This study aims to identify the characteristics and factors associated with TDI treated at a referral service.
Material and methodsA ten-year period cross-sectional retrospective analysis of medical records of patients with TDI in their permanent teeth was performed, and injury-related data were collected. Statistical analysis was performed using the chi-square association test and complex analysis (p<0.05).
ResultsRecords of 545 patients, totaling 1438 traumatized teeth, were evaluated, and a male prevalence at a 2.4:1 ratio was found. The age group with highest incidence was 13–19 years. Central maxillary incisors and dislocations were the most affected teeth and TDI, respectively. Statistical analysis showed different TDI causes according to age: children are often victims of falls, traffic accidents, aggression and collisions, whereas adolescents are involved in sports accidents, and young adults in traffic accidents, falls and collisions.
ConclusionConsidering the scope of this retrospective study at a single referral center, a profile of young male patients with TDI in superior central incisors due to falls, collisions, traffic accidents or sports could be detected.
Identificar las características y los factores asociados con el traumatismo dentoalveolar (TD) atendido en un servicio de referencia.
Material y métodosHa sido realizado un análisis retrospectivo de los pacientes con TD en dientes permanentes en un período de10 años. Fueron extraídos los datos relacionados con el TD. El análisis estadístico se realizó mediante el test de asociación chi-cuadrado y el análisis de los residuos (p<0,05).
ResultadosLos registros de 545 pacientes con un total de 1.438 dientes traumatizados fueron incluidos. Se constata la prevalencia en el sexo masculino, con una proporción de 2,4:1. El grupo etario con mayor incidencia fue el de 13-19 años. Los incisivos centrales superiores fueron los dientes más afectados y el traumatismo dentario más diagnosticado fueron las luxaciones. El análisis estadístico ha mostrado una asociación de diferentes causas de TD con la edad: los niños son víctimas, con mayor probabilidad, de caídas, accidentes de tránsito, agresiones y colisiones, mientras que los adolescentes los son de accidentes deportivos, y los adultos jóvenes de accidentes de tráfico, caídas y colisiones.
ConclusiónConsiderando el alcance de este estudio retrospectivo en un único servicio de referencia, se detectó un perfil de jóvenes pacientes del sexo masculino con la presencia de TD en los incisivos centrales superiores por las caídas, colisiones, accidentes de tráfico o prácticas deportivas.
Traumatic dental injuries (TDI) accounts for about 5.0% of all bodily trauma.1–3 However, its incidence and characteristics changes according to age group and socio-demographic factors involved, as is the case of children injuries, in which TDI represents 17.0–20.0% of all traumas they were involved in.4
Unlike other injuries, the incidence of these lesions decreases from the second decade of life.1,2,4 This can be explained by periodontal ligament space characteristics, upper incisor exposure and lack of lip sealing during the growth phase. In addition, there is an association between Class II malocclusion and TDI.5 Among dental elements, the upper central incisors are most commonly affected due to their projection and exposure.5 Less complex injuries such as single crown fracture and concussion are more frequent than complicated crown fractures or severe dental dislocations.6,7
TDI is a public health hazard due to its high frequency and association with violence, traffic accidents and sports activities.8–10 These injuries have an impact on the quality of life of patients by impairing chewing, phonation, esthetics, as well as their physical and psychological condition.7,11,12
Knowledge of TDI characteristics is important for the establishment of preventive action and treatment so as to reduce associated costs and improve the population's quality of life.9,12 This study aims to identify the characteristics and factors associated with TDI in patients treated at a specialized service for a ten-year period.
Material and methodsThe present cross-sectional retrospective study was reviewed and approved by an Institutional Research Ethics Committee for Human Beings (protocol n. 049/2007). Records of patients treated at an Oral and Maxillofacial Surgery Department (Pelotas, south of Brazil) during a ten-year period were evaluated. Patients with DAT records in permanent teeth were included in the study, but those with incomplete records or showing other kinds of injury were excluded.
After researcher calibration, data were collected and transferred in duplicate to a table specifically created for the study. The collected variables were age, gender, cause of trauma, presence and type of dislocation, tooth fracture and bone plate fracture. Data were analyzed by means of descriptive statistics, and the chi-square test at 95% significance level was performed; when the null hypothesis was rejected, complex analysis to verify the association between variables was carried out.
