Even though laparoscopic nephrectomy improves the quality of postoperative recovery, it still causes moderate to severe pain. Our objective was to determine whether serratus intercostal plane block (SIPB) was noninferior to posterior quadratus lumborum block (QLB) in terms of pain control and quality of recovery.
MethodsThis multicentre, controlled, randomized, blinded study had a sample size of 120 patients who were randomly assigned to SIPB, QLB, and control groups prior to scheduled laparoscopic nephrectomy. We collected the following variables: postoperative dynamic pain scores at 0, 6, 12, and 24 h, postoperative quality of recovery (QoR15), and total opioid consumption (fentanyl and morphine).
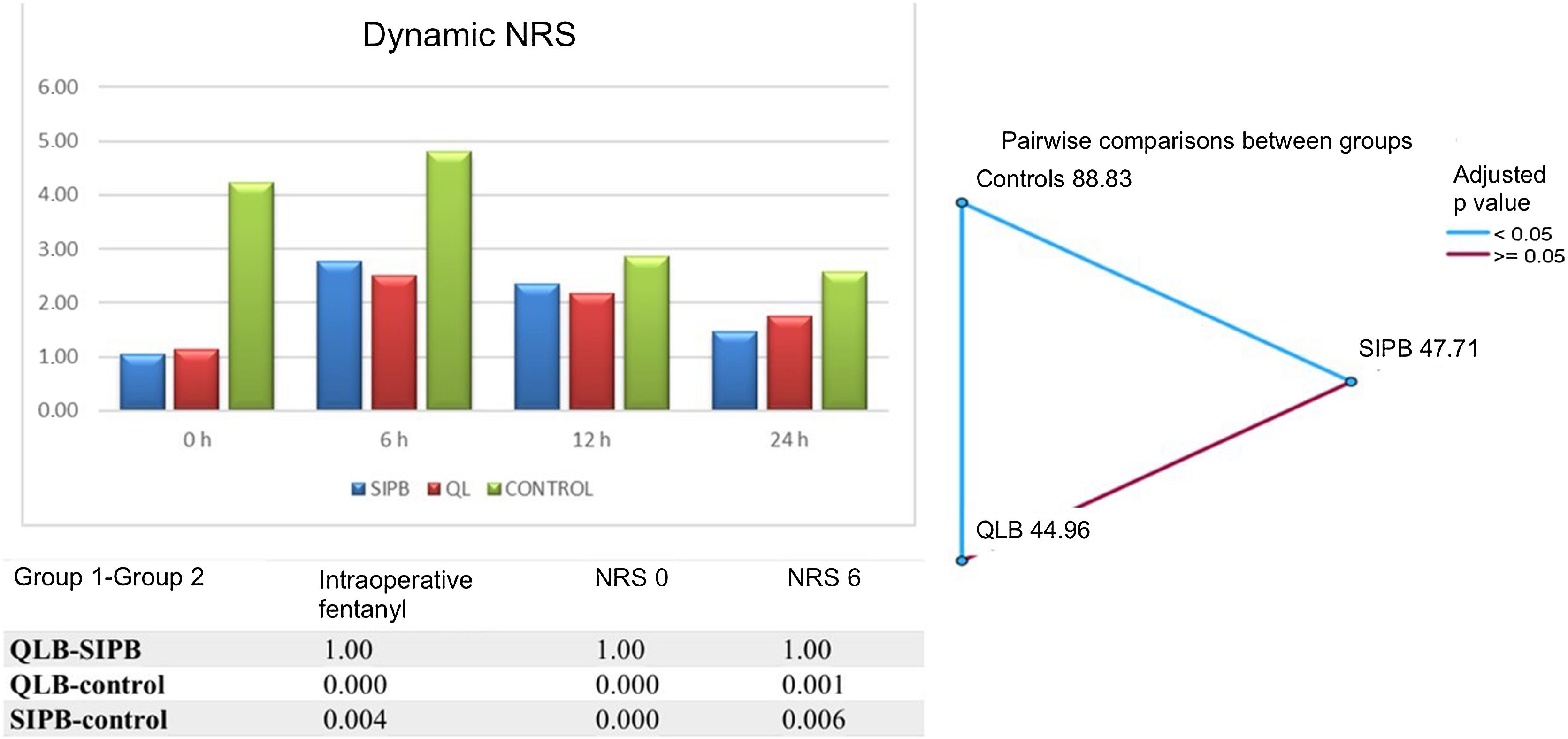
ResultsOur results show that SIPB was non-inferior to QLB with regard to the primary endpoint (NRS 0.4/0.9) and quality of recovery (QoR15 112.7/106.85) (p 0.27). Opioid consumption (fentanyl p 0.37 and morphine p 0.9) was similar in the SIPB and QLB groups, and both groups were superior to controls in terms of intraoperative fentanyl consumption (p 0.001) and pain control (p < 0.001).
