Schizophrenia is a severe and persistent mental disorder that affects around 21 million people worldwide. The etiology of schizophrenia is currently understood as heterogeneous and multifactorial. Genetic and environmental factors are the most common explanations for the onset of schizophrenia, but along with these, hybridized cultural ideas coexist between medical, superstitious, and religious paradigms. The objective was to identify the relationship between cultural beliefs about schizophrenia, etiology and expressed emotion.
MethodsThe present study used a mixed-method design, with an analytical approach for ethnographic research. The sample consisted of 40 people, relatives of patients diagnosed with schizophrenia, selected using simple random probabilistic sampling.
ResultsA valid cultural consensus was found with statistical significance (p≤.05). Emotional trauma in childhood was identified as the leading cause of schizophrenia, followed by hereditary factors, emotional problems, head trauma, mistreatment, and divine will. The better-informed relatives expressed less emotion than those with less cultural competence (Mann-Whitney's U=1.000; p<.001).
ConclusionsMexican families in this study had a high degree of scientific knowledge about the etiology of schizophrenia, but religious ideas and compassionate explanations were part of this hybridized model.
La esquizofrenia es un trastorno mental que afecta a 21 millones de personas en todo el mundo. La etiología de esta enfermedad es multifactorial. Los factores genéticos y ambientales son las explicaciones más comunes sobre su etiología, pero otros paradigmas supersticiosos y religiosos han formado un modelo híbrido que la definen. El ojetivo es identificar la relación entre las creencias culturales de la etiología de la esquizofrenia y la emoción expresada.
MétodosEl presente estudio utilizó un método mixto con un diseño analítico para investigaciones etnográficas. La muestra estuvo conformada por 40 personas, familiares de pacientes diagnosticados de esquizofrenia, seleccionadas mediante muestreo probabilístico aleatorio simple.
ResultadosSe halló un consenso cultural válido estadísticamente significativo (p ≤ 0,05). El trauma emocional en la infancia fue la más importante creencia cultural que causa la aparición de la esquizofrenia, seguida de problemas emocionales, lesiones en la cabeza, maltrato y voluntad divina. Los familiares con mejores conocimientos sobre las causas de la esquizofrenia mostraron menores índices de emoción expresada (U de Mann-Whitney=1,000; p<0,001).
ConclusionesLas familias mexicanas poseen una gran adherencia al conocimiento científico sobre las causas de la esquizofrenia, pero las ideas religiosas y compasivas coexisten con el conocimiento sobre la enfermedad.
Schizophrenia is a severe mental disorder with a worldwide prevalence from 1.4 to 4.6,1 and incidence rates from 0.16 to 0.42 per 1000 population.2 The etiology of schizophrenia is currently understood as multifactorial. However, schizophrenia has been considered mainly as a brain disorder. Biological explanations about the causes of schizophrenia are highly developed on science fields, in areas like the expression of genes, brain function, genetic predisposition, abnormalities in brain development and maturation, neural circuits or neurotransmitter systems.3 However, other non-genetic factors have been studied in relation with the appearance of schizophrenia. Environmental variables as problematic family interactions, unstable parenting, psychosocial stressors, isolation in childhood, immigration, being part of an ethnic minority, chronic cannabis use during adolescence, obstetric complications, severe malnutrition in gestation, fetal hypoxia, incompatibility of Rh blood factor, or being born during the winter or early spring, are variables that demonstrated to increase the risk of developing schizophrenia.3
Though, more importance has been given to the biological aspects than to the psychosocial variables.4 This is allegedly due to the need of increasing the social acceptance of people with the diagnosis who are typically stigmatized; therefore, schizophrenia has been presented as a medical disease like any other.5
Nevertheless, the adoption of the biogenetic model for the explanation of causes of schizophrenia has not been improving the understanding of this illness, and prejudices as well as social exclusion towards these people have remained.6 Despite the most common information that specialists spread to families through health promotion and other psychosocial programs, stigmatic paradigms remain and coexist with scientific knowledge at the same level, building with this hybridized cultural ideas which fluctuate between medical comprehension about causes of schizophrenia and other beliefs.6
Stigma in schizophrenia is one of the difficulties that most affects the understanding of this condition. Stigma is defined as the set of beliefs and attitudes of negative connotation that a group has towards minority groups with some differential attribute, which incite a negative stereotype towards these people in social conscience. One of the most common stigmatic distortions that enlighten the development of schizophrenia is related to the magical-religious explanations of the disease, among others.7
The acceptance or rejection of patients with a severe mental disorder will depend on values and beliefs of the communities where they live. Cultural beliefs about causes of schizophrenia provide different meanings of the disease, and not only explain the disorder in a different way, but also create more tolerable coping strategies for relatives.7 Nonetheless, the lack of scientific knowledge about schizophrenia, usually generates stigmatic attitudes and social rejection towards people who suffer from it,8 and can even affect the family members who take care of the patient, predisposing them to have unhealthy attitudes of criticism, mistreatment, and over-involvement.