ResultsAfter collection, 545 records of patients treated at the service were included in the study, 387 of whom (71.0%) were male and 158 (29.0%) female. As to age, there was an average of 20.77±12.04 years, and the study included patients ranging from six to 63 years, with a median of 17 years.
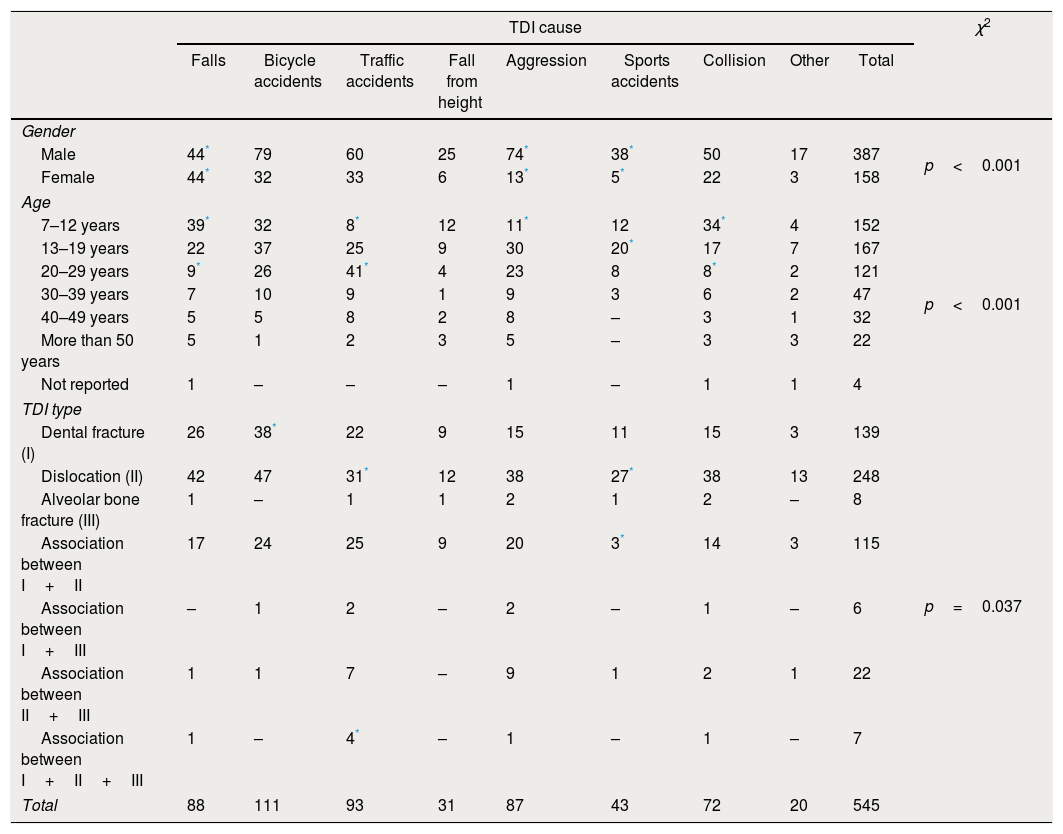
The prevailing age group was between 13 and 19 years (30.6%), followed by 6–12 years (27.9%) and 20–29 years (22.2%). The most common etiologies were bicycle (20.4%) and traffic (16.9%) accidents, falls (16.1%) and aggression (16.0%) (Table 1).
Distribution of TDI cause according to gender, age, TDI type. Chi-square association test and complex analysis.
