The present retrospective study explored the spectrum and characteristics of patients treated with orthognathic surgery at the Universidade Federal do Paraná, Brazil.
Materials and methodOver a six-year period from July 2002 to July 2008, the records of 195 patients with dentofacial deformities who underwent orthognathic surgical procedures were followed up.
ResultsMean patient age was 25.87 years (range 14 to 65 years) and the female to male ratio was 1.5:1. The predominant racial group was “white”. Most patients belonged to the economically productive population. Sixty-two patients had complete dentition. Only 3.59% patients had local anesthesia (rapid palatal expansion). Transverse maxillary deficiency was the most common deformity, followed by maxillary anteroposterior deficiency associated with mandibular anteroposterior excess. Mandibular set-back was the intervention most frequently performed. The surgical procedures took an average of 3 hours 51 minutes and orthodontic treatments took an average of 44.48 months. Complications occurred in 22.57% of patients, the most common of which were permanent paresthesia of the lower lip (7.17%) and inadequate fracture reduction (5.12%).
ConclusionsThe findings included concepts that were useful for characterizing the profile of patients who undergo orthognathic surgery in southern Brazil. The results also may help to correctly develop protocols for patient care designed to improve the overall results of the procedures.
Este estudio retrospectivo explora el espectro y las características de los pacientes tratados con cirugía ortognática en la Universidade Federal do Paraná.
Material y métodoA lo largo de 6 años, a partir de julio de 2002 hasta julio de 2008, se efectuó el seguimiento de 195 pacientes con deformidades dentofaciales que se sometieron a procedimientos de cirugía ortognática.
ResultadosLa edad media de los pacientes fue de 25,87 años (de 14 a 65) y la proporción de mujeres y hombres fue de 1,5:1. El grupo racial predominante fue el “blanco”. La mayoría de los pacientes eran parte de la población económicamente productiva. Sesenta y dos pacientes tenían la dentadura completa. Sólo el 3,59% de los pacientes fueron sometidos a anestesia local (expansión rápida de paladar). La deficiencia transversal maxilar fue la deformidad más común, seguida por la deficiencia anteroposterior del maxilar asociado con el exceso anteroposterior del maxilar inferior. La cirugía más realizada fue el retroceso mandibular. El procedimiento de cirugía duró una media de 3 h y 51 min, y el tratamiento de ortodoncia se prolongó 44,48 meses. Hubo complicaciones en el 22,57% de los pacientes, y las más habituales fueron parestesias (7,17%) y reducción inadecuada de la fractura (5,12%).
ConclusionesLos resultados de esta investigación muestran algunos conceptos que pueden caracterizar el perfil ortognático de los pacientes en el sur de Brasil. También tiene como objetivo colaborar en la correcta instauración de protocolos de cuidado de los pacientes a fin de mejorar los resultados de los procedimientos.
Dento-facial deformity is described as a deformity that mainly affects the jaws and dentition. However, the mid and lower portions of the face may also be affected. Deformities may either be isolated to one jaw or extend to multiple craniofacial structures1. Important advances in diagnostic tools, treatment planning and surgical techniques have made orthognathic surgery a common and safe procedure for the management of dento-facial deformities2. Modern fixation techniques (internal rigid fixation) and the achievement of improved facial esthetics have contributed toward the confidence of patients regarding this type of surgery and have led to an increased demand for orthognathic procedures3,4. However, with this comes the importance of characterizing patients who have undergone this procedure in order to enable an improvement of the process as a whole.
There are few available epidemiological studies on this issue around the world. Some investigations are limited to the spectrum of dento-facial deformities1,2,5,6. Others only address surgical procedures for the correction of a specific type of deformity7–9. Others report the prevalence of malocclusion10–12.
The present article attempts to fill some of the gaps of this field by reporting features of interest related to orthognathic surgery, such as basic epidemiology (male/female gender, age, ethnic background, dental aspects, deformities and surgical procedures), duration of treatment and associated complications.
MethodsA comprehensive analysis was performed of all patient charts in the orthognathic surgery records. All patients having undergone orthognathic surgery at the Oral-Maxillofacial Surgery Department of the Universidade Federal do Paraná (Brazil) between June 2002 and June 2008 were included. Patients with cleft lip/palate or syndromes were excluded. The following were the orthognathic procedures preformed: bilateral sagittal split osteotomy (BSSO); Le Fort I osteotomy; genioplasty; and rapid palatal expansion either alone or in combination with additional procedures.