In a study conducted in Europe by Ruiz et al.,8 it was reported that 68% of the participants attributed the causes of schizophrenia to biological factors. This research also found the variable “childhood trauma” as a possible trigger for the disorder. Also, a study performed in Spain9 reported that people believed that this disease occurred due to excess of drugs, alcohol or parties. Another factor was the guilt associated with mistakes people made in the past and could not cope with. In 2004, a study in Italy highlighted the variable “child trauma” as one of the most important mentions to explain the etiology of schizophrenia, other variables were stress and couple breakups.10
In Guadalajara (Jalisco, Mexico) in 2003, an ethnopsychiatric study which included 41 relatives of patients with some psychiatric diagnosis from the hospital Fray Antonio Alcalde reported that 27% of participants attributed the cause of the disease to drug use, 22% referred to “nervousness”, 20% pointed to head trauma, and 12% pointed to witchcraft.11 Other studies in different latitudes have also found a high percentage of magical religious explanations about the etiology of schizophrenia. A research work carried out in Bali12 reported that 39 relatives of patients with schizophrenia, believed that causes of onset of schizophrenia were: god's will, witchcraft, brain disorders and stress.
Moreover, other 3 studies carried out on the African continent (Ethiopia, Nigeria, and Morocco) mentioned by Muñoz and et al., in 2009, show that the main causal attributions of schizophrenia were: supernatural factors, drugs, and brain biological causes.13 Nevertheless, in 2018, a study conducted in Suzhou and Siping (China) found that respondents attributed the cause of schizophrenia to social, interpersonal and psychological problems (84%) rather than to biological or brain disease problems. The most important cause reported were “stress”.14 Regardless of where the research is conducted, the meaning attributed to the etiology of the disease is often mixed with scientific information and cultural beliefs. However, the most distanced the beliefs are from scientific reality, the attitudes towards people diagnosed with this disorder tend to be less tolerant.
Stigmatic explanations regarding to this illness generate complications in primary caregivers who are normally family members, and who, in different studies have shown levels of emotional, physical and financial overload. These dynamics are commonly known as expressed emotion (EE). High EE is characterized by a series of relationships and communications in the family environment, loaded with negative assessments, criticism, control, and over-involvement; such dynamics cause poor self-concept in individuals with psychosis, as well as difficulty in treatment adherence, emotional instability, symptomatic exacerbations, and continuous relapses, according to Barrowclough et al.15
Cognitive anthropology is a scientific discipline that has provided specialized methods for understanding these issues, with tools such as Cultural consensus, which through free lists examines the knowledge of individual beliefs on any social matter.16 Also, this approach is commonly used to describe beliefs about health problems. The largest number of informants who independently agree on an answer will structure their own cultural domain. This perspective allows to recognize how people understand the processes, in this case, of mental health-illness, beliefs that predispose them to externalize certain behaviors on the individuals who suffer, in this case, schizophrenia.
Therefore, the aim of this research is to study the cultural consensus about the etiology of schizophrenia and its possible relation with high EE, in order to gain a greater understanding of how families perceive the causes of the disease and whether this comprehension impacts on family functioning and the EE, or not. The hypothesis sustains that there is a link between the cultural believes about schizophrenia etiology and high EE.
