Treatment of mental disorders is carried out through of drugs that are associated with hyposalivation. The study assessed the oral and salivary profiles of mental disorder patients undergoing drug treatment.
Material and methodsA cross-sectional study, it involved participants over 18 years with mental disorders. Data collection included demographic, clinical, and oral health assessments, such as salivary flow, pH, and buffering capacity analyses.
ResultsOf the 50 participants, 68% exhibited salivary alterations, with predominance of women. Schizophrenia was prevalent, with most patients taking three or more medications daily. Comorbidities were more common in the salivary alterations group. Salivary flow at rest was significantly lower in the group with alterations. While plaque index and tongue coating were similar in both groups, stimulated sialometry was lower in the alteration group.
ConclusionsXerostomia complaints were prevalent, indicating salivary dysfunction in psychiatric drug users, impacting oral health parameters like plaque index, tongue coating, pH, and buffering capacity.
El tratamiento de los trastornos mentales se lleva a cabo a través de medicamentos que están asociados con la hiposalivación. El estudio evaluó los perfiles orales y salivales de los pacientes con trastornos mentales sometidos a tratamiento farmacológico.
Material y métodosUn estudio transversal, que involucró a participantes mayores de 18 años con trastornos mentales. La recopilación de datos incluyó evaluaciones demográficas, clínicas y de salud bucal, como el flujo salival, el pH y el análisis de la capacidad de amortiguación.
ResultadosDe los 50 participantes, el 68% presentó alteraciones en la saliva, con predominio de mujeres. La esquizofrenia fue prevalente, con la mayoría de los pacientes tomando tres o más medicamentos diarios. Las comorbilidades fueron más comunes en el grupo con alteraciones en la saliva. El flujo salival en reposo fue significativamente más bajo en el grupo con alteraciones. Si bien el índice de placa y el recubrimiento lingual fueron similares en ambos grupos, la sialometría estimulada fue más baja en el grupo con alteraciones.
ConclusionesLas quejas de xerostomía fueron prevalentes, lo que indica disfunción salival en usuarios de medicamentos psiquiátricos, lo que afecta los parámetros de salud oral como el índice de placa, el recubrimiento lingual, el pH y la capacidad de amortiguación.
Mental disorders (MD) manifest as significant disturbances in an individual's cognition, emotional regulation, or behaviour, reflecting dysfunction in psychological, biological, or developmental processes underlying mental functioning.1 Treatment typically involves pharmacological intervention, where antipsychotics, anxiolytics, antidepressants, and mood stabilizers constitute the primary drug classes. Notably, these medications are commonly associated with xerostomia and hyposalivation due to their interference with the autonomic nervous system, which regulates salivary production.2
Saliva, crucial for maintaining oral balance with a pH between 6.5 and 7.4, exerts a range of functions such as tissue repair, oral lubrication, pH maintenance, food bolus formation, antimicrobial actions, and protection against demineralization.3 Hyposalivation can adversely impact oral microbiota, salivary protection mechanisms, nutritional status, phonation, taste, and increase plaque and tongue coating.4,5 The recommended diagnostic tool for hyposalivation is sialometry, involving the collection and measurement of total saliva at rest and during stimulation.6 Additionally, the xerostomia inventory serves as a clinical tool to gauge the dry mouth sensation and its impact on an individual's well-being.7
Despite the well-established connection between medications and hyposalivation, there is a notable lack of studies characterizing the oral and salivary profile of individuals with mental disorders, particularly those undergoing pharmacological therapy. Therefore, this study aims to assess the oral and salivary profile of patients with mental disorders under pharmacological therapy, utilizing salivary flow measurement and a xerostomia questionnaire.
Materials and methodsThe study employed a prospective cross-sectional observational design with a convenience sample comprising participants over 18 years old diagnosed with mental disorders (MD) and undergoing psychiatric medication. Recruitment transpired over a year at a psychiatric inpatient clinic. Exclusion criteria comprised individuals subjected to head and neck radiotherapy, diagnosed with Sjögren's syndrome, and those unable to complete the protocol. The examiner underwent calibration facilitated by an experienced professional calibrator, and the project obtained approval from the Human Research Ethics Committee (Opinion No. 21300719.6.0000.5243).