| TDI cause | χ2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Falls | Bicycle accidents | Traffic accidents | Fall from height | Aggression | Sports accidents | Collision | Other | Total | ||
| Gender | ||||||||||
| Male | 44* | 79 | 60 | 25 | 74* | 38* | 50 | 17 | 387 | p<0.001 |
| Female | 44* | 32 | 33 | 6 | 13* | 5* | 22 | 3 | 158 | |
| Age | ||||||||||
| 7–12 years | 39* | 32 | 8* | 12 | 11* | 12 | 34* | 4 | 152 | p<0.001 |
| 13–19 years | 22 | 37 | 25 | 9 | 30 | 20* | 17 | 7 | 167 | |
| 20–29 years | 9* | 26 | 41* | 4 | 23 | 8 | 8* | 2 | 121 | |
| 30–39 years | 7 | 10 | 9 | 1 | 9 | 3 | 6 | 2 | 47 | |
| 40–49 years | 5 | 5 | 8 | 2 | 8 | – | 3 | 1 | 32 | |
| More than 50 years | 5 | 1 | 2 | 3 | 5 | – | 3 | 3 | 22 | |
| Not reported | 1 | – | – | – | 1 | – | 1 | 1 | 4 | |
| TDI type | ||||||||||
| Dental fracture (I) | 26 | 38* | 22 | 9 | 15 | 11 | 15 | 3 | 139 | p=0.037 |
| Dislocation (II) | 42 | 47 | 31* | 12 | 38 | 27* | 38 | 13 | 248 | |
| Alveolar bone fracture (III) | 1 | – | 1 | 1 | 2 | 1 | 2 | – | 8 | |
| Association between I+II | 17 | 24 | 25 | 9 | 20 | 3* | 14 | 3 | 115 | |
| Association between I+III | – | 1 | 2 | – | 2 | – | 1 | – | 6 | |
| Association between II+III | 1 | 1 | 7 | – | 9 | 1 | 2 | 1 | 22 | |
| Association between I+II+III | 1 | – | 4* | – | 1 | – | 1 | – | 7 | |
| Total | 88 | 111 | 93 | 31 | 87 | 43 | 72 | 20 | 545 | |
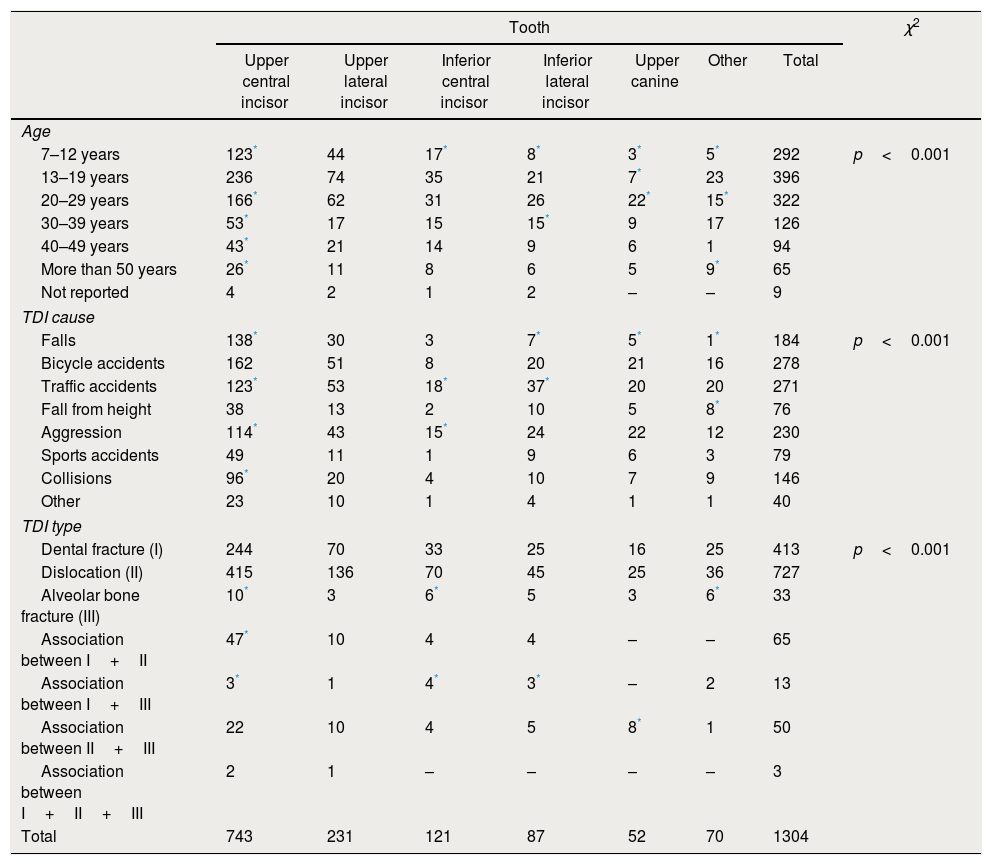
The 545 patients included in the study had a total of 1304 teeth affected by TDI, an average of 2.39±1.69 teeth per patient. Twelve was the maximum number of affected teeth in one isolated patient, with four cases. The most affected dental elements were the maxillary central incisors (57.0%), followed by upper lateral incisors (17.7%), lower central incisors (9.3%) and lower lateral incisors (6.7%) (Table 2).