MethodsThis research used the tools of cognitive anthropology to analyze through semantic structures, the cultural consensus of relatives of individuals with schizophrenia on the etiology of schizophrenia, and its relation with the EE. This study has a mixed design with an analytical method used in ethnographic research.
ParticipantsThe sample was calculated based on Weller and Romney proposal17 to obtain a level of competence greater than 50%, with a reliability level of 95% and error of 5%. Thus, a total of 40 relatives from 18 different families of users from the Instituto Jalisciense de Salud Mental (SALME) in the Area Metropolitana de Guadalajara, were chosen using a simple random probabilistic sampling.
InstrumentsThe Family Expressed Emotion Questionnaire (CEEF) used to evaluate the EE was created by Guanilo and Seclén in 1993.18 This is a structured instrument, made up by 30 Likert-type items that assess criticism, over-protection and hostility, that was adapted for Mexican population with a Cronbach's alpha from >.8570. Its validity has been tested in Mexico by Rascón et al.,19 with the interview Five-Minute Speech Simple (FMSS), obtaining results for CRI κ=.753 and for SIE κ=.729. The cut-off points of De la Torre (2018) were taken as reference, in which a score from 30 to 64 was considered low EE and from 65 up to 120, high EE.
Beliefs about the etiology of schizophrenia were studied with the ethnographic tools of cultural consensus through the technique of free lists. The software used was Anthropac©,20 to analyze the ratio of variances and therefore, to determine the cultural consensus. Cultural agreement was considered when the variability ratio of the studied model was ≥3.20 The average of cultural knowledge was used as a correlation with values ranging from 0 to 1. Johnson's grouping was used to integrate similar items and create multidimensional scale graphs, with a stress adjustment among all items in less than 0.100.21
ProcedurePeople diagnosed with schizophrenia from SALME were identified, and the main caregivers from their families were contacted via phone call to schedule an interview in their homes. All the people identified as primary caregivers of the patients were included. Then, individually and in a private space for each family member, the aim of the study was explained to them, and an informed consent was signed. After that and based on the free list,22 open questions related to the causes of schizophrenia were asked, and once answered, the CEEF of Guanilo and Seclén was applied.18 Based on Anthropac software, the results of the significance were obtained to identify if there was a valid and statistically significant cultural model on the causes of schizophrenia. In addition, with this data, the graphic representations of how the concepts were grouped in each cultural domain were made.
Data analysisThe association between ordinal, nominal, and numerical variables was performed by parametric (Student's t, single factor ANOVA) and non-parametric tests (Fisher's χ2, Mann-Whitney's U) with a 95% reliability level, and 5% alpha error with the SPSS 20 program.
This research was conducted in accordance with the ethical principles for human research in the Helsinki Declaration, the International Harmonization Conference for Good Medical Practices, and the General Health Law on Health Research of the United Mexican States. This research has a low risk according to the General Health Law on Health Research. That being so, the signature of the primary caregivers of the patient was required on an informed consent and it was submitted to consider implementation by Unidad de Investigación Social y Epidemiológica-Instituto Mexicano del Seguro Social (UISESS-IMSS) research committee and the bioethics and research committee of the Mental Health Institute of Jalisco.
ResultsThe sample consisted of 40 relatives of individuals with schizophrenia from 18 different families in the Área Metropolitana de Guadalajara. The average age (range) of the participants was 48.53 (13-86) years; 80% were women. Their marital status predominance was marriage by 60%, 75% professed Catholicism, and 12% reported being Jehovah's witnesses; 40% had finished elementary school studies, 25% finished middle school, and 15% had a bachelor's degree; the rest had high school studies or identified themselves as illiterate.
A 27.5% were housewives, 17.5% had formal employment, and the rest were students and/or unemployed. 70% recognized their role towards their diagnosed family member as supervisors, 55% reported a good and close relationship with their relative, and 30% reported a good but distant one. All of them identified themselves as economically marginalized, part of a low socioeconomic stratum.