ConclusionsSIPB and QLB showed adequate postoperative pain control, good quality of recovery and lower fentanyl consumption, especially compared to the control group.
La nefrectomía laparoscópica ha mejorado la calidad de la recuperación postoperatoria de los pacientes. Sin embargo, esta cirugía sigue causando dolor moderado-intenso. Nuestro objetivo fue determinar si el bloqueo del plano serrato intercostal (BSPI) era no inferior al bloqueo cuadrado lumbar posterior (BCL) en términos de control del dolor y calidad de la recuperación.
MétodosEste estudio multicéntrico, controlado, aleatorizado y ciego tuvo un tamaño muestral calculado de 120 pacientes. Se asignó aleatoriamente a los pacientes a los grupos BPSI, QLB y control antes de la nefrectomía laparoscópica programada. Se evaluaron las puntuaciones de dolor dinámico postoperatorio de los pacientes a las 0, 6, 12 y 24 horas, la calidad postoperatoria de la recuperación (QoR15) y el consumo total de opiáceos (fentanilo y morfina).
ResultadosLos resultados del estudio muestran la no inferioridad de SIPB frente a QLB sobre el objetivo principal (dolor NRS 0,4/0,9) o la calidad de la recuperación (QoR15 112,7/106,85) (p 0,27). BPSI y QLB mostraron un consumo de opioides similar (fentanilo p 0,37 y morfina p 0,9). Ambos grupos fueron superiores al grupo control en cuanto a fentanilo intraoperatorio (p 0,001) y control del dolor (p < 0,001).
ConclusionesBPSI y QLB mostraron un adecuado control del dolor postoperatorio, una buena calidad de la recuperación y ahorro de fentanilo, especialmente en comparación con el grupo control.
Nephrectomy can be performed using either an open or laparoscopic technique, but laparoscopy has a faster recovery time, less morbidity, less blood loss and less pain. Despite this, some patients continue to suffer moderate to severe postoperative pain.
Although opioids are highly effective, they are often used sparingly due to their side effects. The use of regional techniques within a multimodal strategy appears to reduce the need for opioids,1 and some of these techniques provide good pain management and rapid postoperative recovery in patients scheduled for laparoscopic nephrectomy. In this study, we analysed 2 of these techniques, the posterior quadratus lumborum block (posterior QLB) and the serratus intercostal plane block (SIPB).
The posterior QLB2 has proven efficacy in lower abdominal surgery, and can sometimes be as effective as epidural anaesthesia in controlling postoperative pain in laparoscopic nephrectomy.3
The SIPB has been described as the gold standard analgesic technique in open cholecystectomy, and its indications have now been extended to include upper abdominal incision surgery, including open nephrectomy, where it is an effective opioid-sparing strategy that promotes good postoperative recovery.4
The primary objective of this prospective randomized study was to evaluate whether SIPB was non-inferior to posterior QLB in pain control and quality of postoperative recovery. Both techniques were compared with a control group that only received intravenous analgesia. Secondary outcome measures were opioid consumption (intraoperative fentanyl and postoperative morphine at 24 h) and side effects. We also evaluated the difficulty in performing each block as a subjective parameter.
Material and methodThis prospective, randomized, controlled, double-blind study was performed in various hospitals in Spain (Río Hortega University Hospital, Clinical University Hospital, Burgos University Hospital, Costa del Sol Hospital, and A Coruña University Hospital Complex). After obtaining approval from the ethics committee (Ceim Valladolid Est: CASVE NM-20-434) on 6 February 2020 and from the AEMPS (Spanish Agency of Medicines and Health Devices) with EudraCT No. 2020-000779-19, we prospectively registered the protocol in Clinical trials. gov: Identifier: NCT04431388 on 11 June 2020. Given the exceptional circumstances in hospitals between March 2020 and September 2021, recruitment restarted after the pandemic (1 October 2021). During this latency period, the results from the first patients (lack of obvious postoperative benefit compared with not applying new techniques) compelled us to consider adding a control group to the protocol, as this would allow us to compare the results of both techniques with a group of patients receiving standard analgesia. We submitted the amendments and they were accepted by the ethics committee.
