Functional neurological disorders, formerly referred to as conversion disorders, are a frequent clinical problem in neurology, psychiatry and primary care departments. In the new diagnostic categories, emphasis is placed on the positive characteristics necessary to diagnose this disorder. A narrative review of the scientific medical literature related to the subject was performed in order to determine the differences and advantages that the new classification of functional neurological disorders gives to doctors and patients. Historical, diagnostic, clinical and treatment concepts related to functional neurological disorders are reviewed. The conceptual differences between conversion disorders and functional neurological disorders and the implications of these changes in the clinical approach are identified. The new proposed diagnosis for functional neurological disorders provides the opportunity to transform a diagnosis made by ruling out other pathologies to a diagnosis where the presence of neurological signs suggestive of the disorder are verified and can be taught to the patient, and based on them, treatment strategies posed.
Los trastornos neurológicos funcionales, antes llamados trastornos conversivos, son un problema clínico frecuente en los servicios de neurología y psiquiatría y en atención primaria. En las nuevas categorías diagnósticas se hace énfasis en las características positivas necesarias para el diagnóstico de este trastorno. Se realizó una revisión narrativa de la literatura médica para determinar las diferencias y las ventajas clínicas que la actual clasificación aporta al diagnóstico y el tratamiento de los trastornos neurológicos funcionales. Se identifican las diferencias conceptuales entre los trastornos conversivos y los trastornos neurológicos funcionales y las implicaciones de estos cambios en el abordaje clínico. La nueva propuesta diagnóstica para los trastornos neurológicos funcionales brinda la oportunidad de transformar un diagnóstico realizado a partir del descarte de otras afecciones en otro en el que se verifica la presencia de signos neurológicos que apuntan al trastorno y se pueden enseñar al paciente, y a partir de ellos, plantear estrategias de tratamiento.
Somatic symptoms are one of the main reasons for which people go to the doctor. Up to 80% of the general population reports between one and five somatic symptoms in the last seven days.1 Functional neurological disorders (previously called conversion disorders) can justify 14% of new consolations in neurology and are the second cause of referral to this speciality, after headache.2
The incidence of functional neurological disorders has been estimated to be between 2.5 and 500/100,000 in the general population and 20 and 120/100,000 in hospitalised patients.3 Its prevalence in life is approximately 0.5%; peaks of presentation occur between the ages of 20 and 40.4 In primary care, a prevalence of 20–25% can be found, and it is more common in non-industrialised countries with low socioeconomic levels.5,6
From the first version of the Diagnostic and Statistical Manual (DSM-I) to the fourth version (DSM-IV), sensorimotor symptoms which fall into the denomination “medically unexplained” were classified first as hysterical neurosis and then as conversion disorders. It was assumed in these diagnostic manuals that sensorimotor manifestations were associated with conflicts, stressors or psychological factors, although the empirical evidence of this association was confusing and uncertain in some cases.7
An important debate was raised on how somatoform disorders could be reclassified in the DSM-5. Some believed that the category should be abolished completely,8 while others proposed to “refine it”.9 Finally, with the DSM-5, the need for a psychological stressor as an explanation of functional neurological disorder was eliminated, and it was sought to emphasise the identification of the positive characteristics in the physical examination.10 Another change of the DSM-5 is that it does not require the symptoms to be “medically unexplained” in order to consider them of a functional type; this modification that some celebrate is criticised by others who consider that this could mean that some patients are classified as “mentally ill” when they are not.11 The objective of this article was to review the practical implications for patients and doctors with regard to the diagnostic category of functional neurological disorders, emphasising movement disorders.