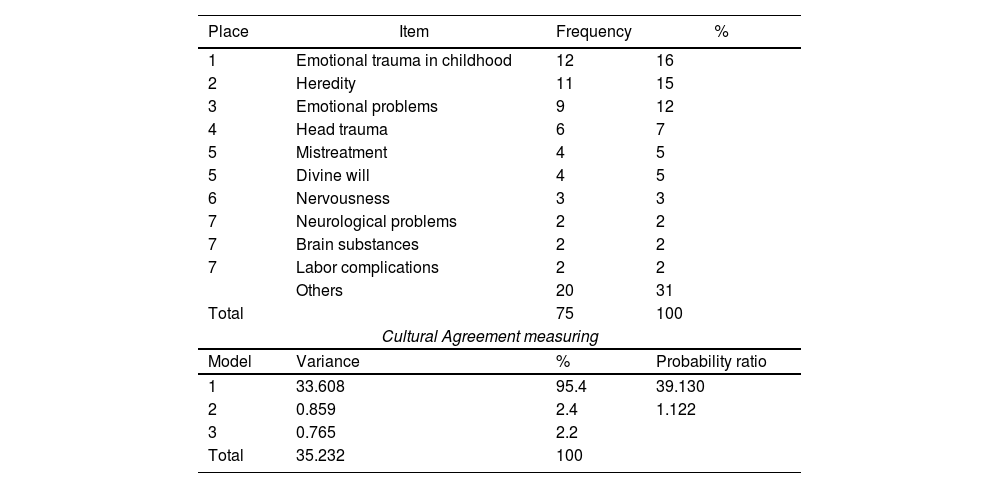
Regarding the beliefs about the factors that cause the onset of schizophrenia, it was found that emotional trauma in childhood was identified as the first cause of schizophrenia described by family members (16%). The next factor was heredity with 15% and was followed by emotional problems (12%), head trauma (7%), mistreatment (5%), and divine will (5%), among others. It should be noted that variables related to neural problems and brain substances (4%) occupied the last places on the list but were still part of the valid cultural consensus (Table 1).
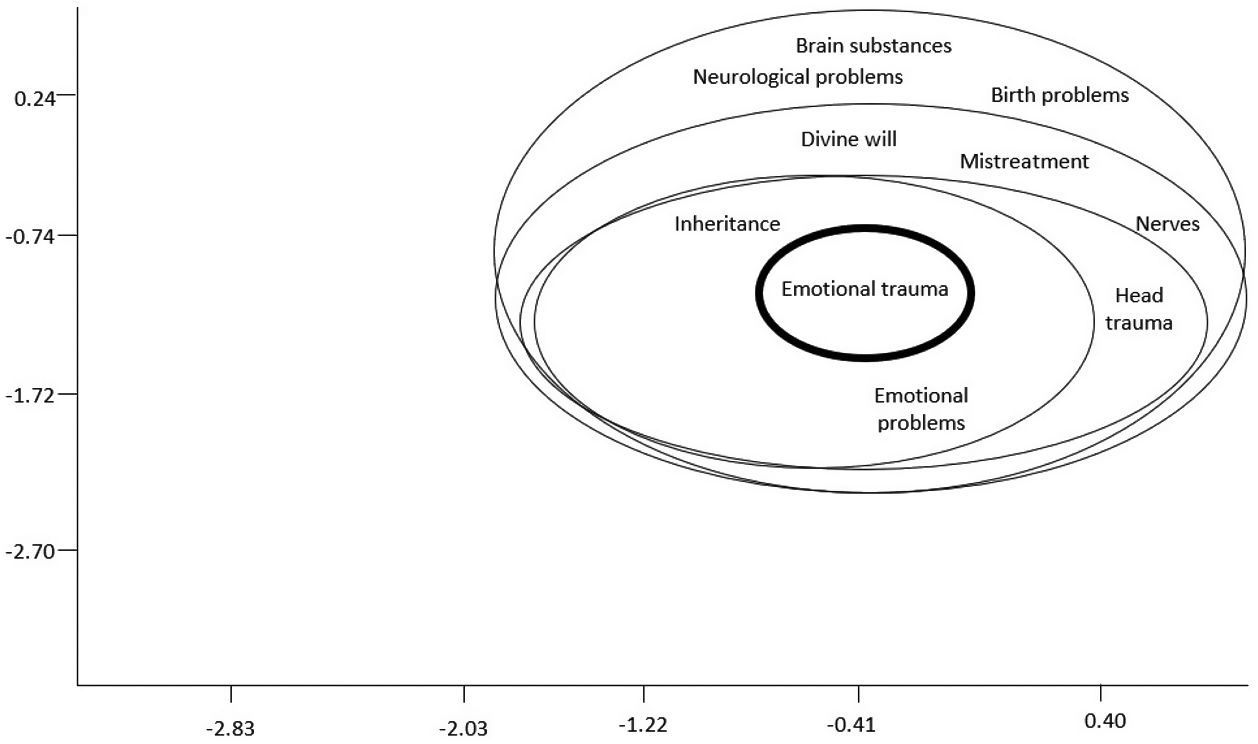
Multidimensional diagram.
