Bipolar disorder (BD) has been related to various cognitive dysfunctions as well as to a high prevalence of metabolic syndrome (MS), which seems to influence the cognitive performance of patients with BD. Therefore, different hypotheses have been generated to try to explain the pathophysiological relationship between cognitive deficit in BD and MS. The objective was to review the current literature regarding the possible pathophysiological explanation of the relationship between BD and MS and its effect on cognitive performance of patients with BD.
MethodsA bibliographic search was carried out using MEDLINE, ClinicalKey, EMBASE, Literatura Latino-Americana y del Caribe en Ciencias de la Salud [Latin American and Caribbean Literature in Health Sciences] (LILACS), APA PsycNet, Scopus and Scielo databases, and the Pan-American Medical Electronic Library; using the following search terms: “bipolar disorder”[MeSH Terms] OR “bipolar disorder”[All Fields] OR “mood disorders”[All Fields] AND “cognitive deficit”[MeSH Terms] OR “cognitive deficit”[All Fields] OR “cognitive dysfunction”[All Fields] OR “cognitive impairment”[All Fields] OR “cognitive decline”[All Fields] AND “metabolic syndrome” [MeSH Terms] OR “metabolic abnormalities”[All Fields] OR “metabolic effects”[All Fields] OR “obesity” [All Fields] OR “abdominal obesity” [All Fields] OR “overweight” [All Fields] OR “diabetes” [All Fields] OR “hypertension” [All Fields] AND “antipsychotics” [MeSH Terms] OR “antipsychotics”[All Fields] AND “antidepressants” [MeSH Terms] OR “antidepressants”[All Fields] AND “mood stabilizers” [MeSH Terms] OR “mood stabilizers”[All Fields]. Filters: free full text, full text, from 2001 to 2022. A total of 80 articles in Spanish and English, of any type of design, were selected. Selection and reading were carried out by all the authors.
Results and conclusionsThe various pathophysiological hypotheses proposed, inflammatory, endocrine, drug, environmental and social, suggest that a series of changes at the macro and microcellular level are correlated in patients with BD and MS with a negative effect on cognition of patients both globally and in specific domains, mainly executive function, memory, attention, and perceptual motor skills. Research processes should be continued to explore the various hypotheses that support the relationship between BD, MS and cognition.
El trastorno bipolar (TB) se ha relacionado con diversas disfunciones cognitivas y una alta prevalencia de síndrome metabólico (SM), el cual parece influir en el desempeño cognitivo de los pacientes con TB, por lo que se han generado diferentes hipótesis para tratar de explicar la relación fisiopatológica entre el déficit cognitivo en el TB y el SM. El objetivo es revisar la literatura en busca de las posibles explicaciones fisiopatológicas de la relación entre TB y SM y su efecto en el desempeño cognitivo de los pacientes con TB.
MétodosSe realizó una búsqueda bibliográfica utilizando las bases de datos MEDLINE, ClinicalKey, EMBASE, Literatura Latino-Americana y del Caribe en Ciencias de la Salud (LILACS), APA PsycNet, Scopus y Scielo, y la librería electrónica Médica Panamericana; se utilizaron los siguientes términos de búsqueda: “bipolar disorder”[MeSH Terms] OR “bipolar disorder”[All Fields] OR “mood disorders”[All Fields] AND “cognitive deficit”[MeSH Terms] OR “cognitive deficit”[All Fields] OR “cognitive dysfunction”[All Fields] OR “cognitive impairment”[All Fields] OR “cognitive decline”[All Fields] AND “metabolic syndrome” [MeSH Terms] OR “metabolic abnormalities”[All Fields] OR “metabolic effects”[All Fields] OR “obesity” [All Fields] OR “abdominal obesity” [All Fields] OR “overweight” [All Fields] OR “diabetes” [All Fields] OR “hypertension” [All Fields] AND “antipsychotics” [MeSH Terms] OR “antipsychotics”[All Fields] AND “antidepressants” [MeSH Terms] OR “antidepressants”[All Fields] AND “mood stabilizers” [MeSH Terms] OR “mood stabilizers”[All Fields] Filters: Free full text, Full text, from 2001-2022. Se seleccionaron en total 80 artículos en español y en inglés, de cualquier tipo de diseño. Todos los autores efectuaron la selección y la lectura.