Literature reviewFunctional neurological disorders are symptoms and syndromes such as psychogenic movement disorders or non-epileptic seizures (NES), which are real medical problems not related to a disease process. The term functional12 is not used as a synonym of psychogenic, but instead it is used to describe a group of disorders in which a functional and non-structural alteration of the nervous system and biopsychosocial model is fundamental to understand the nature of the symptom or of the syndrome.13 Currently, around 30% of patients who attend neurological clinics do so for medically unexplained symptoms.14 A study conducted by Stone et al.,2 which included 3781 patients referred to a neurology consultation, found that 14% were diagnosed with a functional neurological disorder, and the next most common diagnosis was headache. In epilepsy video-monitoring units, 20–50% of admitted patients have non-epileptic seizures, and in abnormal movement clinics, 20% have functional movement disorders.15,16 After studying these two patient groups, some investigators found that the similarities are significant, although patients with movement disorders tend to be older, with a lower proportion of women and of previous sexual abuse than patients with non-epileptic seizures. This therefore raises the question of whether it is the same with different symptomatic expressions.17,18
The focus on medically unexplained symptoms (MUPS), although widely criticised, has made a “practical” approach possible, according to some authors. This term refers to physical symptoms which remain without a organic explanation, either due to lack of findings in the physical examination or in the paraclinical or imaging tests.3 This term has been used in three ways: (a) to refer to symptoms in the absence of obvious illness; (b) to describe specific clinical syndromes such as chronic fatigue syndrome or irritable bowel syndrome, and (c) to refer to somatoform disorders in general.
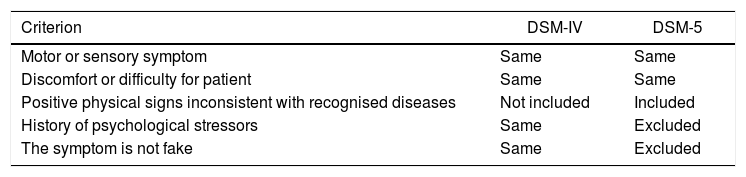
In a recent study, van Dessel et al.19 evaluated 325 patients with a diagnosis of MUPS to whom the criteria of the DSM-IV and the DSM-5 were applied; they found that 92.9% fulfilled criteria of the DSM-IV for somatoform disorders, while 45.5% fulfilled criteria of the DSM-5 for functional somatic syndrome, which indicates that the DSM-5 has more restrictive criteria and that patients have to present more intense symptoms and with greater functional impairment in order to be diagnosed according to the more recent criteria (Table 1).
Comparison between the criteria of the DSM-IV and the DSM-5 for the diagnosis of functional neurological disorder.
| Criterion | DSM-IV | DSM-5 |
|---|---|---|
| Motor or sensory symptom | Same | Same |
| Discomfort or difficulty for patient | Same | Same |
| Positive physical signs inconsistent with recognised diseases | Not included | Included |
| History of psychological stressors | Same | Excluded |
| The symptom is not fake | Same | Excluded |
DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DSM-5: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Therefore, the introduction of a new term by itself does not resolve the problem, given that it can also be misinterpreted. Success will depend on the people who are diagnosed and the clinics and investigators who use the diagnostic classification. However, it remains problematic that the diagnostic category lies in a psychiatric classification, although the symptoms exist in the interface of neurology and psychiatry. In Table 1, some diagnostic criteria of the DSM-IV and the DSM-5 for functional neurological disorder are compared.