Patients undergoing laparoscopic nephrectomy, aged over 18 years, American Society of Anesthesiology (ASA) class I-III were included. Written informed consent was obtained from all patients. Exclusion criteria were allergy to the. study drugs, contraindication for the study nerve blocks (coagulopathy, infection at the injection site, etc.), chronic pain and emergency surgery.
The primary objective of this noninferiority trial was to evaluate whether pain management in the first 24 postoperative hours in the SIPB group was noninferior to the QLB group. For this purpose, we used the sealedenvelope.com online calculator for binary outcome non-inferiority trials. Assuming that there is a true difference of 5% (90% vs 85%) in favour of standard treatment (QLB), 72 patients (36 per group) would be required to be 90% confident that the upper limit of a one-sided 95% confidence interval (or two-sided 90% confidence interval) will exclude a difference of more than 28% in favour of the standard group. The mean NRS score recorded in patients with QLB in a previous study (3.35) was taken as a reference value.5 Considering a potential dropout rate of 10%, we included 40 patients in each group to achieve a statistical power of 90% and a bilateral α error of 0.05. We decided later to add a control cohort of 40 patients, since the main objective of the study was to compare both regional techniques. This brought the final sample size to 120 patients.
Patients were randomized to 3 groups (allocation ratio 1:1:1) using an online random number generator. This ratio was written down and placed in an opaque envelope. Patients were added to each group until we obtained the required number. The patients, the evaluator, and the statistician were blinded to the analgesia technique used. Only the anaesthesiologist who performed the techniques knew each patient’s group, but they were not involved in intraoperative anaesthesia management or data collection.
All patients gave their informed, signed consent to receive anaesthesia and participate in the study. On the day of surgery, before the intervention, each patient’s demographic data (age, sex, ASA class) were collected. Monitoring included electrocardiogram, pulse oximetry, noninvasive blood pressure, the bi-spectral index (BIS™) and the GE Healthcare neuromuscular transmission module. General anaesthesia was induced with intravenous midazolam (0.03 mg/kg), fentanyl (1 µg/kg), propofol (2 mg/kg) and rocuronium (0.6 