Resultados y conclusionesLas diversas hipótesis fisiopatológicas descritas (inflamatoria, endocrina, medicamentosa, ambiental y social) plantean que una serie de cambios macrocelulares y microcelulares se correlacionan en los pacientes con TB y SM con un efecto negativo en la cognición de los pacientes, tanto general como en dominios específicos, principalmente función ejecutiva, memoria, atención y habilidades perceptuales motoras. Deben continuarse los procesos de investigación que permitan explorar las diversas hipótesis que sustentan la relación entre TB, SM y cognición.
Bipolar disorder (BD) is episodic, with a variable, recurrent and chronic course, characterised by alternating episodes of mania or hypomania and depression. It affects over 1% of the world’s population and is associated with a decrease in life expectancy and an increase in premature deaths related to suicide and chronic medical conditions such as metabolic syndrome (MS) and premature cardiovascular disease.1–8
MS includes a group of clinical, biochemical and metabolic abnormalities, such as abdominal obesity, insulin resistance, arterial hypertension and dyslipidaemia, the pathophysiological mechanism of which is not fully understood. It is diagnosed using the criteria of different groups and associations such as the International Diabetes Federation (IDF), the American Association of Clinical Endocrinologists (AACE), the World Health Organization (WHO) and the European Group for the Study of Insulin Resistance (EGIR).6,8–16
International studies have shown a high prevalence of MS in patients with BD,8–10,12,17–19 with rates ranging from 16% to 67%.5,8,12,17 The association between BD and MS has a significant influence on the clinical presentation of BD (it is more severe and difficult to treat12,17,20–22) and, it would seem, on the cognitive deficit observed in these patients and their prognosis.
Cognitive deficit is the deterioration of mental processes related to thinking, learning and memory; it can be identified using different psychometric tests that help us calculate the capacity for abstract thinking, assimilation and logical reasoning, and by measuring the IQ and other higher cortical functions, such as language, execution of orders, recognition of objects and construction of figures.23,24
Patients with BD have various cognitive deficits that often even extend to periods of remission or euthymia and are reflected in the patient's performance in different neuropsychological tests and in IQ scores. These deficits have been associated with a poorer quality of life, impaired psychosocial functioning, difficulties at work and in social situations and a higher mortality rate.2,4,6,9,14,17–29
In recent years, there has been an increasing interest in understanding the mechanisms by which cognitive dysfunction occurs in BD.30 However, little attention has been given to the relationship between MS and neurocognition in patients with BD.25 Our aim with this article has therefore been to search the current literature for possible pathophysiological explanations of the relationship between BD and MS and its effect on the cognitive performance of patients with BD.
MethodsWe conducted a literature search in the databases of MEDLINE, ClinicalKey, EMBASE, LILACS (Literatura Latino-Americana y del Caribe en Ciencias de la Salud) [Latin American and Caribbean Literature on Health Sciences], APA PsycNet, Scopus and Scielo, and the digital library of Editorial Médica Panamericana, using the following terms: bipolar disorder; bipolar affective disorder; mood disorder; mania; euthymia; metabolic syndrome; obesity; hypertension; diabetes; cognitive function; cognitive dysfunction; neurocognitive dysfunction; cognitive impairment; and executive dysfunction; and the connectors AND and OR between each of the terms. After that, we selectively reviewed primary sources of information such as scientific articles, books, publications, degree theses and works. We did not use secondary sources of information, such as compilations, summaries or proceedings of expert conferences. We only reviewed articles in Spanish and English published in the last 20 years.
Cognitive disorders in patients with bipolar disorderBD has been classified worldwide as one of the main causes of cognitive deficit-related disability, which is observed from before the first manifestation of symptoms and during all phases of the disorder, including euthymia.12,31–36 Although not all patients with BD suffer from cognitive problems, approximately 40%–60% of patients suffer some degree of deficit, which can vary from mild to severe, depending on the results of different neuropsychological tests.37 The deficit includes alterations in attention, memory, verbal skills (ability to learn, order, relate and reason information through spoken language) and executive functions (mental activities of planning, organising and regulating a task, ability to do several activities at once and to adjust attention quickly to various stimuli).12,25,32–34,38–41
During the manic phase, cognitive deficits are more noticeable; the more severe the mania, the worse the domain scores.42 Attention is one of the most affected, followed by alterations in tasks involving concept formation and executive function.13,35,43,44 In the depressive phase, poor performance is evident in decision-making tasks, problem-solving strategies and concept formation, as well as decreased sensitivity to detect stimuli, reaction speed and working memory.13,35,44–46
During euthymia, a decrease in attention and verbal and psychomotor response, memory failures and executive dysfunction can be observed.13,20,26,44,45 These deficits are reported to persist during periods of remission and, although they usually remain at a subsyndromal level, they can become clinically significant in 5%–35% of patients.34,40,42,47,48 However, additional short- and long-term follow-up studies are required in order to assess the course of cognitive impairment in patients with BD.