Diagnosis of functional neurological symptoms, an opportunity to link neurology and psychiatrySince the DSM-5 played down the psychosocial formulation in the diagnosis of functional neurological symptoms, others doctors who are not psychiatrists have seen the opportunity to approach these diagnoses. This can be seen as a disadvantage or as an opportunity. From the first impression, the psychiatrist would see the need to retake from neurology the elements of the physical examination which would contribute positively to the diagnosis. From the second position, the psychiatrist would be left out of this diagnostic category, as the study by Kanaan et al.20 indicates, in which neurologists and neuropsychiatrists in the United Kingdom were interviewed, in order to understand the opinion that they had of the role of psychiatry in the diagnosis of functional neurological symptoms. A total of 76% responded that psychiatrists are not essential for the diagnosis of conversion disorders, and 71% that psychiatrists do not consider the diagnosis of conversion disorder, even when the case is referred to them.20
However, and although the diagnostic approximation proposed by the DSM-5 requires that the psychiatrist has more training in the neurological physical examination which makes it possible to look for positive neurological signs from the current diagnosis, with regard to psychological criteria and the discrimination of the functional symptoms that these allow, there is no doubt that in some cases they will be absolutely relevant for the diagnosis, as stated by Kanaan et al.: “Nobody who has had a patient who developed dysphonia before going on stage or dystonia of the hand after signing an unwelcome document would doubt that there is a psychological history that makes sense of their problem”.21
Neurosciences and functional neurological disordersThe different presentations of functional neurological disorders, such as motor, sensory and visual abnormalities and NES have been studied using different perspectives: psychoanalytic, neurophysiological, cognitive and through structural and functional images, among others. The functional motor presentations included in this review can be subdivided into negative symptoms, such as weakness or paralysis, and positive symptoms, such as tremor, dystonia or NES.22
Until now, no definitive model has been proposed of the neuronal correlations in functional neurological disorders.23 Pérez et al. observed that neuroimaging studies of these patients indicate alterations in four cerebral regions which mediate processing and emotion regulation (pregenual anterior cingulate cortex, ventromedial prefrontal cortex, insula and tonsils), cognitive control (dorsolateral prefrontal cortex, dorsal anterior cingulate cortex, inferior frontal gyrus), self-referential processing (temporoparietal junction, posterior cingulate cortex and precuneus) and motor planning (supplementary motor area).24 In addition, three key concepts have been proposed25:
- •
Attention or self-monitoring. Attention has been proposed as an important factor for the development and maintenance of MUPS.19 In the case of functional neurological disorders, self-directed attention is necessary for the symptom to manifest. This is why a reduction or disappearance of functional movement tends to be observed when using distraction techniques.26 For example, a certain sensitivity to distraction has been demonstrated in patients who suffer functional tremors with tests which include rhythmic voluntary movements,27 ballistic movements,28 auditory rhythms29 and mental concentration in numerical series of sevens.30
- •
Expectations/beliefs related to the symptom. This concept not only covers the consciously reported beliefs of the symptoms, but also includes the previous expectations or beliefs towards these in the context of active inferences carried out by the brain. Active inferences refer to those that the brain can predict actively and look for explanations for the sensory afferent neurons based on past experiences.31 Therefore, interactions between sensory bottom-up information and top-down predictions on information received result in perception or movement. Therefore, patients with functional neurological disorders can present symptoms which are not consistent with the neuroanatomical and neurophysiological principles of the disease, but that are adapted to beliefs acquired previously about brain function.22
- •
Agency. The sense of agency refers to a fundamental aspect of the own conscience of human beings. With this, judgements can be made about our actions (“I have moved my arm” versus “my arm was moved”) and having a sense of control of these: a sense of agency.32 Abnormal movements in functional neurological disorders resemble the movements made deliberately by the patient. However, the patients’ report is that they do not control this movement, which is why it has been considered that there could have been an interruption of processes related to the sense of agency in these patients.22 Furthermore, Pareés et al.33 demonstrated that these patients may have differences in sensory attenuation compared to control patients. Sensory attenuation refers to the physiological phenomenon that causes a reduction in the perception of the intensity of self-generated stimuli.34 Furthermore, it is believed that sensory attenuation reflects the process that labels the movement as self-generated and has been related to the loss of sense of agency and contributes to the perception of the movement as involuntary.35
Recently, Espay et al.36 have proposed the need to establish specific diagnostic criteria based on phenotypes. Their main argument lies in the fact that relevant clinical signs depend on the specific phenotype. For example, distractibility is a key characteristic of functional tremor, but it would not be applied to functional dystonia, which, according to them, is better defined by the fixed nature of the symptom.
The proposal of the DSM-5 to reach the diagnosis of functional neurological disorders from the positive signs found in the neurological examination triggered the interest of clinicians and investigators.37 Daum et al.38 compared the presence of 38 clinical signs in 20 patients with “conversion disorder” and 20 control patients with an organic lesion. They identified five highly reliable signs: (a) Hoover's sign; (b) giveway weakness; (c) co-contraction; (d) midline splitting and (e) splitting of vibration sense. The last two were in the case of sensory deficit.