| Place | Item | Frequency | % |
|---|---|---|---|
| 1 | Emotional trauma in childhood | 12 | 16 |
| 2 | Heredity | 11 | 15 |
| 3 | Emotional problems | 9 | 12 |
| 4 | Head trauma | 6 | 7 |
| 5 | Mistreatment | 4 | 5 |
| 5 | Divine will | 4 | 5 |
| 6 | Nervousness | 3 | 3 |
| 7 | Neurological problems | 2 | 2 |
| 7 | Brain substances | 2 | 2 |
| 7 | Labor complications | 2 | 2 |
| Others | 20 | 31 | |
| Total | 75 | 100 | |
| Cultural Agreement measuring | |||
| Model | Variance | % | Probability ratio |
| 1 | 33.608 | 95.4 | 39.130 |
| 2 | 0.859 | 2.4 | 1.122 |
| 3 | 0.765 | 2.2 | |
| Total | 35.232 | 100 | |
A single valid cultural consensus was found, with a variability ratio of 39,130 and a statistical significance of P≤.05, which included 95.4% of all possible variations of the model items, with a multidimensional diagram with stress of 0.01 (figure 1).
At the center of the multidimensional diagram was located the variable “emotional trauma” as the strongest idea of the cultural consensus of this sample. In the later circles, emotional problems and hereditary factors were positioned as the second most common group of variables. Mistreatment, divine will, nervousness, and head trauma were placed in the following two spheres as possibilities that completed the most solid explanations about the appearance of schizophrenia. This cultural agreement has hybridized explanations defined by: biological, religious and compassionate issues.
Therefore, it resulted that 55% of the sample in this study had a low EE and the remaining 45% had a high EE. Based on the single-factor ANOVA, there was no significant difference between gender (P=.898), marital status (P=.839), religion (P=.473), schooling (P=.382), occupation (P=.479), or family relationship (P=.170) with the expressed emotion.
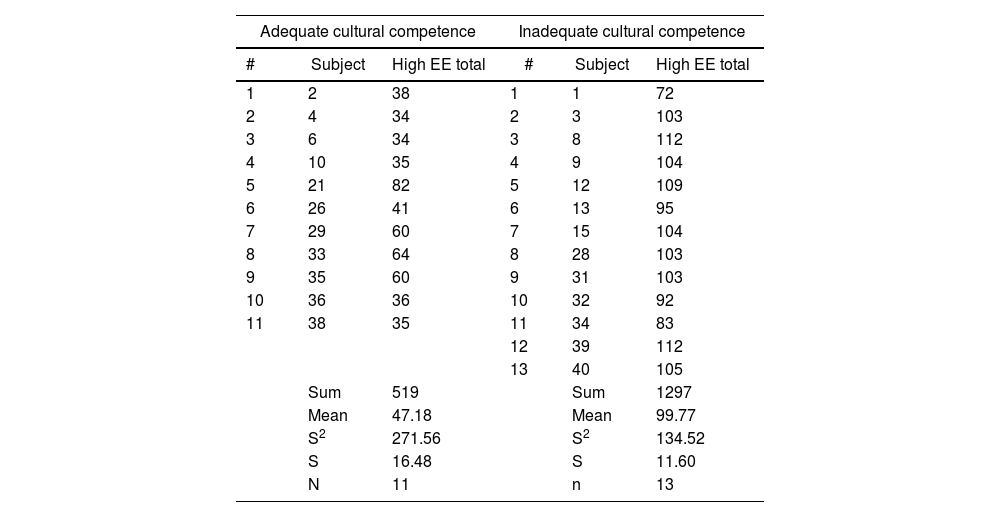
Participants with adequate cultural competence (good informants) who provided answers attached to the valid cultural consensus on etiology of schizophrenia and people with inadequate cultural competence (bad informants) were categorized in order to analyze a possible association with high EE. Subjects with inadequate cultural competence showed a high EE (P≤.05) (t=–9.15; 95%CI, 64.50-40.66) (Table 2).