Cognitive disorders in patients with bipolar disorder and metabolic syndromeIn patients with BD and MS, worse neurocognitive performance has been observed, both general and in specific domains, compared to those without MS.8,18,20,21,25,26,49,50 A recent study conducted in patients with BD found a relationship between MS and decreased performance in executive function (Cohen’s d = 0.52; 95% confidence interval [95% CI], 0.16–0.90), memory (d = –0,57; 95% CI, –0.92 to –0.22) and perceptual motor skills (d = –0.39; 95% CI, –0.76 to –0.03) after adjusting for confounding factors such as age, gender, education and psychopharmacological treatment.51
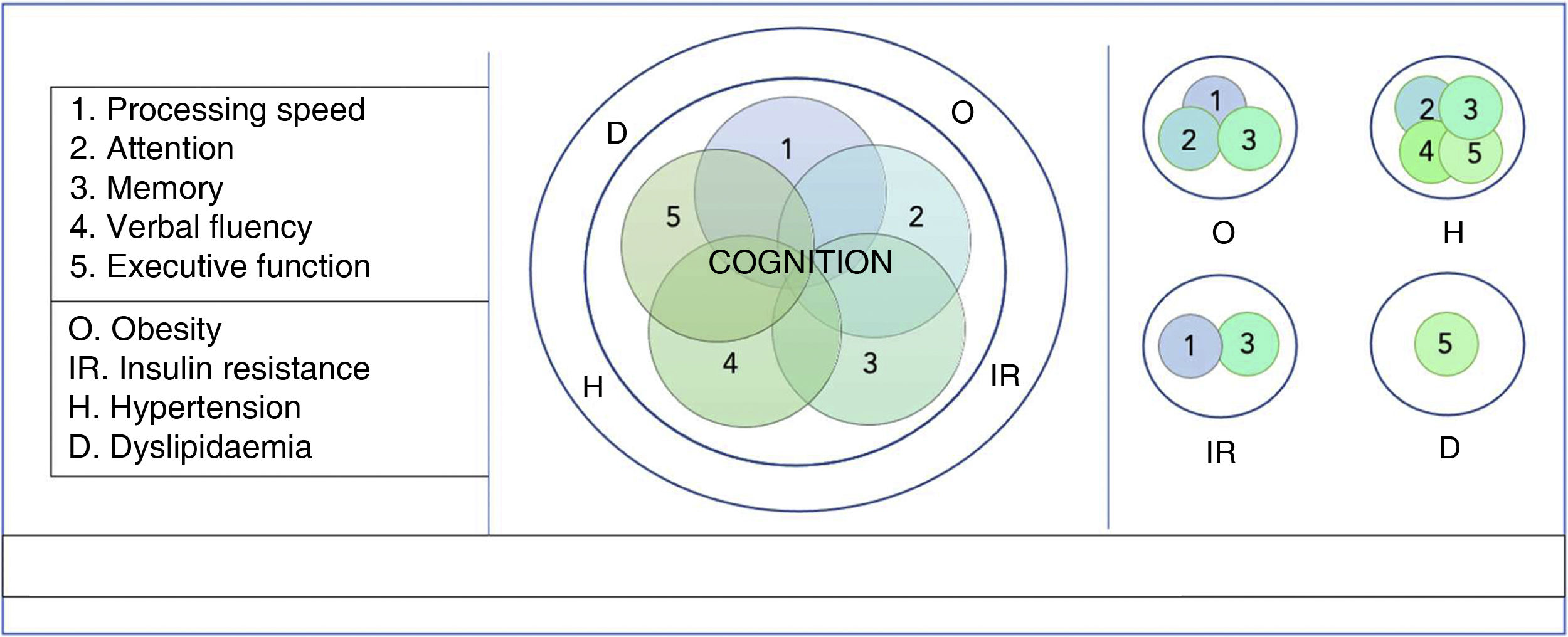
Current evidence indicates that each of the components of MS (abdominal obesity, insulin resistance, hypertension and dyslipidaemia) has a negative effect on the cognition of patients with BD8,25,52,53 (Fig. 1). Obesity is the most studied of these components and has been related to both cognitive deficit overall and alterations in processing speed, attention and memory.8,20,25,33,49,50,53–56 Insulin resistance has been associated with an accelerated decline in memory and processing speed and with lower scores on the Mini-Mental State Examination (MMSE).21,52,57 High blood pressure has been linked to poorer performance in verbal fluency and memory, executive functions and attention.14,18,19 Dyslipidaemia, mainly dystriglyceridaemia, has been associated with impaired executive function in patients with BD.25
HypothesisEndocrine hypothesisSeveral neuroendocrine abnormalities have been associated with MS and its development in patients with BD, including hypothalamic–pituitary–adrenal axis hyperactivity, hypothalamic-pituitary-thyroid axis disruption, cortisol dysregulation and glucocorticoid resistance. When the hypothalamic–pituitary–adrenal axis is activated, in addition to an increase in adrenocorticotropic hormones, there is an increase in the production and release of cortisol, a counter-regulatory hormone to insulin that plays an important role in the increase of circulating lipids, the redistribution and accumulation of visceral fat in the abdominal region, the inhibition of the peripheral use of glucose, the activation of gluconeogenesis and the increase in adrenaline and noradrenaline concentrations.8,16,43,46
The hypersecretion of cortisol has been observed in all phases of BD (mania, depression and euthymia), with the consequent development of the above-mentioned changes. These changes have been associated, first of all, with being overweight and abdominal obesity, which are in turn associated with atrophy of various cortical and subcortical structures, and of frontal regions that mediate executive function, learning, memory and decision-making.12,20,49,55,58 Secondly, they have been associated with hyperglycaemia, insulin resistance, hyperlipidaemia and hypertension linked to hippocampal atrophy, reduction in amygdala size, neuronal injury, loss of brain tissue and alterations in the structure, composition and function of cerebral blood vessels. All of the above, individually and synergistically, have been associated with decreased processing speed, executive dysfunction, poorer verbal fluency and, consequently, decreased cognitive performance.9,12,22,39,54,55,58–61
