Liver transplantation (LT) has an incidence of intraoperative cardiopulmonary arrest (CPA) of around 5%. Patients who experience CPA during this procedure have a reduced survival rate of approximately 50%.
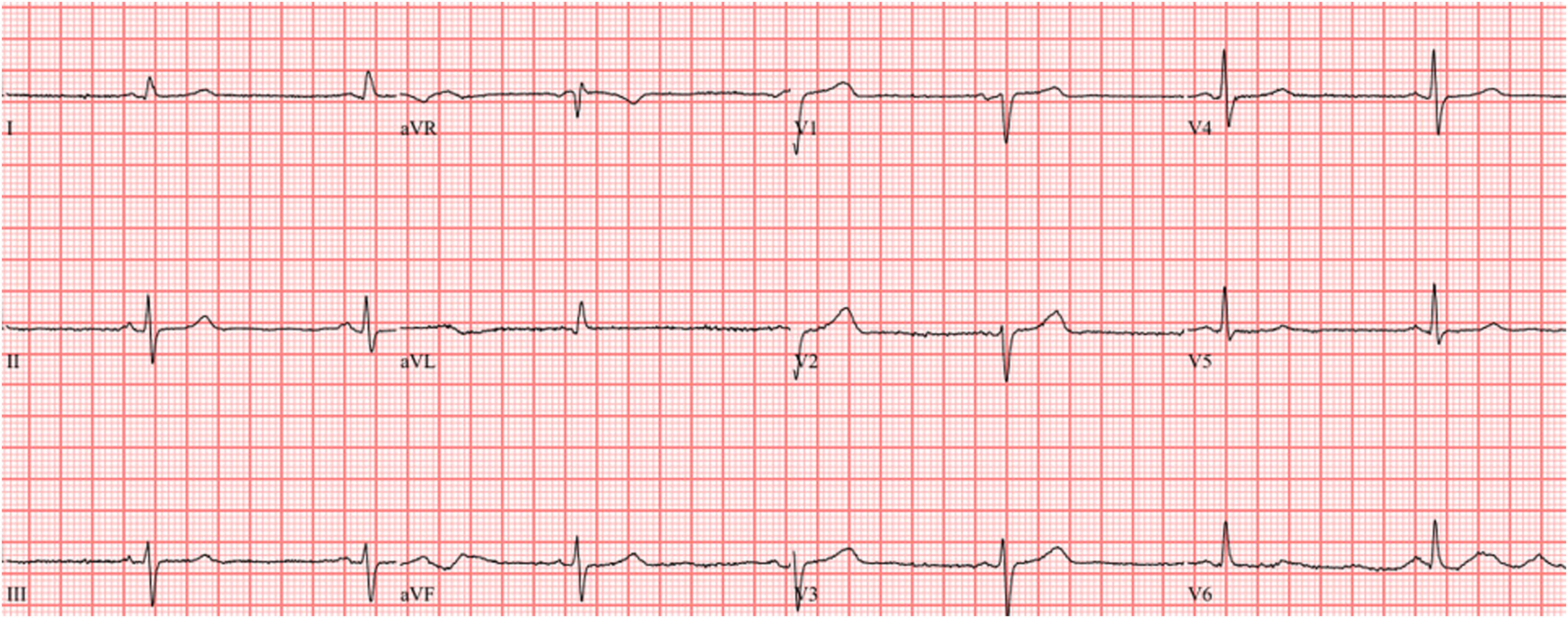
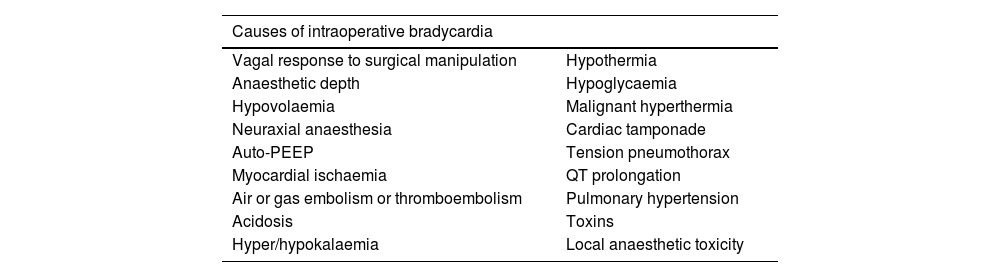
Most CPAs occur during the neohepatic phase due to reperfusion syndrome, but this is not always the underlying cause, and a broad differential diagnosis must be performed.
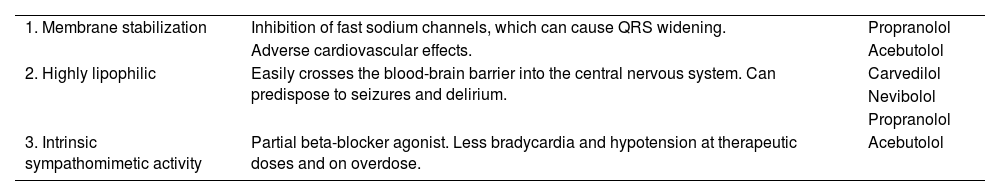
We introduce the case of a cirrhotic patient who received beta-blocker therapy in the preoperative period and who experienced intraoperative CPA during LT surgery, which was successfully resolved through advanced cardiopulmonary resuscitation (CPR) maneuvers and specific treatment for beta-blocker toxicity (calcium and glucagon).
La cirugía de trasplante hepático (TH) presenta una incidencia de parada cardiorrespiratoria (PCR) intraoperatoria en torno al 5%. Los pacientes que sufren PCR durante dicha intervención presentan una supervivencia reducida cercana al 50%.
La mayoría de PCR se producen en la fase neohepática debido al síndrome de reperfusión, pero no siempre es esta la causa subyacente y debemos realizar un diagnóstico diferencial amplio.
Presentamos el caso de un paciente cirrótico en tratamiento con betabloqueantes que presentó PCR durante el TH, de la que se recuperó tras reanimación cardiopulmonar (RCP) avanzada y tratamiento específico para la toxicidad por betabloqueantes (calcio y glucagón).