The diagnosis of functional tics can be particularly difficult because distractibility and suggestibility are also characteristics of body tics.39,40 However, onset in adulthood following a precipitating event, absence of family history, inability to suppress movements, absence of premonitory emergency, absence of pali-, echo- and coprophenomena, the presence of blocking tics, lack of rostral-caudal distribution of the tics and the presence of other functional neurological symptoms indicate the presence of functional tics.
Therefore, to determine that a symptom is functional neurological, the following conditions should be met: (a) that it causes discomfort or difficulty in the patient's functioning; (b) that it is not consistent with another recognised disease, and (c) that it is not explained as a simulated symptom.
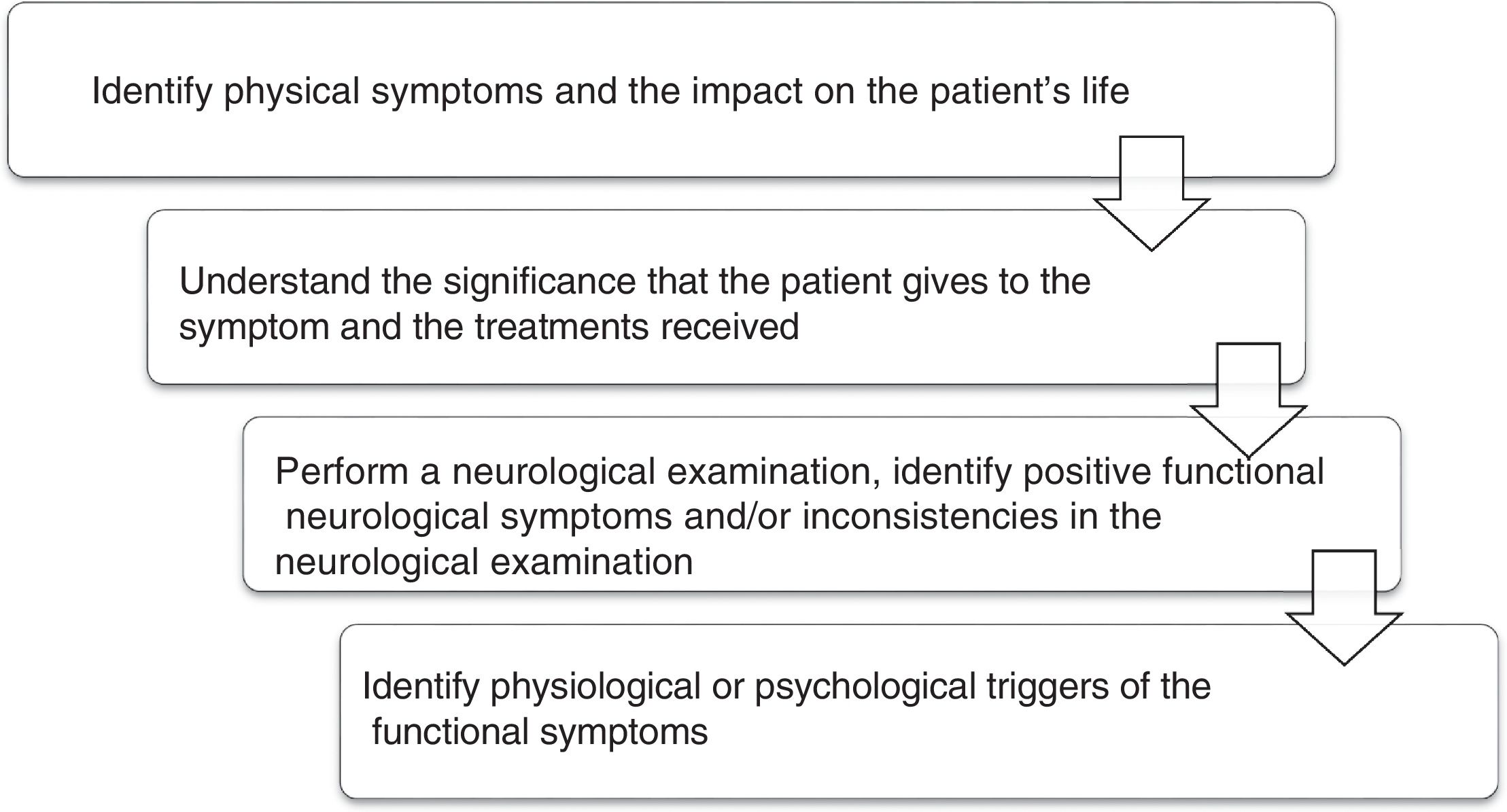
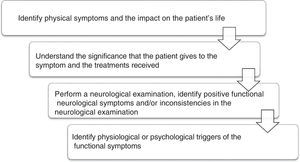
Several professionals may assess these patients: general practitioners, psychologists, neurologists, psychiatrists and other medical specialists. To facilitate the approach, the sequence in Fig. 1 is proposed.18
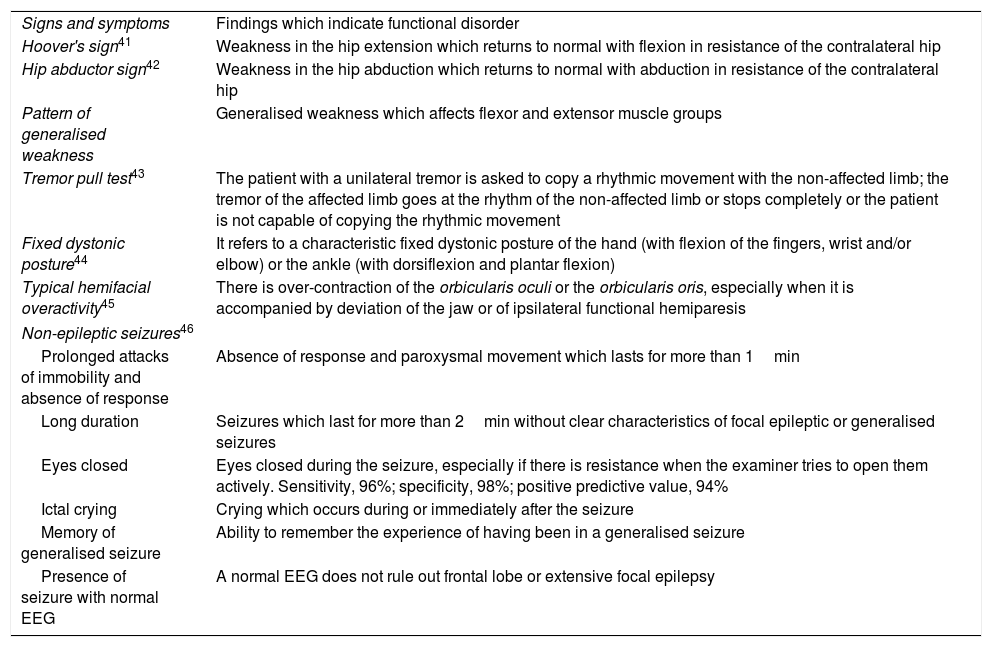
Physical examinationThe positive findings of the physical examination of a patient with functional neurological symptoms are the key to the diagnosis. Therefore, the diagnosis is not done by exclusion or only because the symptoms are peculiar. Some examples of clinical signs which are a strong indication of functional neurological symptoms are described in Table 2.
Motor symptoms which can be found in patients with functional neurological disorder.