Alterations in the hypothalamic-pituitary-thyroid axis have frequently been found in patients with BD, and are linked to the development of depressive or manic symptoms in the different phases of the disorder and to a poorer response to treatment and shorter duration of remission. In turn, thyroid hormones have been associated with a variety of metabolic changes in the body, such as vascular endothelial dysfunction and dyslipidaemia, which could be linked to the development of MS in patients with BD.62
Inflammatory hypothesisAbnormalities in the immune system are another potential explanation for the association between BD, MS and cognitive deficit. Studies conducted in recent years have evaluated the central and peripheral markers of oxidative stress and inflammation and have shown that changes in the production of proinflammatory cytokines during the different phases of BD (mania, depression and euthymia)9,22,63,64 and a variation in the expression of proinflammatory markers such as C-reactive protein, tumour necrosis factor alpha and interferon gamma, may not only interfere with the action of insulin on hepatic glucose and lipid metabolism, but also contribute towards glucocorticoid resistance through direct effects on the expression and function of the glucocorticoid receptor and, in turn, on the development of MS and cognitive deficit.9,12,39,55,63 Based on these results, a correlation between inflammation, MS and cognitive deficit in patients with BD has been proposed. However, the results have been inconclusive and even contradictory at times.63,64
In 2013, an observational cross-sectional study was conducted with 41 patients with Bipolar 1 Disorder (BD1) in the different phases of the disease and 11 control subjects, in which the concentrations of 10 peripheral inflammatory factors were determined. A tendency towards a decrease in the serum concentrations of interleukin 2 and an increase in interleukin 4 were observed in the group of patients in the depressive phase compared to those with mania, euthymia and control, but without statistically significant differences between the concentrations of these and the other interleukins or the tumour necrosis factor.63 Another study conducted that same year described deterioration in the domains of memory, language and attention in patients with BD who had a higher expression of adipokines and C-reactive protein.39 These are inflammatory markers involved in oxidative stress, alteration in the metabolism of carbohydrates, lipids and proteins, insulin resistance in skeletal muscle and adipose tissue, and impaired secretion of insulin by the beta cells of the pancreas, with the consequent development of MS.65