Cultural competence and expressed emotion.
| Adequate cultural competence | Inadequate cultural competence | ||||
|---|---|---|---|---|---|
| # | Subject | High EE total | # | Subject | High EE total |
| 1 | 2 | 38 | 1 | 1 | 72 |
| 2 | 4 | 34 | 2 | 3 | 103 |
| 3 | 6 | 34 | 3 | 8 | 112 |
| 4 | 10 | 35 | 4 | 9 | 104 |
| 5 | 21 | 82 | 5 | 12 | 109 |
| 6 | 26 | 41 | 6 | 13 | 95 |
| 7 | 29 | 60 | 7 | 15 | 104 |
| 8 | 33 | 64 | 8 | 28 | 103 |
| 9 | 35 | 60 | 9 | 31 | 103 |
| 10 | 36 | 36 | 10 | 32 | 92 |
| 11 | 38 | 35 | 11 | 34 | 83 |
| 12 | 39 | 112 | |||
| 13 | 40 | 105 | |||
| Sum | 519 | Sum | 1297 | ||
| Mean | 47.18 | Mean | 99.77 | ||
| S2 | 271.56 | S2 | 134.52 | ||
| S | 16.48 | S | 11.60 | ||
| N | 11 | n | 13 | ||
EE: expressed emotion.
Since the normal distribution of the samples could not be checked, the data was analyzed using Mann-Whitney's non-parametric U-test method. Mann-Whitney's U also suggested a statistical significance of P≤.05, confirming the significant difference between the best-informed relatives with less emotion expressed, and those with less cultural competence. That is to say, the ones whit etiological inappropriate explanation of schizophrenia presented a higher EE than the others.
DiscussionThis research studied the cultural consensus about etiology of schizophrenia and its possible relation with high EE. The hypothesis of this study sustained that there is a link between the cultural believes about schizophrenia etiology and high EE. And, as it's been shown, the comprehension about etiology has an impact on family expression of EE. Best-informed relatives express less EE. The sample size of relatives contemplated for this study (n=40) was similar to the number of relatives included in other studies that analyzed family beliefs about the schizophrenia etiology, such as those performed by Lindgren et al.23 in Maryland (n=40), in Saudi Arabia (n=37) by Wahass et al.24, and in United Kingdom (n=52) by Kirov et al.25 The number of participants even matches with studies about EE in families of people with schizophrenia such as Guidorizzi's et al. (n=30) in 2012.26
Unlike two decades ago, a large number of people around the world knows a lot about mental disorders;27 this has led to a shift of greater acceptance and more humanitarian attitudes towards these people. However, as with everything else, there are several ways to understand these conditions. On one hand, there is the knowledge based on the scientific information available; and on the other, the empirical knowledge from the individual experiences build up by life itself.
Being directly involved with a person with a mental disorder allows people to understand the reality of this illness in a deeper way. This affirmation is sustained by studies like the one of Magliano et al.,10 that puts into evidence that family members and health professionals are more effective in identifying schizophrenia (>70%) compared to the general population. However, relationship or closeness does not exempt any individual from having a deficient understanding of this mental condition.