| Signs and symptoms | Findings which indicate functional disorder |
| Hoover's sign41 | Weakness in the hip extension which returns to normal with flexion in resistance of the contralateral hip |
| Hip abductor sign42 | Weakness in the hip abduction which returns to normal with abduction in resistance of the contralateral hip |
| Pattern of generalised weakness | Generalised weakness which affects flexor and extensor muscle groups |
| Tremor pull test43 | The patient with a unilateral tremor is asked to copy a rhythmic movement with the non-affected limb; the tremor of the affected limb goes at the rhythm of the non-affected limb or stops completely or the patient is not capable of copying the rhythmic movement |
| Fixed dystonic posture44 | It refers to a characteristic fixed dystonic posture of the hand (with flexion of the fingers, wrist and/or elbow) or the ankle (with dorsiflexion and plantar flexion) |
| Typical hemifacial overactivity45 | There is over-contraction of the orbicularis oculi or the orbicularis oris, especially when it is accompanied by deviation of the jaw or of ipsilateral functional hemiparesis |
| Non-epileptic seizures46 | |
| Prolonged attacks of immobility and absence of response | Absence of response and paroxysmal movement which lasts for more than 1min |
| Long duration | Seizures which last for more than 2min without clear characteristics of focal epileptic or generalised seizures |
| Eyes closed | Eyes closed during the seizure, especially if there is resistance when the examiner tries to open them actively. Sensitivity, 96%; specificity, 98%; positive predictive value, 94% |
| Ictal crying | Crying which occurs during or immediately after the seizure |
| Memory of generalised seizure | Ability to remember the experience of having been in a generalised seizure |
| Presence of seizure with normal EEG | A normal EEG does not rule out frontal lobe or extensive focal epilepsy |
EEG: electroencephalogram.
Adapted from Stone et al.23
One of the most traditional signs of functional neurological disorders is la belle indifférence. In a systematic review carried out by Stone, it was found that the mean frequency of this sign was present in 21% (0–54%) of 356 patients with conversion symptoms and in 29% (0–60%) of 157 patients with organic disease. Current evidence does not support the use of la belle indifférence in order to discriminate between conversion symptoms and symptoms of organic diseases,47 although in some cases it could have an important diagnostic value.
Aspects of the clinical evaluation which are not necessary or can be delayedDue to the influence and emphasis of previous versions of the DSM, some clinicians feel the need to find a recent psychological stressor or a history of traumatic events that can be associated with the functional neurological disorder. This investigation is not currently necessary for the diagnosis of functional neurological disorder. One of the reasons for this statement according to some authors is that the time of the first consultation is short and skill and training is required to address these aspects correctly. The active search for symptoms of anxiety or depression during the first evaluation by the neurologist or the non-psychiatrist doctor is not a priority either. These aspects can be evaluated at a later stage.22
The objectives of the psychiatrist and psychologist include identifying comorbidities such as depression, anxiety, dissociation, use of substances or abuse, for which the specific treatments that each case requires will be indicated, such as psychotropic drugs and/or psychotherapy. It is not necessary or sufficient to find a psychiatric comorbidity to confirm or rule out a functional neurological symptom. The possibility that functional symptoms co-exist with other symptoms of established neurological disease should also be considered.42
In terms of diagnostic error, a systematic review which included 27 studies with 1466 patients, from 1965 to 2003 and with an average follow-up of five years, demonstrated that diagnostic errors or false positives are decreasing: in 1950, 29% (interval 23–36%); in 1960, 17% (12–24%); in 1970, 4% (2–6%), and in 1980, 4% (2–6%). This difference is statistically significant (p<0.02), independently of age, gender and duration of symptoms.48
Therapeutic focusOnce the diagnosis is clear, its nature should be communicated appropriately to the patient. In order to achieve this, it is necessary to take into account the most common errors: (a) telling the patient that they do not have anything; (b) telling them that what is happening is not a neurological problem; (c) attributing the functional symptoms to psychological problems prematurely; (d) focusing excessively on the absence of pathological findings in the neurological examination.