mg/kg), and orotracheal intubation was performed. Anaesthesia was maintained with inhaled sevoflurane in a mixture of oxygen and fresh air to maintain a BIS index between 40 and 60. Rocuronium bromide was administered if the patient presented 2 or 3 train-of-four (TOF) twitches, and a bolus of fentanyl (100 µg) was administered if haemodynamic parameters (heart rate and mean arterial pressure) increased by 20% over preoperative baseline. All patients received 8 mg IV dexamethasone after induction and 1 g IV paracetamol and 4 mg IV ondansetron 30 min before the end of surgery. During the postoperative period, all 3 groups received IV dexketoprofen 50 mg/8 h intravenously and IV paracetamol 1 g/6 h. Rescue analgesia consisted of patient-controlled intravenous infusion (PCA) with morphine in all 3 groups and patients were taught how to self-administer analgesia as required (adding 1 bolus if the NRS was > 5 and the patient presented functional impairment). The PCA device consisted of 0.5 mg/mL of morphine and was programmed as follows: 4 mL bolus dose and 15 min lockout interval)
Our patients were divided into 3 groups: SIPB, QLB and controls.
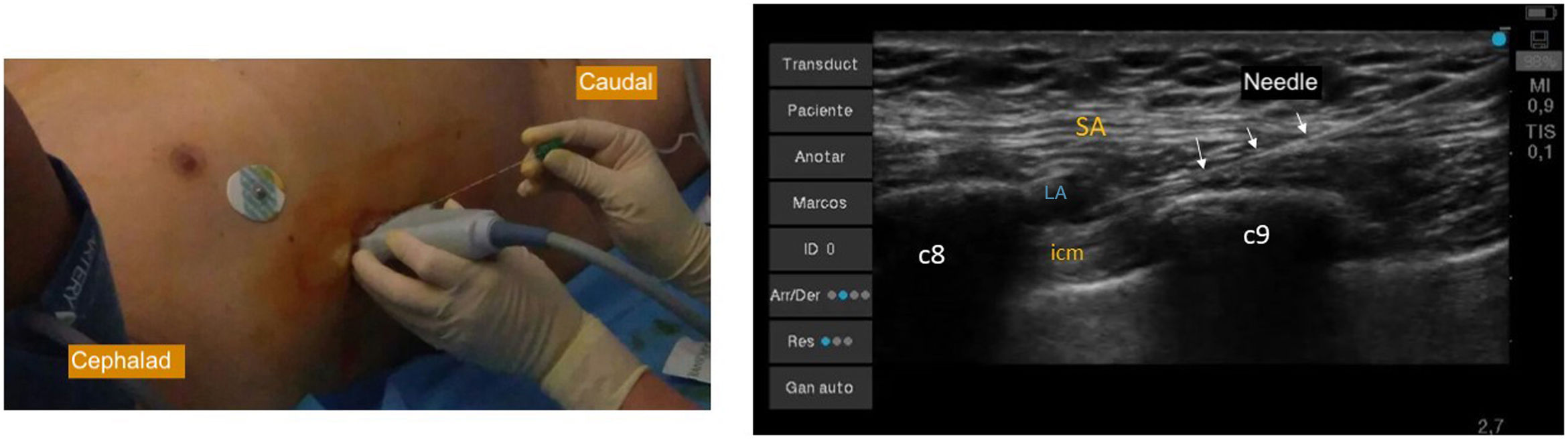
SIPB group: The low serratus intercostal plane block was performed after induction with the patient either supine or in lateral decubitus. A portable ultrasound system (Edge II Sonosite® Bothell WA, USA) with a high-frequency (6−15 Hz) linear transducer placed in a sagittal plane on the midaxillary line was used to identify thoracic structures. After swabbing the injection site, a 90 mm AKUS PRO® needle (AKUS innovation, Murcia, Spain) was inserted in-plane in a caudocranial direction. When the needle tip reached the plane between the serratus anterior and external intercostal muscles at the level of the eighth rib, a 20 mL bolus of 0.25% levobupivacaine plus 4 mg dexamethasone was administered and the spread of the injectate was monitored on ultrasound (Fig. 1).
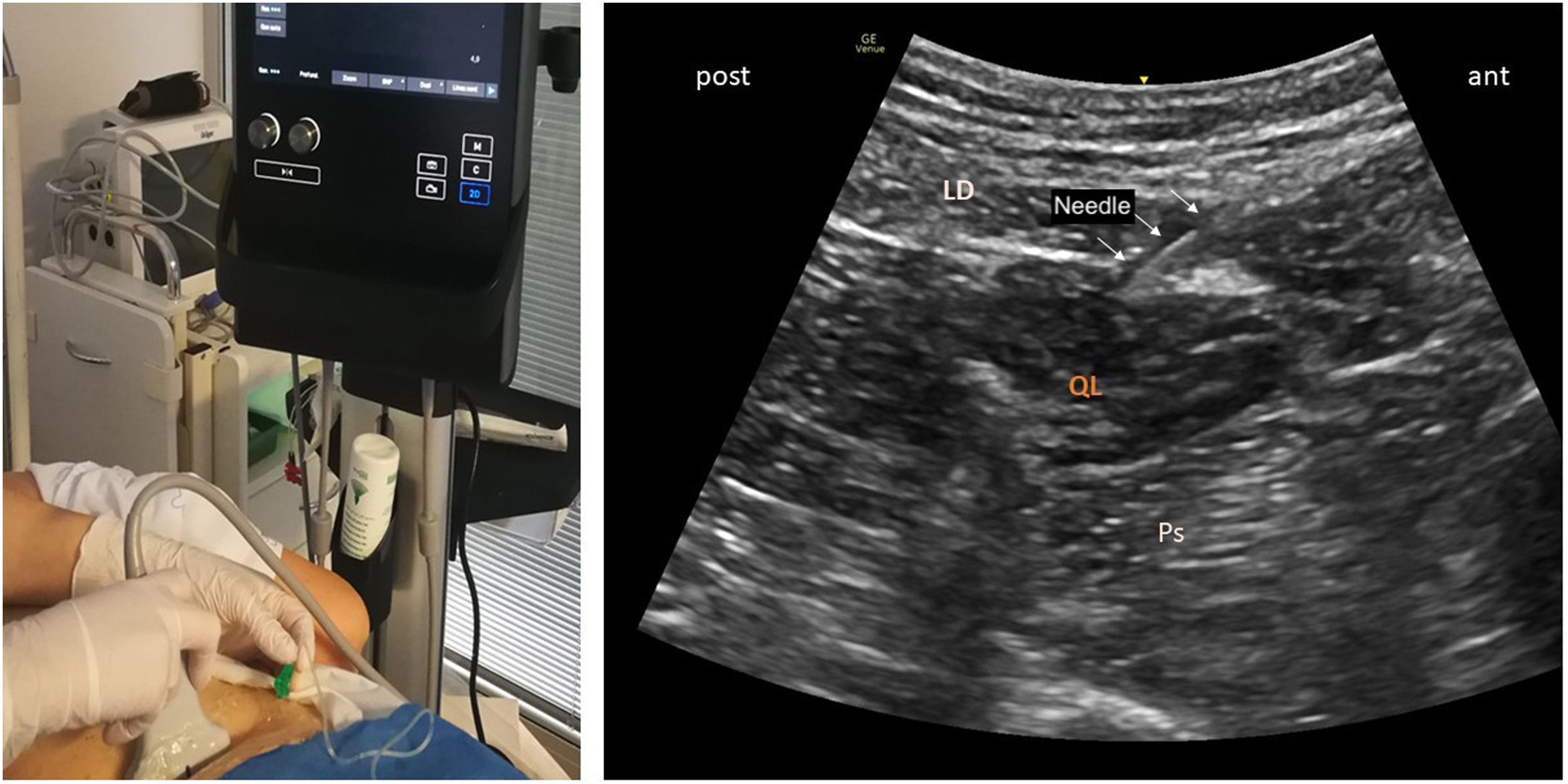
QLB group: With the patient in the lateral decubitus position, a convex transducer was placed on the lateral abdominal wall at the level of L3-4. After identifying the muscles of the abdominal wall, the probe was moved posterolaterally until the quadratus lumborum and latissimus dorsi muscles were identified. After swabbing the injection site, the needle was introduced 90 mm anteriorly until reaching the posterior surface of the quadratus lumborum muscle, where 20 mL of 0.25% levobupivacaine plus 4 mg dexamethasone was administered between the QL muscle and the thoracolumbar fascia using the in-plane technique (Fig. 2).