The lack of knowledge resulting from the absence of information or misinformation about schizophrenia, usually generates negative attitudes or social rejection against people who live with it.8 The attitude of rejection or acceptance towards people with a mental disorder will depend on how people understand their condition.6
Regarding the etiology of schizophrenia, in this study, the cause with the highest number of mentions was emotional trauma in childhood (16%), followed by biological-hereditary factors and then, by other variables such as emotional problems, head trauma, mistreatment, and divine will. The attribution of “emotional trauma”, a social-contextual variable, as the main cause of schizophrenia matches with what was reported in Italy, by Magliano et al.,10 where environmental and psychosocial causes predominated as the determinant onset of the disorder, according to more than 68% of respondents.
These results differ from the ones obtained, for example, in an European research where Ruiz et al.,8 that showed a tendency to explain the etiology of the disorder from a medical perspective, under terms of a biological approach in 68% of the cases. Towsend28 argued that studies made in Anglo-Saxon and European societies tended to give more importance to the biological factors that explain the disease, unlike Latin or African populations studies, where the emphasis was placed mostly on non-medical explanations. Either way, it is relevant to clarify that, although in the Spanish study the etiological cause of schizophrenia was a biological factor, the mention of childhood trauma (23%) was also found in a significant proportion of mentions. Nevertheless, though in this study the biological-hereditary factor took second place in mentions, the medical-scientific understanding of the disease was not discarded and had a predominant place within the cultural consensus: inheritance, neurological problems, brain substances and labor complications were the other biological variables that made up the cultural consensus. This allows to consider that, even though there is a discrepancy of the order of the causes, explanations are consistent in both latitudes.
Concerning religious factors, it is to notice that in this study, magical-religious explanations were also part of the cultural consensus about the etiological explanations of the disease. This holds the premise that Mexico remains as a significantly religious country. Studies about religiosity in Mexicans, has reported that religious beliefs, magic, witchcraft, horoscopes, energies or amulets, are common ideas in almost 78% of the population.29 However, it should be clarified that divine will was not the most prevalent answer within the cultural agreement. The difference between the scientific and the magical-religious understanding in this research, compared to the one performed in the 1970s in Mexico,6 where magical-religious explanations prevailed, could be due to the psychoeducational advance in the population studied.
The Mexican Psychiatric Association (APM) and the Psychiatric Association of Latin America (APAL) argue that religious explanations of mental phenomena such as schizophrenia come from the cultural contexts of the territories in which they occur.30 Some studies from different latitudes suggest that religious beliefs are highly used to cope with the stress that dealing with an illness like schizophrenia can cause.
In this regard, various research has shown that religious interpretations of the disease, help people to find a positive prospective on the lives of individuals and their families. Studies in people with severe mental illness in Springfield, Missouri,31 and Maryland,23 found that a significant percentage of people referred that religion had helped them a lot to deal with their disorder. Similarly, in samples of patients with schizophrenia from Saudi Arabia (n=37),24 or in United Kingdom (n=52),25 indicated that religion was their external support to their condition, since it helped them to deal with their treatment. Even some of these studies claimed that these people had a better understanding and treatment adherence than those who didn’t have the religious support.32
Mental health disciplines like psychology and psychiatry, have an important relation with religious beliefs33 as these are important expressions of narratives, symbolisms, and traditions that give meaning to people's lives. Therefore, religion may help people with schizophrenia to encourage their recovery.34 However, the abundant presence of magical-religious attributions in this mental illness, can also increase prejudgments against people with the diagnosis, due to preconceived ideas given by superstition or ignorance.
The impact of this phenomena allows to recognize the possible harm to health associated with the over explanation of the disease based on spiritual beliefs and practices.35 While some people are helped by their faith, others are highly stigmatized.34 Studies like Lopez's in 2016, showed that 57% of the total of participants, considered that the representation of their disease was influenced by their spiritual beliefs, 31% in a positive way and 26% in a negative one.7 It is evident that the overrepresentation of the disease in exclusively religious terms, can be detrimental to the life of the person as they privilege their attention in religious responses over the medical care of their condition.
Although it is scientifically recognized that schizophrenia has a multifactorial explanation and that there is not only one factor by which its emergence can be fully understood,36 nowadays, the prevailing paradigm is the biological explanation. However, the nature of Mexican culture is often defined as religiously ritualistic and festive despite being a secular country.37 This form of spirituality could not be reduced by official secularity38 and perhaps it explains this double reverse conception of mental disorders, despite the constant effort in psychoeducation by medical institutions and specialists.