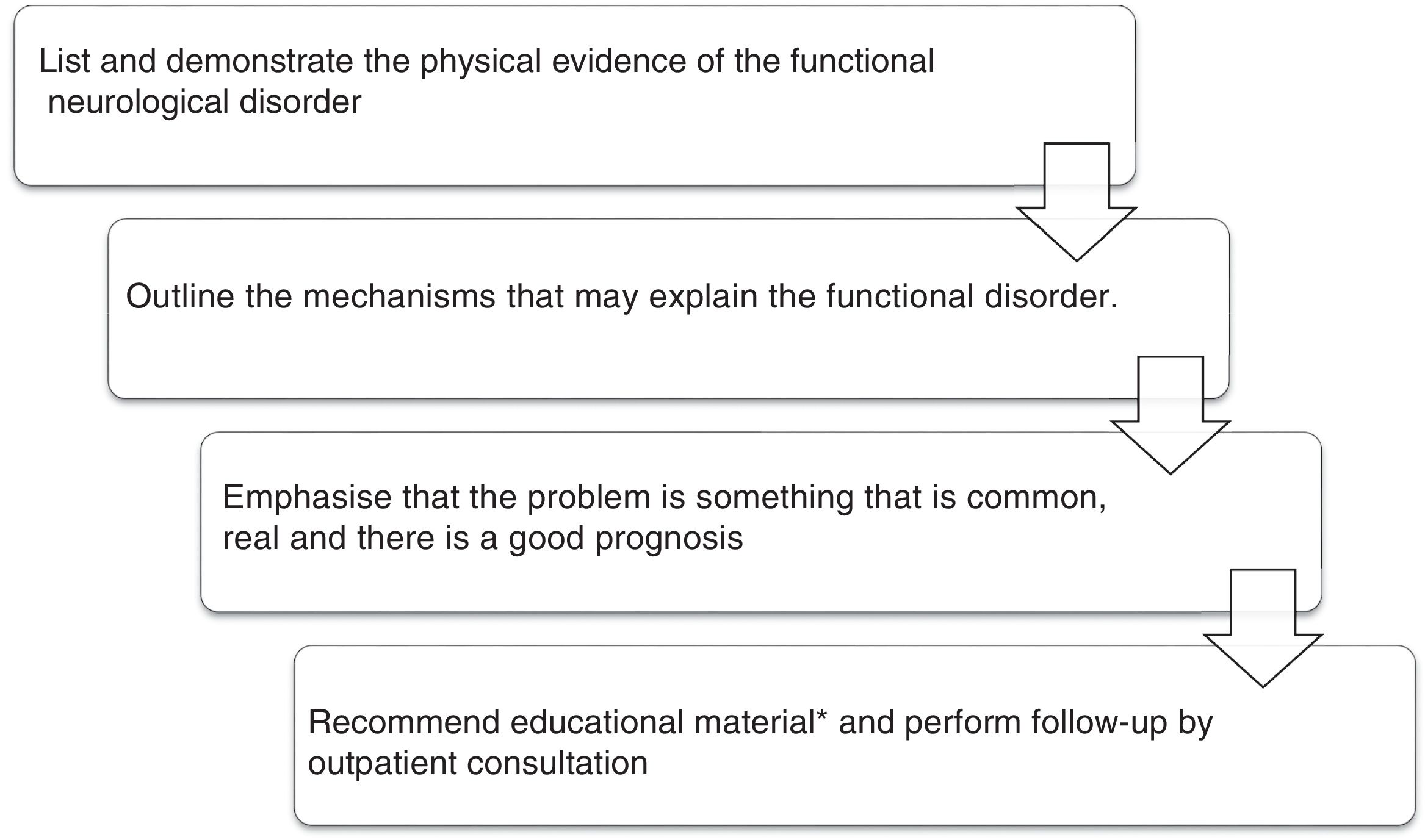
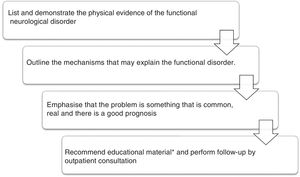
The importance of neurologists in the teams who evaluate these patients is increasingly insisted upon.49 Consistent with this, once the diagnosis has been performed, the process of educating the patient and their family should be started, highlighting the common, genuine, functional and potentially reversible nature of the symptoms. The positive nature of the diagnosis should be explained, including the demonstration of relevant signs in the neurological examination and the important role of care, expectations and predictions in these types of movements. Patients should be shown simple distraction strategies (music, walking, alternating gait patterns) to interfere in the case of abnormal movements.50 All patients should be followed-up on an outpatient basis to provide them with support in the recovery and to determine the need for complementary studies. Fig. 2 describes the comprehensive care and psychoeducational material which has been used in specialist treatment centres.
Care of patient with diagnosis of functional movement disorder.