Control group: Patients assigned to the control group received intravenous analgesia only, including PCA morphine in the postoperative period.
A specific NRS questionnaire was designed to record dynamic pain (coughing, deep breathing, movement, etc.) on a scale of 0 (no pain) to 10 (worst pain imaginable). These questionnaires were administered at 0, 6, 12 and 24 postoperative hours. Other outcomes recorded were quality of recovery using the modified (15-item) QoR15 surgical recovery scale, which was administered 24 h after surgery, and opioid consumption (intraoperative fentanyl and postoperative morphine at 24 h). Nerve blocks were performed by anaesthesiologists with extensive experience in regional anaesthesia, and the questionnaires were administered by the staff in charge of each operating room and the postoperative care unit (PACU), who were blinded to the analgesia technique.
Regional techniques were compared with controls who received only intravenous analgesia. All date are presented as mean ± SD. Pain (NRS) was assessed using a nonparametric test after using the Kolmogorov Smirnov test to confirm that the values were not normally distributed. The QoR15 scores were analysed as continuous variables. The following non-parametric tests were used: Kruskal Wallis for independent samples, Friedman for dependent samples, and one-factor ANOVA for parametric samples. Secondary outcome measures (intraoperative fentanyl and cumulative morphine consumption) were analysed using noninferiority tests and posthoc tests with a significance level of 5%. The rescue morphine dose, the number of additional analgesics used, and the frequency of PONV were analysed using the Wilcoxon rank sum test with a significance level of 5%. The 95% confidence intervals (95% CI) for median differences in the NRS score and postoperative morphine dose were calculated using the Hodges-Lehman estimator. The Friedman test and Bonferroni correction were used for multiple comparisons. Probability (P) values less than α 0.05 were considered significant and differences between groups were identified. All statistical analyses were performed using SPSS for Windows version 22.
Variables recorded in the regional technique groups were compared, and the results of each comparison were then compared with controls (no regional technique).
