The continuous development of medicine in most fields requires physicians to apply the latest methods and technology to ensure patients’ safety. In the field of anesthesiology we are pioneers in the application of measures that guarantee the security of our patients, making possible the greatest reduction in mortality seen among all other specialties. This objective has been achieved thanks to the introduction of changes such as the one presented in this review article.
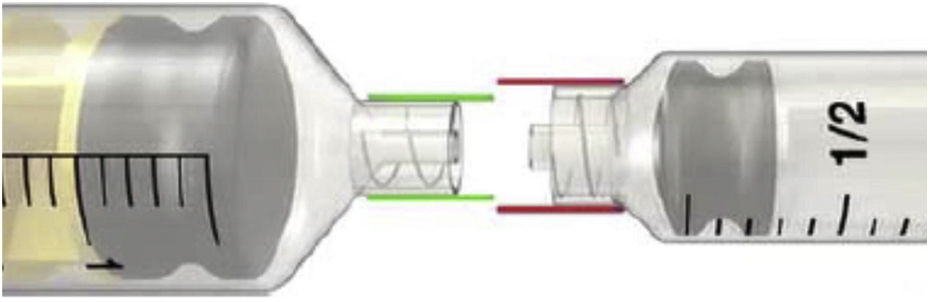
The specific NRFit® connections for neuraxial and other regional anesthesia applications prevent wrong route medication errors to occur. These medication errors have been related to a high morbidity and mortality rate. This article reviews this new technology based in our own two-year experience at Hospital Universitario Príncipe de Asturias (Alcalá de Henares, Madrid) as well as a literature review using PubMed, UpToDate and ClinicalKey.
El continuo avance de la medicina en todos los campos requiere por parte de los médicos la aplicación de métodos y tecnología que hagan de la seguridad del paciente una garantía. En el campo de la anestesiología somos pioneros en la aplicación de medidas que garantizan la seguridad, haciendo posible la mayor reducción en la mortalidad de entre las observadas en el resto de las especialidades. Este objetivo se ha logrado gracias a la introducción de cambios como el que presenta este artículo de revisión.
Las conexiones modificadas NRFit® permiten la administración de fármacos destinados a bloqueos nerviosos, haciendo practicamente imposible los errores de medicación por infusión a través de un acceso equivocado, de gran morbimortalidad. Este artículo revisa esta nueva tecnología, ya obligatoria en otros países de nuestro entorno, desde la experiencia de más de dos años de uso en el Hospital Universitario Príncipe de Asturias (Alcalá de Henares, Madrid) y una búsqueda bibliográfica en PubMed, UpToDate y ClinicalKey.