*Educational material.51
A group of experts in functional movement disorders gathered in Edinburgh in 2013 with a view to proposing therapeutic recommendations based on physiotherapy.52 Based on the symptom generation model, this type of physiotherapy seeks to approach and impact on the beliefs of disease, self-directed attention and abnormal movement patterns of the patients through a process of education, retraining of movements and strategies of self-management within a positive non-judgemental context. In this way, this type of physiotherapy is currently a key point in the multidisciplinary care of patients with functional movement disorders.
Cognitive behavioural therapy (CBT)In the last decade, CBT has been studied in the treatment of NES, with positive results. Goldstein et al.53 compared 12 weeks of CBT+standard medical care versus standard medical care without CBT in 66 patients with NES. The intention-to-treat analysis showed a statistically significant reduction in the frequency of seizures at the end of the treatment; however, this difference was not maintained in the follow-up at three months. More recently, La France et al.,54 in a randomised multicentre clinical trial, compared four treatment arms in 38 patients with NES: flexible dose of sertraline, CBT, CBT+flexible dose of sertraline and standard medical care. Both psychotherapeutic treatment arms demonstrated a significant reduction in seizures. In the CBT group there was also significant improvement in the depression, anxiety, quality of life and general functioning scores. Currently, this psychotherapeutic intervention is being publicised as a therapeutic option for the treatment of NES.55
Repetitive transcranial magnetic stimulationRepetitive transcranial magnetic stimulation (rTMS) has been proposed as a tool for the treatment of functional neurological disorders. Shah et al.50 reported the positive effects of the application of rTMS in the motor cortex and dominant premotor cortex, combined with suggestion techniques. After the stimulation of the premotor cortex, they observed improvement in quality of life in relation to the physical symptoms, but worsening of the psychological symptoms was reported.
In another study, Broersma et al.56 evaluated the efficacy of rTMS in patients with functional hand paresis. The use of rTMS in the motor area related to the hand induced a significant increase of muscular strength measured objectively. However, the subjective rates of improvement did not differ with respect to the placebo group. These results indicate that rTMS could improve the muscular strength of patients with functional paresis by itself, but at the same time they indicate that the reduction in muscular strength is not a nuclear issue of these patients, which is why rTMS could be used in conjunction with behavioural approaches.
Hypnotic suggestionHypnosis involves the controlled modulation of some components of cognition by an external agent (hypnotist) or oneself (self-hypnosis) using suggestion, which usually takes the form of verbal orders related to the intended effect. A hypnosis session starts with an induction procedure, using suggestions to focus attention and relaxation, followed by targeted suggestions with the aim of producing changes in some aspects of the experience or behaviour. Therefore, the effects of suggestion include the production or removal of what is attributed as functional symptoms.57
The use of suggestion in hypnosis for the treatment of functional symptoms has increased in recent decades. Nevertheless, the evidence base on this topic is dominated particularly by case reports and case series. To date, only two controlled and randomised studies which included the use of hypnosis for hospitalised patients and outpatients with functional neurological symptoms have been performed.58,59 Only one of these studies showed an additional benefit with the use of hypnosis. More studies on this subject are needed.57
To conclude, functional neurological disorders are made up of a range of diverse symptoms which are disabling for patients and highly prevalent in general and specialised medical consultations. The diagnosis, before exclusion, should now be performed from the positive findings of the neurological examination, backed up with the clinical suspicion derived from the patient's history.
Clinicians who treat patients with suspected functional neurological disorders now have the opportunity to adopt new diagnostic and therapeutic strategies which test the clinical ability to explain the diagnosis and educate the patient and their family in the face of these clinical manifestations, which will have a crucial importance in the progression and prognosis of the patients.
With the current interest for this clinical condition and the contribution from research and neurosciences, it is possible to think that in the near future the understanding of the neurogenesis of these disorders will improve and patients will be offered better therapeutic approaches.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Restrepo M, Restrepo D. Del trastorno conversivo a los trastornos neurológicos funcionales. ¿Superando el diagnóstico por descarte? Rev Colomb Psiquiat. 2019;48:174–181.