Demographic and clinical data collectionDemographic and clinical data, acquired through interviews and medical records, encompassed gender, race, age, medical diagnosis, comorbidities, addictive habits, medication use, and dry mouth complaints. Only smokers were considered for addictive habits, given restrictions on alcohol and illicit drug contact. Medications were categorized by daily dosage (1, 2, 3, or more) and drug class (hypnotic, anxiolytic/sedative, antidepressant, and antipsychotic).
Salivary profile assessmentSalivary quality and flow were evaluated by collecting total saliva without and with stimulation.8 Sialometry was conducted in the morning following pre-test instructions. Unstimulated and stimulated flow rates below 0.2mL/min and 0.7mL/min, respectively, were deemed low flow rates.8 Participants were categorized into two groups based on salivary analyses: those with and without salivary alteration, defined by hyposalivation or xerostomia. Salivary pH and buffer capacity were measured during stimulated saliva collection, with values considered normal between 6.8 and 7.2 for pH and buffer capacity.9
Xerostomia questionnaireParticipants reporting dry mouth underwent the xerostomia inventory, featuring 11 questions with a scoring range of 11–55, higher scores indicating greater xerostomia severity.10
Oral profile assessmentDental bacterial plaque formation was assessed using the simplified oral hygiene index (IHOS), classifying results as good, fair, or poor.11 Tongue coating was evaluated using a coating index based on affected area, ranging from 0 (no coating) to 4 (more than two-thirds of the tongue).12 An intraoral examination was conducted to assess mucosal and oral structures.