The patients were submitted to a history background, physical examination and appropriate laboratory tests. Excluding edentulous patients, all cases underwent presurgical orthodontics. All the patients consented to surgery and underwent the operation at the hands of residents and a senior surgeon.
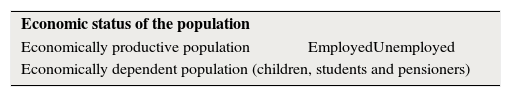
Each record was analyzed following a strict protocol, including the date of first examination, age, gender, racial group (white, Asian, Amerindian, multiracial and black) and economic status (Table 1). The classification of racial group and economic status was based on the criteria of the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística)13.
Each patient's dental situation was investigated and divided into edentulous, partial dentition or complete dentition. Bone conditions were also analyzed. The diagnostic spectrum for dento-facial deformities was as follows: vertical maxillary deficiency or excess; transverse maxillary deficiency; anteroposterior maxillary deficiency or excess; maxillary rotation; anteroposterior mandibular deficiency or excess; mandibular asymmetry; macro or microgenia; open bite; and combined deformities. Cephalometric analyses were derived from a composite analysis of Ricketts, Downs, Stainer, Tweed, Holdaway, Gonzalez and Burstone14. Other aspects analyzed were type of surgical procedure, date of surgery, local or general anesthesia, duration of orthodontic treatment, duration of surgery and complications related to procedure performed.
It should be stressed that the Oral-Maxillofacial Surgery Service of the Universidade Federal do Paraná provides service to the state government of Paraná, Brazil. Thus, there is no cost to the patient regarding radiology or the complete surgical procedure.
All data were analyzed with the aid of the Microsoft Excel program for Windows (XP Professional® 2007, Microsoft Corporation©, USA). For such, descriptive statistics (frequencies), the chi square test and t test were used, with the level of significance set at 5%. The study received approval from the ethics committee of the Universidade Federal do Paraná.
ResultsA total of 195 patients underwent orthognathic surgery over the six-year period analyzed. Patient age ranged from 14 to 65 years (mean: 25.87). There was a difference in mean age between females and males (27.04 and 24.13, respectively). Female patients outnumbered male patients by a ratio of 1.5 to 1. The racial distribution was 89.23% white, 6.67% multiracial, 3.08% black, 0.51% Asian and 0.51% missing record. There were no Amerindians. Economic status was listed in 92.31% of the charts. There were 119 patients in the economically productive population and 89.07% of these were employed. The economically dependent population was comprised entirely of students and pensioners (61 patients).
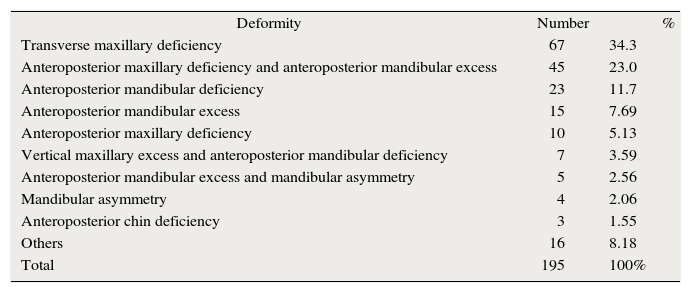
Regarding dental situation, 62.05% had a complete dentition, 36.92% had a partial dentition and 1.03% were edentulous. The maxilla was the most affected (40.51%), followed by the maxilla and mandible combined (32.30%) and mandible alone (27.19%). Transverse maxillary deficiency was the most common deformity, followed by anteroposterior maxillary deficiency associated to anteroposterior mandibular excess. Deformities found in two patients or fewer were categorized as "others" (deformity spectrum; Table 2).