Drug hypothesisThe side effects of psychotropic medications contribute to increased rates of MS in patients with BD by inducing changes in serotonergic, adrenergic, dopaminergic and histaminergic receptors in the centre of the hypothalamus that controls hunger and satiety. These changes lead to increased calorie intake, with consequent weight gain, an overproduction of ApoB-100, hyperlipidaemia, insulin resistance, diabetes and an increase in substances such as leptin, free fatty acids, adiponectin, tumour necrosis factor alpha and resistin.8,9,49,51,66–68
Antidepressants with antihistamine effect, such as tricyclics and mirtazapine, have been associated with abdominal obesity, reduction in high-density lipoproteins (HDL) and increased prevalence of MS (PR = 2.17; 95% CI, 1.24–3.80; p = 0.007).18,69 Lithium carbonate and valproic acid are associated with a significant weight gain (13% and 21% respectively) and effects on glucose metabolism and insulin resistance. Lithium carbonate, in particular, the first-choice for a mood stabiliser in BD, has been shown to lead to an increase in glucose uptake by adipocytes and the stimulation of appetite in some patients22 and to mild negative effects on immediate verbal learning, memory and psychomotor performance in patients with BD in the euthymic phase.36,70–72 Alterations in fatty acid metabolism and verbal memory deficits have been found with valproic acid.70,71 Less specific negative effects on cognition have been described with carbamazepine and topiramate,71,72 while no effects have been shown on cognition or the development of MS with lamotrigine.72,73
Antipsychotics are a treatment option for patients with BD, either as a monotherapy or in combination with mood stabilisers, and are the main contributors to weight gain, hyperlipidaemia, diabetes and MS.74 The rate of MS in patients treated with several antipsychotics is 50%, whilst in those treated with only one it is 34.3% (p = 0.015).68 Clozapine and olanzapine are the antipsychotics most associated with the development of MS, with weight gains ranging from 4 to 10 kg after starting the therapy, followed by quetiapine and risperidone, with weight gains from 2 to 4 kg, but the findings are variable with respect to alteration of lipids and carbohydrates.51,66,74,75 Although antipsychotics appear to improve cognition in the early course of the disease by counteracting the detrimental effects of the mental illness, in the long term, by increasing their effect on metabolism, their continued use could have a negative impact on cognitive functions, especially when administered at high doses or in combined treatments.18,22,36,76 However, further long-term studies are required in order to better understand the impact of antipsychotics on the neurocognitive functioning of patients with BD.41,72