Distribution of affected tooth according to age, TDI cause and TDI type. Chi-square association test and complex analysis.
| Tooth | χ2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Upper central incisor | Upper lateral incisor | Inferior central incisor | Inferior lateral incisor | Upper canine | Other | Total | ||
| Age | ||||||||
| 7–12 years | 123* | 44 | 17* | 8* | 3* | 5* | 292 | p<0.001 |
| 13–19 years | 236 | 74 | 35 | 21 | 7* | 23 | 396 | |
| 20–29 years | 166* | 62 | 31 | 26 | 22* | 15* | 322 | |
| 30–39 years | 53* | 17 | 15 | 15* | 9 | 17 | 126 | |
| 40–49 years | 43* | 21 | 14 | 9 | 6 | 1 | 94 | |
| More than 50 years | 26* | 11 | 8 | 6 | 5 | 9* | 65 | |
| Not reported | 4 | 2 | 1 | 2 | – | – | 9 | |
| TDI cause | ||||||||
| Falls | 138* | 30 | 3 | 7* | 5* | 1* | 184 | p<0.001 |
| Bicycle accidents | 162 | 51 | 8 | 20 | 21 | 16 | 278 | |
| Traffic accidents | 123* | 53 | 18* | 37* | 20 | 20 | 271 | |
| Fall from height | 38 | 13 | 2 | 10 | 5 | 8* | 76 | |
| Aggression | 114* | 43 | 15* | 24 | 22 | 12 | 230 | |
| Sports accidents | 49 | 11 | 1 | 9 | 6 | 3 | 79 | |
| Collisions | 96* | 20 | 4 | 10 | 7 | 9 | 146 | |
| Other | 23 | 10 | 1 | 4 | 1 | 1 | 40 | |
| TDI type | ||||||||
| Dental fracture (I) | 244 | 70 | 33 | 25 | 16 | 25 | 413 | p<0.001 |
| Dislocation (II) | 415 | 136 | 70 | 45 | 25 | 36 | 727 | |
| Alveolar bone fracture (III) | 10* | 3 | 6* | 5 | 3 | 6* | 33 | |
| Association between I+II | 47* | 10 | 4 | 4 | – | – | 65 | |
| Association between I+III | 3* | 1 | 4* | 3* | – | 2 | 13 | |
| Association between II+III | 22 | 10 | 4 | 5 | 8* | 1 | 50 | |
| Association between I+II+III | 2 | 1 | – | – | – | – | 3 | |
| Total | 743 | 231 | 121 | 87 | 52 | 70 | 1304 | |
Concerning TDI, 1438 injuries were observed, among which dental dislocations were found in 55.8% of cases alone, whereas 9.0% were associated with dental and/or bone fractures. Dental fractures occurred isolatedly in 31.7% of cases whereas in 6.2% of them were associated to other kinds of injuries. Alveolar bone fractures occurred in isolation in 2.5% of cases as contrasted to 1.2% associated with tooth fractures or dislocations (Table 2).