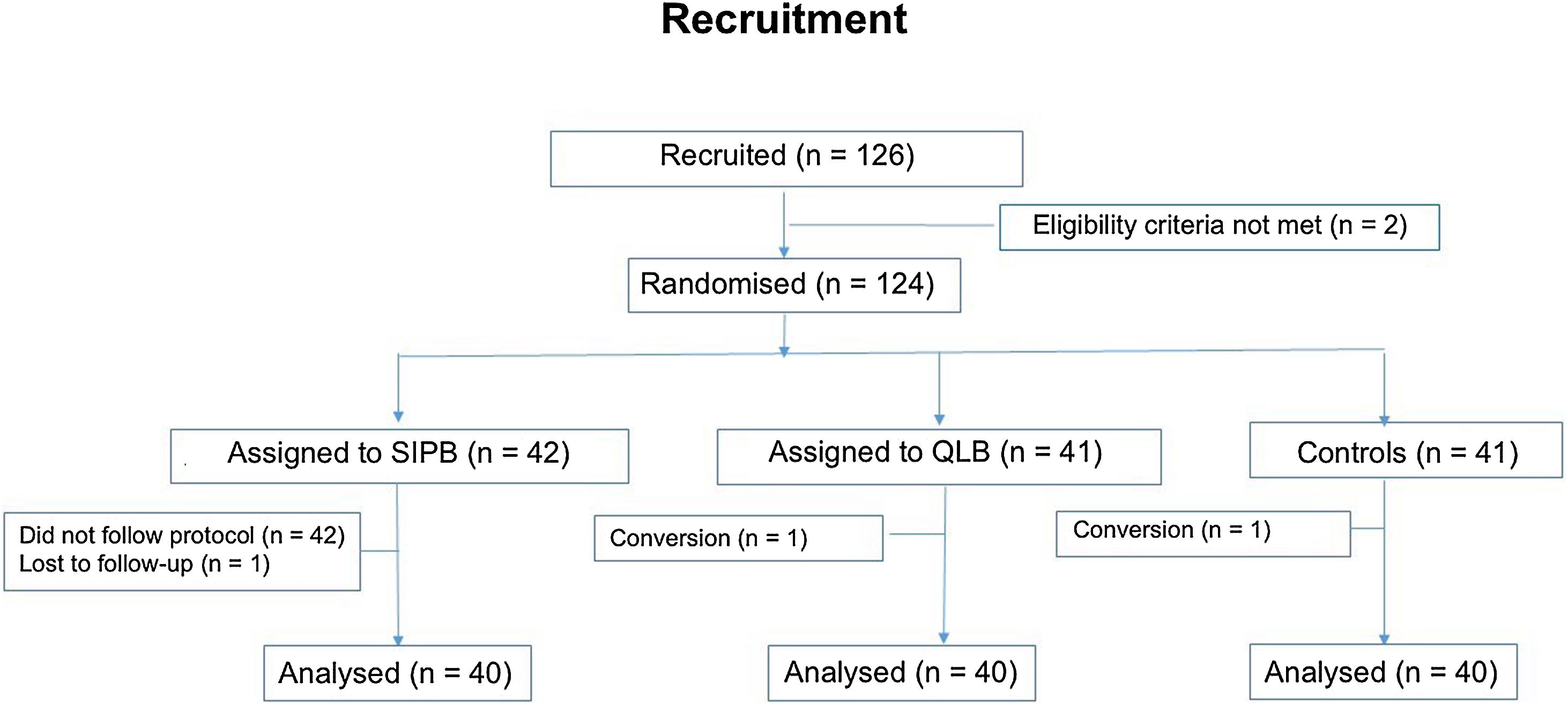
ResultsAlthough the study started in 2020, data collection was complicated by the pandemic and the impact it had on hospitals. For this reason, the study was discontinued and restarted in October 2021. By December 2023, we had enrolled and randomized 126 patients, excluding those recruited before the pandemic. Fig. 3 shows the CONSORT (Consolidated Standards of Reporting Trials) guidelines.
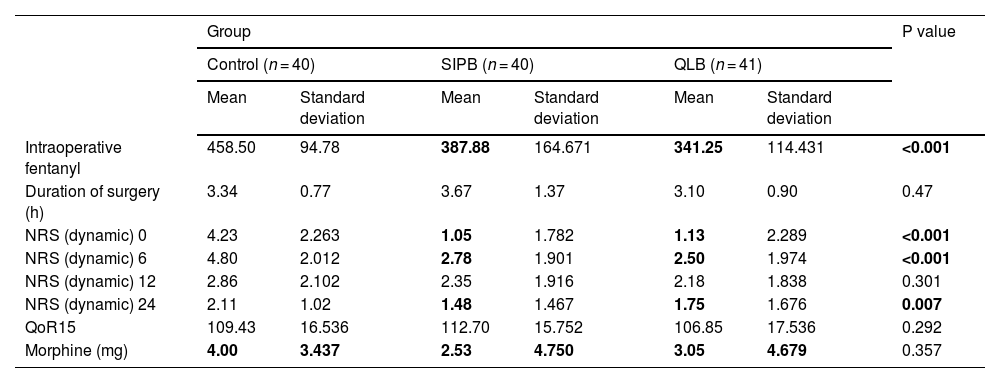
We analysed 120 patients scheduled for laparoscopic nephrectomy. Groups were evenly distributed in terms of sex (SIPB 24/16; QLB 22/19; controls 24/16) (p 0.7) and mean age (SIPB 67.03 ± 9.92 years; QLB 63.78 ± 12.83; controls 65.53 ± 10.17) (p 0.43). Most patients were ASA II (SIPB 76.2%; QLB 65%; controls 77.8%) (p 0.63), and the primary outcome measure (dynamic pain management) did not differ significantly between groups. SIPB for pain management was non-inferior to QLB, with NRS scores at 0 (SIPB 1.4, QLB 1.13; 95% CI [p 0.875]), 12 (SIPB 2.35; QLB 1.8), and 24 (BPSI 1.6; QLB 1.55) hours, and quality of recovery QoR15 (BPSI 112 ± 15; QLB 106 ± 85) (p 0.278). The median test for independent samples showed similar results. There were no significant differences in secondary outcome measures between regional anaesthesia groups. Intraoperative fentanyl (SIPB 363 µ ± 147; QLB 327µ ± 112) and postoperative morphine (SIPB 3.43 mg ± 5.9; QLB 3.5 mg ± 5.5) consumption was similar in both groups. The Mann Whitney U test found no differences between variables (p 0.604) (Table 1).