Environmental and social hypothesisExposure to an adverse early environment, poverty, social isolation, malnutrition and poor education, which according to epidemiological studies have a high prevalence in patients with BD, has been associated with increased susceptibility to developing MS.55 Similarly, traumatic experiences in childhood, and a history of physical, emotional or sexual abuse, have been linked not only to the risk of mood disorders and development of BD, but also to a significant negative impact on metabolic health and an increased risk of obesity, insulin resistance, type 2 diabetes mellitus (DM2) and MS in adulthood, with the subsequent development of premature cardiovascular disease and a deterioration in cognitive function.55
Lifestyle factors have also been linked to weight gain and obesity in patients with BD. Poor eating habits, with high-calorie diets rich in refined carbohydrates, as well as processed foods and physical inactivity, are common in this group of patients, and in turn contribute to the alteration of inflammatory profiles and the subsequent development of MS, with its consequences on both cardiovascular and cognitive health.39,51,55
Smoking, a common habit in patients with BD, with a rate of 35.2% compared to 12.8% in the general population, has been described as a risk factor for multiple diseases and is related to impairments in insulin function, increased metabolic risk and poorer cognitive performance.51 A study published in January 2015 and conducted with 363 patients with BD reported worse cognitive performance in smokers, with a negative association between pack-years and general cognitive performance.39
Chronic stress, one of the most important known triggers of affective episodes in patients with BD, generates multiple adaptive changes as part of a compensatory mechanism. The burden of these changes in the body is known as “allostatic load”, the impact of which is evident not only in the different systems of the body, such as the cardiovascular and neuroendocrine systems—in which the glucose and lipid metabolism are affected, leading to obesity, insulin resistance, interruption in lipid regulation and finally MS—but also in the brain, as changes occur in brain volume, along with impairment of attention, memory and visuospatial function.18,55,77,78
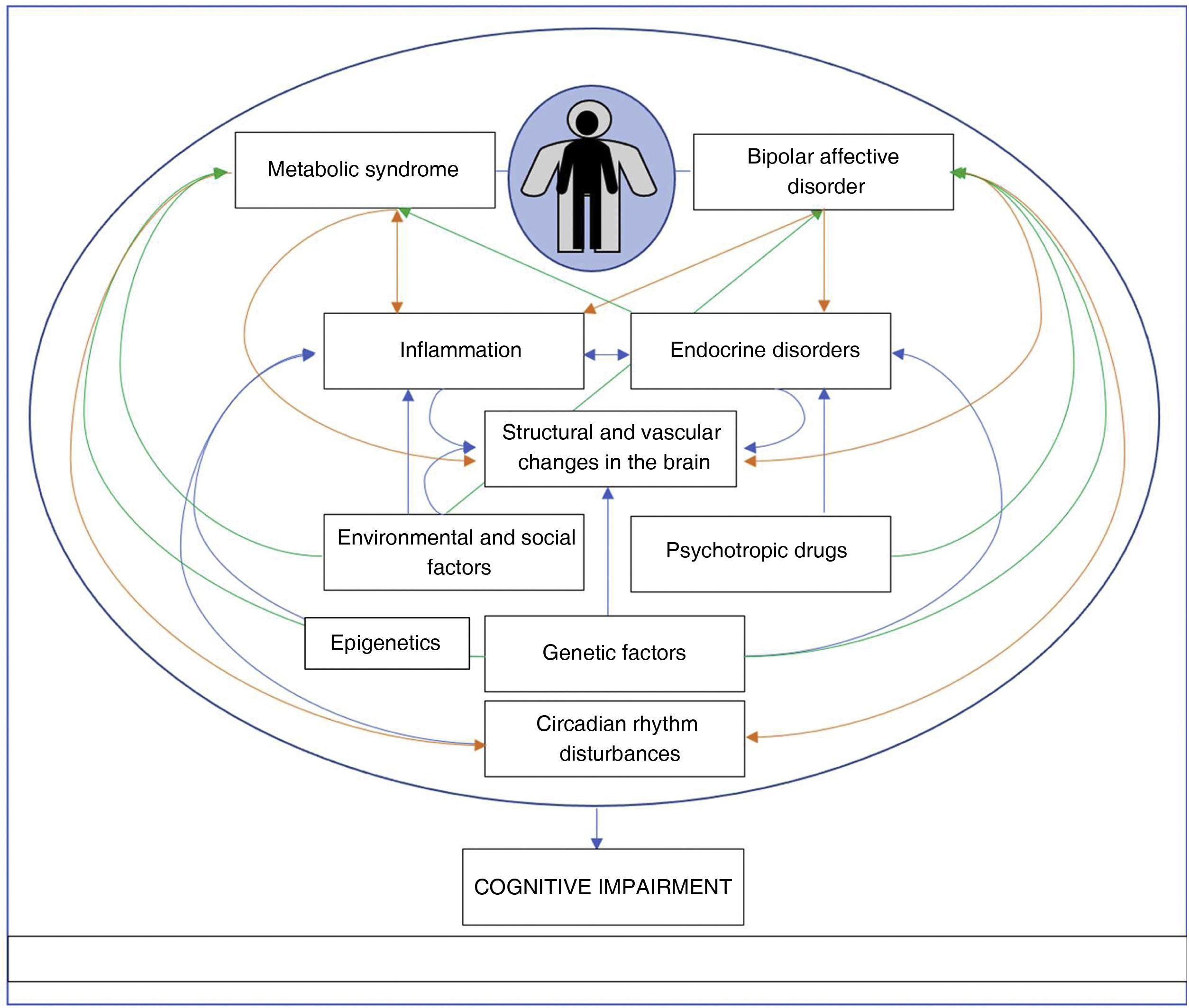
DiscussionBoth BD and MS have been associated with cognitive deficits. Thus, in this review, we present the findings related to possible pathophysiological explanations for the relationship between BD and MS and its effect on the cognitive performance of patients with BD, divided into a group of four hypotheses: endocrine; inflammatory; drug-related; and environmental and social. Using the neuroendocrine and inflammatory hypotheses, we found that hyperactivity of the hypothalamic–pituitary–adrenal axis, cortisol deregulation, and the overproduction of proinflammatory cytokines present in patients with BD are associated not only with the development of MS, but also with cognitive deficit. The drug hypothesis describes how the effect of psychotropic drugs on metabolism can have a negative impact on cognitive functions. Finally, from an environmental and social perspective, it would seem that early adverse environments, trauma, stress and unhealthy lifestyles contribute to the development of MS and, in turn, to a lower cognitive performance.