Incidence of dentofacial deformities in 195 patients having undergone orthognathic surgery
| Deformity | Number | % |
| Transverse maxillary deficiency | 67 | 34.3 |
| Anteroposterior maxillary deficiency and anteroposterior mandibular excess | 45 | 23.0 |
| Anteroposterior mandibular deficiency | 23 | 11.7 |
| Anteroposterior mandibular excess | 15 | 7.69 |
| Anteroposterior maxillary deficiency | 10 | 5.13 |
| Vertical maxillary excess and anteroposterior mandibular deficiency | 7 | 3.59 |
| Anteroposterior mandibular excess and mandibular asymmetry | 5 | 2.56 |
| Mandibular asymmetry | 4 | 2.06 |
| Anteroposterior chin deficiency | 3 | 1.55 |
| Others | 16 | 8.18 |
| Total | 195 | 100% |
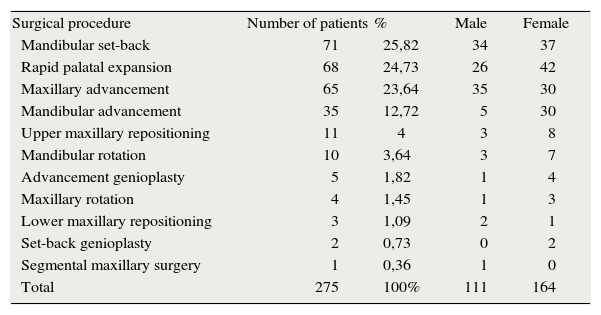
A total of 275 surgical procedures were performed. Some patients needed more than one procedure in the same surgery in order to correct the deformity. For the purposes of analysis, the surgeries were divided by procedure performed and a single surgery could comprise more than one procedure. The ratio of females to males was 1.4:1. There was an increase in combined procedures over the years. In the first three years of the analysis, 33.7% of all orthognathic surgeries were combined, whereas this figure increased to 40.6% in the last three years. Mandibular set-back, rapid palatal expansion and maxillary advancement were the most common procedures performed. In addition to one of these procedures, mandibular advancement and maxillary impaction were also performed. Table 3 displays the number and gender of the patients in all procedures. The findings were submitted to the Shapiro-Wilk normality test, followed by the Student's t-test (95% confidence interval) and chi-square test. These tests were used to analyze gender differences in each surgical procedure. Only mandibular advancement exhibited a statistically significant difference between genders (p ≤0.5).
Surgical procedures according to gender
| Surgical procedure | Number of patients | % | Male | Female |
| Mandibular set-back | 71 | 25,82 | 34 | 37 |
| Rapid palatal expansion | 68 | 24,73 | 26 | 42 |
| Maxillary advancement | 65 | 23,64 | 35 | 30 |
| Mandibular advancement | 35 | 12,72 | 5 | 30 |
| Upper maxillary repositioning | 11 | 4 | 3 | 8 |
| Mandibular rotation | 10 | 3,64 | 3 | 7 |
| Advancement genioplasty | 5 | 1,82 | 1 | 4 |
| Maxillary rotation | 4 | 1,45 | 1 | 3 |
| Lower maxillary repositioning | 3 | 1,09 | 2 | 1 |
| Set-back genioplasty | 2 | 0,73 | 0 | 2 |
| Segmental maxillary surgery | 1 | 0,36 | 1 | 0 |
| Total | 275 | 100% | 111 | 164 |
Only seven patients underwent orthognathic surgery with local anesthesia (all cases of rapid palatal expansion). The other 188 patients were submitted to general anesthesia. Procedures carried out under general anesthesia took an average of three hours 51 minutes (ranging from 1 hour to 8 hours 30 minutes). The mean duration of orthodontic treatment was 44.48 months. The mean period between first examination with the surgeon and the day of surgery was 17.18 months (in most cases, the surgeon's first examination did not coincide with the orthodontist's first examination).
Fifty-one complications associated to orthognathic surgery occurred among 44 patients: permanent paresthesia in lower lip (14 patients; 7.17%); inadequate fracture (10 patients; 5.12%); inadequate occlusion (3 patients; 1.53%); exposure of fixation material (3 patients; 1.53%); hemorrhage (2 patients; 1.02%); recurrence within a short period of time (2 patients; 1.02%); inadequate fixation (2 patients; 1.02%); and breaking of orthodontic appliance (2 patients; 1.02%). Less common complications were nasal septum deviation, lip injury, oral mucosa hyperplasia, degeneration of the facial nerve, incorrect planning, hyperesthesia, exacerbated swelling, hypertension crisis during surgery, arm swelling due to poor position during surgery and inadequate urethral catheterization, totaling 11 patients (5.64%).