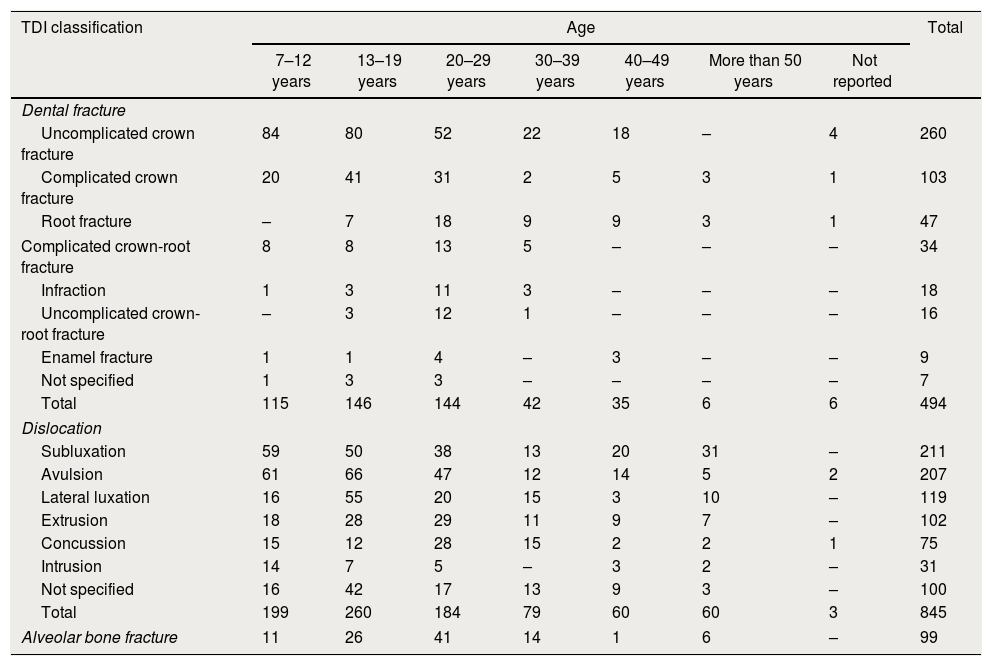
Among dental fracture types, uncomplicated crown (52.6%) and complicated crown (20.9%) were the most frequent. As to dislocation, subluxation and avulsion occurred most frequently, with 25.0% and 24.5% respectively (Table 3).
Distribution between age and TDI classification.
| TDI classification | Age | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 7–12 years | 13–19 years | 20–29 years | 30–39 years | 40–49 years | More than 50 years | Not reported | ||
| Dental fracture | ||||||||
| Uncomplicated crown fracture | 84 | 80 | 52 | 22 | 18 | – | 4 | 260 |
| Complicated crown fracture | 20 | 41 | 31 | 2 | 5 | 3 | 1 | 103 |
| Root fracture | – | 7 | 18 | 9 | 9 | 3 | 1 | 47 |
| Complicated crown-root fracture | 8 | 8 | 13 | 5 | – | – | – | 34 |
| Infraction | 1 | 3 | 11 | 3 | – | – | – | 18 |
| Uncomplicated crown-root fracture | – | 3 | 12 | 1 | – | – | – | 16 |
| Enamel fracture | 1 | 1 | 4 | – | 3 | – | – | 9 |
| Not specified | 1 | 3 | 3 | – | – | – | – | 7 |
| Total | 115 | 146 | 144 | 42 | 35 | 6 | 6 | 494 |
| Dislocation | ||||||||
| Subluxation | 59 | 50 | 38 | 13 | 20 | 31 | – | 211 |
| Avulsion | 61 | 66 | 47 | 12 | 14 | 5 | 2 | 207 |
| Lateral luxation | 16 | 55 | 20 | 15 | 3 | 10 | – | 119 |
| Extrusion | 18 | 28 | 29 | 11 | 9 | 7 | – | 102 |
| Concussion | 15 | 12 | 28 | 15 | 2 | 2 | 1 | 75 |
| Intrusion | 14 | 7 | 5 | – | 3 | 2 | – | 31 |
| Not specified | 16 | 42 | 17 | 13 | 9 | 3 | – | 100 |
| Total | 199 | 260 | 184 | 79 | 60 | 60 | 3 | 845 |
| Alveolar bone fracture | 11 | 26 | 41 | 14 | 1 | 6 | – | 99 |
The chi-square association test was statistically significant upon crossing all categories of variables (p≤0.05), except for gender and age (p=0.06), gender and dental element (p=0.57), gender and TDI type (p=0.42), and age and TDI type (p=0.65). Tables 1 and 2 include variable crossings that showed statistically significant associations, as well as complex analysis which highlight the associated pairs of variables.