Statistical analysisStatistical analyses utilized SPSS 22.0, employing proportions for categorical variables and means, standard deviations, minimum-maximum values, and medians for numerical variables. Fisher's exact test assessed differences in categorical variables, and Student's t-test compared age means between groups. Significance was established at p<0.05 for all analyses.
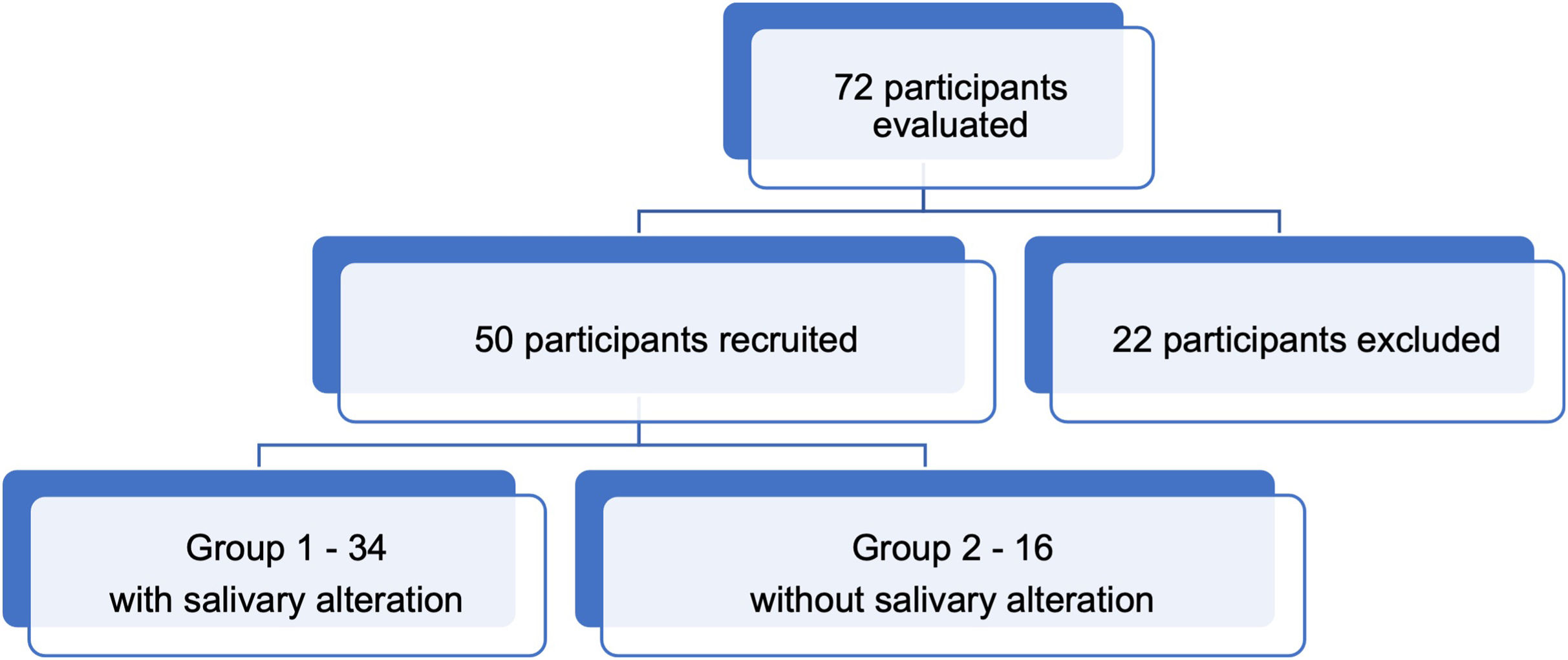
ResultsOut of the initial 72 participants assessed, 22 were excluded due to an inability to complete the prescribed treatment and tests, resulting in the inclusion of 50 participants. Among these, 34 (68%) exhibited salivary alterations (Group 1 – G1), while 16 (32%) displayed no salivary alterations (Group 2 – G2). Within G1, 7 participants (21%) reported solely xerostomia without hyposalivation (Fig. 1).
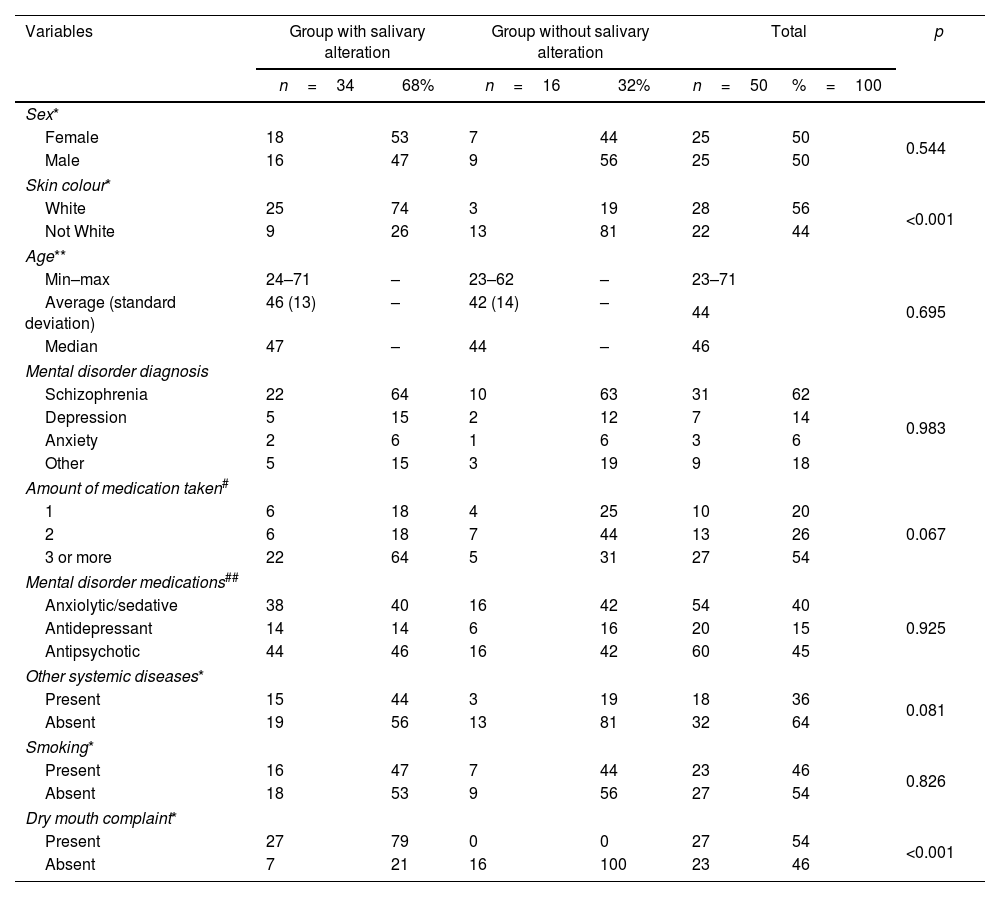
Examining demographic data, it was noted that a majority of G1 comprised women (18–53%), whereas G2 was predominantly composed of men (9–56%). White skin colour prevailed in G1 (25–74%), whereas non-white skin colour predominated in G2 (13–81%), showing a significant difference (p<0.001). The age range of the total sample spanned from 23 to 71 years, with an average age exceeding 40 in both groups (Table 1). In terms of mental disorders, schizophrenia constituted the diagnosis in over 60% of cases in both groups. G1 exhibited a higher proportion of participants (64%) taking three or more medications, while G2 had 44% of participants taking only two medications daily (p=0.067). Antipsychotics were the most commonly used medications in both groups, accounting for 46% and 44% of medications in G1 and G2, respectively. Participants were queried about comorbidities such as hypertension and diabetes, with both groups predominantly indicating an absence of comorbidities; however, G1 exhibited a higher prevalence of other diseases (p=0.081). Regarding tobacco use, 53% of G1 participants and 56% of G2 participants denied the habit.