DiscussionAll 195 patients analyzed in the present study had some type of dentofacial deformity. Thus, no conclusions may be drawn regarding the incidence of these deformities in the population as a whole. As expected, there was a predominance of female patients and a predominant age group2,6,9,15. It has been described that the younger age group tends to express a greater concern with aesthetics, while the older age group is less inclined to have surgery and is more concerned with the risks of surgery1. In the present study, white individuals were predominant, which is explained by the European colonization of southern Brazil13.
Few previous studies have addressed the occupations of individuals having undergone orthognathic surgery. The patients from the economically productive population sought orthognathic surgery more than those from the economically dependent population, which is in disagreement with a previous study1. However, further studies are needed to determine the true profile of these patients.
The maxilla was the most affected bone, as reported in previous studies3,15. When this bone is most affected, authors generally include transverse maxillary deficiency deformities. Otherwise, the maxilla and mandible together is reported to be the most commonly affected2. However, it is difficult to compare findings, as some studies classify deformities based on the Angle Classification and others based on facial deformities16.
Transverse maxillary deficiency was the most common deformity and was a component of a large number of cases of malocclusion. The high number of cases of transverse maxillary deficiency could be associated to factors such as the fact that the surgical procedure is simple, the combination of this deformity with others, which limits the treatment process, or the cessation of orthodontic expansion. Anteroposterior maxillary deficiency and anteroposterior mandibular excess (Class III) was the second most common deformity, which is in agreement with a number of studies2,6. This suggests that this deformity is somewhat unacceptable to the population and makes many patients seek treatment. One study revealed that a higher number of individuals with severe Class III malocclusion sought treatment in comparison to those with severe mandibular deficiency1. Another study on facial profile attractiveness found that a protrusive mandibular profile was the least attractive4. The reasons patients with transverse maxillary deficiency or anteroposterior maxillary deficiency and anteroposterior mandibular excess sought the treatment were different. The former group sought treatment through the recommendation of an orthodontist and the latter group has sought treatment on their own due to issues of aesthetics.
Surgical procedures mainly involved rapid palatal expansion and mandibular set-back, either alone or combined with another procedure. Mandibular advancement was less common, implying that this deformity was relatively more acceptable on the part of the population6.
The duration of surgery was directly related to the complexity of the orthognathic procedure and experience of the surgeon. The surgeries were performed by residents with different levels of skill. Thus, the mean duration of surgery cannot be compared with the findings of studies involving senior surgeons alone. Similar studies report a mean duration ranging from three hours 51 minutes to three hours 54 minutes15.
Total duration of orthodontic treatment was 44.48 months, which is long in comparison to previous studies reporting a mean duration of 38.6 months or 21.9 months17,18. At the oralmaxillofacial surgery department analyzed in the present study, the patients themselves select their orthodontist of choice. Therefore, 115 different orthodontists were involved in this study. In many cases, the increase in duration was due to inadequate planning on the part of the orthodontist and frequent failure of patients to show up for scheduled appointments.
The most common postoperative complication was permanent paresthesia in the lower lip. Since the inferior alveolar nerve is exposed during mandibular ramus osteotomy, immediate postoperative paresthesia of the nerve is common, with a reported incidence of 85% to 87%1. However, the present study only considered long-term paresthesia, which is reported to range from 1.3 to 7%19. Inadequate fractures occurred in 5.12% of patients, which is similar to the findings described in a previous study (1% to 9.2%)19. Rigid intermaxillary fixation was applied for six weeks among the patients in the present study, with good aesthetic and functional results. There was a low incidence of other problems, all of which were solved. Serious complications and other problems seem to be quite rare in orthognathic surgery, which is a very safe method. However, typical complications should be stressed during preoperative counseling to the patient, at this is an elective surgery.
ConclusionThe purpose of the present study was to analyze features related to orthognathic surgeries performed at the Oral-Maxillofacial Surgery Service of the Universidade Federal do Paraná in the city of Curitiba (PR, Brazil). Improvements in this area can be only achieved through in-depth analysis of all procedures. It is also important to establish the profile of the patients having undergone orthognathic surgery in order to achieve better results. There are few studies on orthognathic epidemiology. Further studies should be carried out with the aim of determining the profile of orthognathic surgery patients in different countries and thus preparing orthognathic surgeons to achieve better results.