Regarding the cause of trauma, statistical analysis mainly demonstrates a positive association between male patients with aggression, falls and sport accidents; age (7–12 years) with falls and collisions; age (13–19 years) with sports accidents; age (20–29 years) with traffic accidents; dental fractures with bicycle accidents; and dislocations with traffic and sports accidents (Table 1).
Concerning the involved tooth in trauma, upper central incisors were associated all ages, except 13–19 years which was associated with upper canines. About cause, upper central incisors had association with falls, traffic accidents, aggression and collisions; inferior central incisors with traffic accidents and collisions; and lateral inferior incisors with traffic accidents (Table 2).
DiscussionThe present retrospective study was conducted at a permanent tooth trauma monitoring and treatment center of a public institution service. Patients treated in this service are usually forwarded to Emergency Hospitals due to facial injuries. TDI cross-sectional studies allow monitoring higher age and gender prevalence, in addition to the association between different TDI and causing factors.7,9
A male prevalence at a 2.4:1 ratio was found. This finding is supported by other research in the literature, and it is agreed that boys play sports and high risk competitions of intense contact; in adult men, in turn, TDI is additionally related to traffic accidents and aggression.9,13,14 In this study, an association between gender and cause was also found, inasmuch as men, regardless of age, showed TDI due to falls, aggression and sports.
One of the major TDI risk factors is age, and the most affected age group consists of children and adolescents.1–3 The high number of injuries in this population can be explained by their daily activity characteristics, with great time spent in recreation and sports.15 In this retrospective study, 58.5% of cases were reported in patients between six and 19 years of age. The average age of 20.77 years observed in the study was similar to that found in literature.7,16
The cause–age association showed that children aged seven to 12 years suffer TDI by fall, collision with objects, traffic accidents and aggression, in this order. Falls and collisions are major causes related to school recreational activities.17 In these cases, preventive actions are rare and difficult to implement.16 However, aggression cases can be accounted for by school fights and domestic violence, and the evaluation of these patients is essential to the identification of likely domestic aggression and its report to authorities.18 The main etiology for teenagers between 13 and 19 was associated to sports, which is also in agreement with that described in literature, and reinforces the need to use mouth guards to prevent these injuries.5,19
Dental dislocations were the most prevalent TDI type, being present in 64.8% of cases. This type of TDI occurs mainly in children and adolescents6,20 due to anatomical characteristics during the phase of mixed dentition and facial growth.5 In this period, the periodontal ligament space is increased, being a dislocation predisposition and, since the mandible has not its fully developed yet, there may be lack of lip seal and excessive incisor exposure. In this study, 54.3% of dental dislocations affected patients of up to 19 years.
Higher impact etiologies are related to a greater transmission of forces to supporting tissues, dental dislocations and bone fractures.16 Medical records of the evaluated patients showed an association between bicycle accidents and dental fractures, traffic accidents with dental and bone fractures, and sports accidents with either isolated dislocations or associated with dental fractures. Thus, in the face of TDI due to higher impact accidents, injuries to the periodontal tissues should be investigated, since they show greater severity and a worse prognosis.7,13
As to TDI classification, infraction, enamel fracture and uncomplicated crown fracture accounted for only 19.9% of all injuries. The high prevalence of other lesions with pulp and/or supporting tissue involvement can be explained by the characteristics of the evaluated service. Because it is an institutional public care TDI specific service, less severe cases are resolved in the public health network, without the need for referral. Among dental elements, the results found in this study are in agreement with those in literature, which point to upper incisors as the most usually affected teeth.3,13
The knowledge of dental trauma epidemiology has an important role in clinical treatment of those injuries. According to patient profile (age, gender and cause of trauma) the attendance may be prepared for the most associated diagnosis and involved teeth. Thus, it may improve the early treatment and prognosis of the injuries.
Considering the limitations of a retrospective analysis conducted at a single TDI-referral center, TDI prevalence in children and adolescents was found along a ten-year period due to falls, collisions and traffic and sports accidents. Most TDI showed an involvement of supporting and/or pulp tissues, the upper central incisor being the most affected tooth.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare no conflict of interest.