Outcome measures (pain: NRS, recovery quality: QoR15 and opioid use).
| Group | P value | ||||||
|---|---|---|---|---|---|---|---|
| Control (n = 40) | SIPB (n = 40) | QLB (n = 41) | |||||
| Mean | Standard deviation | Mean | Standard deviation | Mean | Standard deviation | ||
| Intraoperative fentanyl | 458.50 | 94.78 | 387.88 | 164.671 | 341.25 | 114.431 | <0.001 |
| Duration of surgery (h) | 3.34 | 0.77 | 3.67 | 1.37 | 3.10 | 0.90 | 0.47 |
| NRS (dynamic) 0 | 4.23 | 2.263 | 1.05 | 1.782 | 1.13 | 2.289 | <0.001 |
| NRS (dynamic) 6 | 4.80 | 2.012 | 2.78 | 1.901 | 2.50 | 1.974 | <0.001 |
| NRS (dynamic) 12 | 2.86 | 2.102 | 2.35 | 1.916 | 2.18 | 1.838 | 0.301 |
| NRS (dynamic) 24 | 2.11 | 1.02 | 1.48 | 1.467 | 1.75 | 1.676 | 0.007 |
| QoR15 | 109.43 | 16.536 | 112.70 | 15.752 | 106.85 | 17.536 | 0.292 |
| Morphine (mg) | 4.00 | 3.437 | 2.53 | 4.750 | 3.05 | 4.679 | 0.357 |
When comparing the results of patients in the SIPB and QLB groups with controls, statistically significant differences (significance level 0.5) were observed at the 95% CI in intraoperative fentanyl consumption (458 µ controls vs. 387µ/341 µ in SIPB/QLB) and in pain scores within the first 6 postoperative hours: NRS 0 h (4.23/1.05 and 1.13) (p 0.000) and NRS 6 h (4.28/2.78 and 2.5) (p 0.000). However, there were no differences in pain scores at 12 h (p 0.301), quality of recovery QoR15 (p 0.292) or postoperative morphine consumption (p 0.351) (Fig. 4).
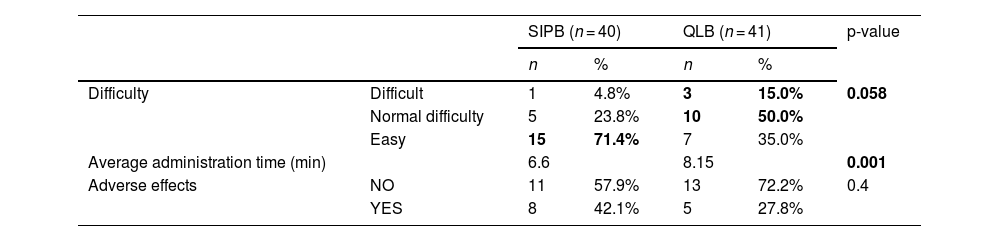
Operator-perceived difficulty in performing the technique and the time taken showed a statistically significant difference in favour of the SIPB, which was easy to perform (p-value 0.058 in the Pearson Chi-square test) and took 6.6 min compared to 8.15 min for the QLB (Table 2). None of the techniques showed significant side effects.
DiscussionLaparoscopic techniques are now preferred over open techniques in kidney surgery because they are less traumatic, present fewer complications, and facilitate recovery.5 The key to a speedy recovery is multimodal analgesia, since post-nephrectomy pain is multifactorial. Our results show that fascial blocks are a good option for controlling somatic pain. Intraoperative opioid consumption was similar in the SIPB and QLB groups, but was lower in both nerve block groups compared with controls.