Other possible hypotheses to be considered—that are not mentioned in the literature on the subject—are sleep disorders and genetics. Circadian rhythm disturbances are thought to be of great importance in BD, even serving as an early marker of crises, and sleep loss is also prevalent in obesity, diabetes and MS.15 One of the many factors that directly influence cognitive performance is sleep, which is essential for memory consolidation and processing.79 However, it is not clear whether the changes in the circadian cycle of a person with BD and MS lead to a greater cognitive deficit purely because of the sleep disorder, or because of the cumulative factor of their comorbidities. Equally, given the evident polygenicity—and its interaction with environmental factors—involved in all three conditions (BD, MS and cognitive deficit), including genes that encode ion channels, neurotransmitter transporters and synaptic components,80 it is difficult to establish a single genetic factor as a possible explanation for the pathophysiological relationship between the cognitive deficit in BD and MS.
When we analyse these hypotheses together, they all point to the development of a series of macrocellular and microcellular changes, which in turn correlate in patients with BD and MS with a negative effect on the patients’ cognition, both generally and in specific domains, which are mainly executive function, memory, attention and perceptual motor skills. It could then be argued that there is a possible additive and synergistic factor between them, and that the “inflammation” hypothesis may play an intermediate role, by enhancing the independent effects of each one. For example, inflammation is one of the responses generated by the alteration of cortisol and the hypothalamic–pituitary–adrenal axis, which are part of the endocrine hypothesis, and one of the mechanisms mediating the structural and vascular changes also triggered by genetic and environmental factors and epigenetics (Fig. 2). Therefore, based on our review, we would venture to say that the inflammatory hypothesis and the associated dynamic changes constitute one of the strongest hypotheses, despite the contradictory findings in the studies around this.
Although information has been obtained from different sources indicating that the coexistence of BD and MS affects the cognitive function of these patients, this review has found the predominance of cross-sectional studies, with small sample sizes and multiple ways of assessing cognitive functions—which increases the heterogeneity of the results—to be a limitation. Therefore, new and continuous—and preferably longitudinal—processes of investigation are needed in order to identify and explain the common mechanisms between BD, MS and cognitive deficit. We also need to establish which factors can be modified, as an early identification and appropriate intervention could positively influence both the disease course and the progression of the cognitive deficit. This should become a challenge for those healthcare professionals who interact with this patient population on a daily basis, in addition to reducing the number of crises, increasing symptom-free time, and ensuring adequate adherence to treatment and maintaining an adequate metabolic profile.
ConclusionsThe coexistence of BD and MS in the same patients seems to have been associated with a number of different cognitive dysfunctions, which is why there has been an increased interest in recent years in understanding the pathophysiological mechanisms by which that coexistence of both diseases affects cognitive performance.
All the components of MS have been associated with a negative effect on patients’ cognition, both generally and in specific domains, these being mainly executive function, memory, attention and perceptual motor skills.
The various pathophysiological hypotheses proposed (inflammatory, endocrine, drug-related, environmental and social) suggest that a series of macrocellular and microcellular changes correlate with the deterioration of different cognitive domains in patients with BD and MS.
Further research is required in order to identify the shared biological and pathophysiological mechanisms that support the relationship between BD, MS and cognition, in order to help establish new treatment options aimed at preventing cognitive deficit.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingMinisterio de Ciencia, Tecnología e Innovación [Ministry of Science, Technology and Innovation], Colombia (code 111577757629. Contract 781 of 2017).