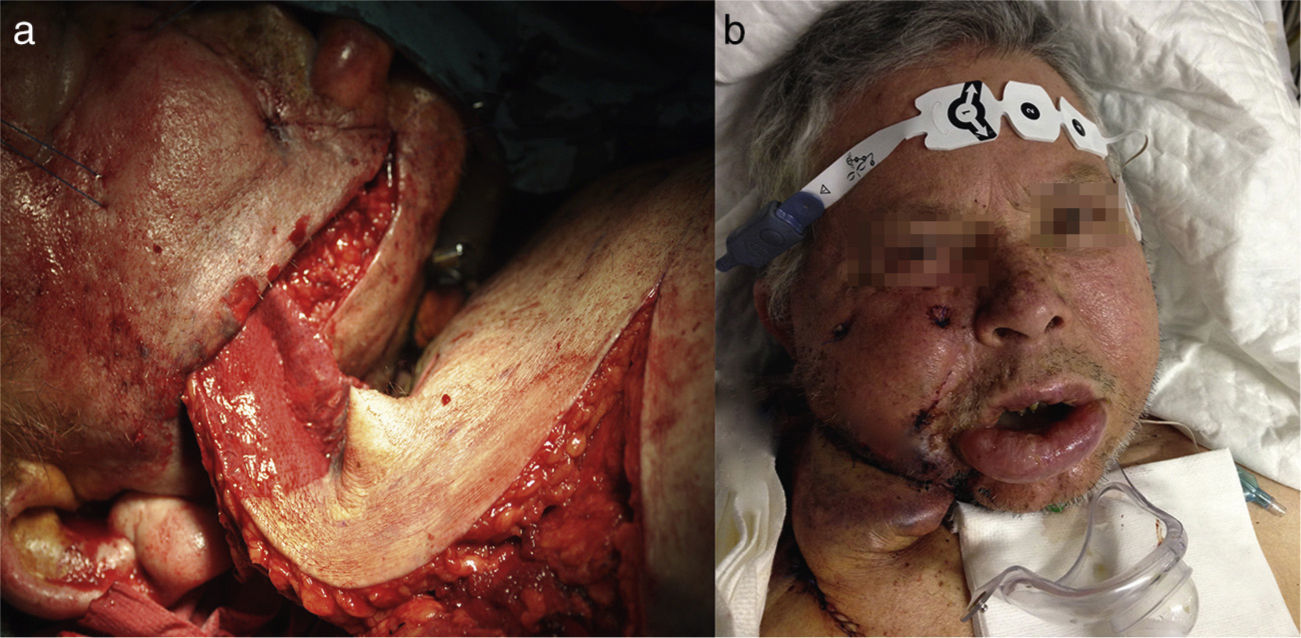
We decided to employ a deltopectoral myocutaneous flap using a delay procedure for the purpose of introducing new lymphatic vessels into the patient's cheek to improve his condition.
A right deltopectoral flap was harvested, a distal area of 6í5cm was de-epithelialized and introduced into a subcutaneous pocket in the patient's cheek. Direct closure of the defect was performed, excluding the distal end, which was covered with the de-epithelialized tissue in the form of a free skin graft (Fig. 2 a and b). Seventy-two hours later, he began to hear and see, his lip competence had improved and his facial volume had decreased. One week later, he developed respiratory distress provoked by right basal atelectasis, which worsened progressively. It was accompanied by atrial fibrillation, hyponatremia and hyperglycemia. Finally, he died 31 days after surgery due to multiple organ failure.
DiscussionFacial lymphedema is a condition that can have multiple etiologies. It is uncommon but, when it occurs, it can be devastating.9 As a result of a poorly functioning surgical drain, protein-rich lymphatic fluid accumulates in the interstitium. The accumulation of fibroblasts and the reduction in the number of macrophages provoke a fibrotic induration of the tissue and this fibrosis compresses the flow, making the situation worse.
Piso et al.1 used manual lymphatic drainage according to the Vodder method,1 but this approach can result in complications: tumor spread, thrombosis, infection, hypotension and carotid sinus syndrome.
Felmerer et al.10 presented a series of 14 patients treated by means of autologous microsurgical lymph vessel transplantation.
Mihara et al.8 described the technique of lymphaticovenous anastomosis (LVA) using supermicrosurgery, and Ayestaray et al. present 4 cases of LVA.
Corten et al.3 reported the case of a patient treated with a free pectoralis major flap, and Clodius et al.11,12 described 1 case involving a pedicled groin flap and another in which an axillary (lateral thoracic) flap was used. Smith and Conway2 also employed a lateral thoracic flap. Withey et al.2 reported their experience using a lymphatic bridge with a deltopectoral flap. Cheng et al.5 presented 6 patients treated by means of a vascularized submental lymph node flap, and Becker et al.13 and Lin et al.14 employed groin lymph node transfer.
In the case we report, the chronic and disabling nature of the process and the patient's precarious hemodynamic status led us to choose a surgical technique that would involve only limited invasiveness, while being simple and effective. It consisted in the transfer of lymph nodes in the subcutaneous tissue of the deltopectoral flap to the subcutaneous pocket in the patient's cheek, where the lymphatic drainage system was damaged. Because of its proximity, the transferred tissue generated a new lymphatic network (lymphogenesis), which connected with the affected lymphatic and venous network.
We report the drainage of a facial lymphedema with satisfactory bilateral results, despite the unilateral placement of the flap. The facial appearance was improved, as well as the auditory and visual functions, despite the patient's final outcome.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe authors declare that they have received no outside funding.
Conflicts of interestThe authors declare they have no conflicts of interest.
Please cite this article as: Martínez-Pèc)rez F, Arribas-García I, Álvarez-Flórez M. Manejo quirúrgico del linfedema facial secundario a tratamiento oncológico. Rev Esp Cir Oral Maxilofac. 2016. http://dx.doi.org/10.1016/j.maxilo.2015.03.007