Laparoscopic nephrectomy pain has a somatic and visceral component (irritation of the diaphragm, visceral nociception and ureteral colic) and an inflammatory component caused by the release of inflammatory mediators in response to surgical stress.6 In multimodal anaesthesia, nonsteroidal anti-inflammatory drugs should be used with caution due to their renal metabolism.6,7 In this type of surgery, central and chest wall blocks have been used to block innervation of the incisional dermatomes (T7-12), visceral innervation (kidney T8-L1 and ureters T10-12) and diaphragmatic irritation. The paravertebral block has been used successfully in the context of general anaesthesia.8 There are some reports in the literature describing the use of spinal anaesthesia in robotic and laparoscopic nephrectomy, even allowing robotic surgery to be performed in awake patients.9 However, the side effects associated with these techniques should not be overlooked.
The use of ultrasound to guide regional anaesthesia has led to the description of new blocks, some of which can be used in laparoscopic nephrectomy. Among these, the transverse abdominis plane (TAP) block has given poor results,10 but the quadratus lumborum block (QLB) has been widely used. Aditianingsih et al.11 report that coverage of the QLB extended from T9 to L2 dermatomes, including those associated with the Pfannenstiel incision (T12-L1). The analgesic effect was sufficient to control surgical wound pain, and was associated with a lower incidence of complications than epidural analgesia. Theoretically, this technique could produce somatic and visceral analgesia due to the spread of the local anaesthetic in the paravertebral space, which prolongs the analgesic effect for 6−48 h and achieves similar visceral pain relief to epidural blockade.12 In their review of 12 randomized controlled clinical trials with a total of 821 patients, however, Wang et al.13 concluded that a single injection provided a significant, but not clinically relevant, analgesic improvement in the recovery of patients undergoing nephrectomy.
After reading the article published by Corso et al.,14 we decided to investigate whether SIPB was an analgesic option, as it was not inferior to a technique that had already shown efficacy.
In our study, we compared the efficacy of administering local anaesthetic (LA) in the serratus intercostal plane (blockade of the lower intercostal nerves T7-11) with LA administration in the posterior aspect of the quadratus lumborum muscle (spread through the thoracolumbar fascia). To avoid the bias of technical difficulty, we chose 2 superficial nerve blocks: the posterior QLB, which has proven efficacy,15 and the SIPB. Data from previous studies showed that the SIPB effectively anaesthetises the upper abdominal wall (subcostal approach) in open nephrectomy.16,17 In Onay et al.,18 morphine consumption (20.45 mg) in patients undergoing open nephrectomy under QLB was far higher than that observed in patients undergoing similar procedures under SIPB (4.17 mg).17
The results of our study show that intraoperative consumption of fentanyl in both regional anaesthesia groups (SIPB and QLB) was low, suggesting than these techniques were successful in managing intraoperative stress. Dam et al.,19 however, reported savings in postoperative, but not intraoperative, opioids. The results obtained with both techniques are similar, although anaesthesiologists find SIPB easier and faster to perform than QLB. Our data show that SIPB is a more superficial block that is easy to administer and has a low learning curve. It provides adequate analgesia with a single shot, is not associated with any complications (unlike QL20,21), and achieves an average QoR15 score of 112 ± 15, which is close to the good quality standard.
This study has several limitations. We originally designed a study with 2 experimental groups in which we tried to avoid biases (selection, application, etc.), but then decided to include a control group. To do this, we matched our controls with the 2 other groups and included the same number of patients; however, we cannot be certain to have avoided bias. This may have affected the differences in the results obtained in the control group and the experimental groups, but not the differences observed between the experimental groups. Some hospitals were only able to recruit a small number of patients for various reasons; therefore, recruitment was uneven across the hospitals involved. Regarding the “ease of administration” parameter, which was rated by each anaesthesiologist, we attempted to compensate for the subjectivity of this rating by quantifying the time required to administer both nerve blocks.
ConclusionsOur study shows that SIPB was not inferior to QLB in pain management, and is easier to administer. SIPB and posterior QLB administered before the surgical incision in patients undergoing laparoscopic nephrectomy are associated with lower intraoperative fentanyl consumption and adequate postoperative pain control compared with the control group.
FundingThe authors report that the sponsor was not involved in this investigation, and has not influenced the findings of this study.
The authors certify that there is no conflict of interest with any financial organization in relation to the material discussed in the manuscript.
The authors would like to express their gratitude for the efforts made by the entire team that collaborated on the study, for their tenacity in not giving up despite the circumstances. This article was made possible thanks to the support for research provided by the awards received for the work on intercostal serratus plane block (ISPB) at ESRA Europe and ESRA Spain.