In a previously mentioned research, carried out by Villaseñor et al.11 in the city of Guadalajara, it was found that 27% of the participants attributed the etiology of the disease to drug use, an idea that coincides with the results of Ruiz et al.8 in Spanish population; however, in the present study, drug abuse was not found to be a trigger for schizophrenia. According to the DSM-5, the use of drugs and psychoactive substances has a high rate of comorbidity with the appearance of schizophrenia, but this diagnosis should not be confused with the one of drug-induced psychosis.
Nervousness or head trauma, coincide with the variables mentioned in the study of the Civil Hospital of Guadalajara11 as triggers for the disease. Although these ideas are not variables that significantly appear on the review of the schizophrenia causes in scientific publications, they are not necessarily ruled out possibilities. Nervousness is a cultural experience that in Mexico expresses an emotional discomfort associated with anguish or anxiety. It is possible that relatives perceive this sensation as a trigger for schizophrenia, associating it with a form of prodromal or residual symptom of the disorder. Similarly, a possible head injury could validate the appearance of a serious mental disorder in its involvement with the alteration of a larger structure.
The fact that emotional trauma in childhood, emotional problems, and mistreatment were considered as explanations for schizophrenia, reflects a cultural sensitivity in the sample of relatives included in the present study. To think that a life full of traumatic experiences, a difficult childhood, family violence and family indifference, destroys the psyche in such a striking way is not actually wrong. Studies that have focused their analysis on contextual variables, explain the etiology of schizophrenia based on helplessness, marginalization, failed family communication, traumatic childhood experiences, among others. It is worth mentioning that family trauma was also the most important variable in Magliano's study in Italy.10
As for the EE, 45% of relatives with the role of caregivers of the person with schizophrenia presented a high EE and it was precisely this percentage of people who provided an understanding of the etiology that did not match the cultural consensus of this study. The percentage of relatives identified with high EE matches with the data found in another research in Mexico,19 where 42% of the people showed high EE.
The fact that a significant association has been found between EE and those who live with the person with schizophrenia confirms the theory of EE, which states that this phenomenon falls on those who spend more time with the patient and have bigger responsibilities in his or her caregiving. This study also corroborates the statement of Barrowclough et al.15 and Cozolino et al., 39 which argues that relatives with high EE seem less informed about schizophrenia. This research found a significant difference among relatives who presented a higher scientific knowledge of schizophrenia and expressed lower EE, over those who showed a lack of information about the disorder and expressed higher EE (t=–9.15; P<.01; Mann-Witney's U=1.00; P<.01).
Although this study did not find a significant relation between uninformed people and educational level, other studies such as Kurihara et al.12 found that relatives who assigned supernatural attributions to the development of schizophrenia had less education. Regardless the educational level of an individual, psychoeducational interventions can achieve that a person, nevertheless of the variables that define them, may standardize their beliefs40 with the scientific evidence about schizophrenia, and with this have a greater acceptance of the person and their disease.
ConclusionsThis group of relatives of people with schizophrenia in western Mexico proposes a cultural agreement sustained by 3 cores: emotional trauma, biological-scientific notions, and religiosity. Identifying this cultural consensus provided an important insight into the condition and proximity areas to understand how the vision of the causes of the disease is built up and address them with more precise psychoeducational methods. Understanding the core of the cultural consensus on schizophrenia, mental health specialists will have better tools to identify this knowledge and demystify those that are counterproductive to the lives of these people.
The present research showed that the less scientific knowledge about schizophrenia, the more expressed emotion. The limitations of this study were centered on the small sample that we were able to include and the methodology that did not allow these findings to be generalized to other family groups. The importance of psychoeducation is highlighted to promote scientific knowledge of mental disorders in order to reduce high EE. It is urgent to identify cultural consensus on this condition and to re-educate beliefs that might be harmful or stigmatizing to people diagnosed with schizophrenia.
FundingThe present research work has not received specific support from public sector agencies, commercial sector or non-profit entities.
Conflict of interestsWe have no known conflict of interests to disclose.