Distribution of the sample according to demographic and clinical profile.
| Variables | Group with salivary alteration | Group without salivary alteration | Total | p | |||
|---|---|---|---|---|---|---|---|
| n=34 | 68% | n=16 | 32% | n=50 | %=100 | ||
| Sex* | |||||||
| Female | 18 | 53 | 7 | 44 | 25 | 50 | 0.544 |
| Male | 16 | 47 | 9 | 56 | 25 | 50 | |
| Skin colour* | |||||||
| White | 25 | 74 | 3 | 19 | 28 | 56 | <0.001 |
| Not White | 9 | 26 | 13 | 81 | 22 | 44 | |
| Age** | |||||||
| Min–max | 24–71 | – | 23–62 | – | 23–71 | 0.695 | |
| Average (standard deviation) | 46 (13) | – | 42 (14) | – | 44 | ||
| Median | 47 | – | 44 | – | 46 | ||
| Mental disorder diagnosis | |||||||
| Schizophrenia | 22 | 64 | 10 | 63 | 31 | 62 | 0.983 |
| Depression | 5 | 15 | 2 | 12 | 7 | 14 | |
| Anxiety | 2 | 6 | 1 | 6 | 3 | 6 | |
| Other | 5 | 15 | 3 | 19 | 9 | 18 | |
| Amount of medication taken# | |||||||
| 1 | 6 | 18 | 4 | 25 | 10 | 20 | 0.067 |
| 2 | 6 | 18 | 7 | 44 | 13 | 26 | |
| 3 or more | 22 | 64 | 5 | 31 | 27 | 54 | |
| Mental disorder medications## | |||||||
| Anxiolytic/sedative | 38 | 40 | 16 | 42 | 54 | 40 | 0.925 |
| Antidepressant | 14 | 14 | 6 | 16 | 20 | 15 | |
| Antipsychotic | 44 | 46 | 16 | 42 | 60 | 45 | |
| Other systemic diseases* | |||||||
| Present | 15 | 44 | 3 | 19 | 18 | 36 | 0.081 |
| Absent | 19 | 56 | 13 | 81 | 32 | 64 | |
| Smoking* | |||||||
| Present | 16 | 47 | 7 | 44 | 23 | 46 | 0.826 |
| Absent | 18 | 53 | 9 | 56 | 27 | 54 | |
| Dry mouth complaint* | |||||||
| Present | 27 | 79 | 0 | 0 | 27 | 54 | <0.001 |
| Absent | 7 | 21 | 16 | 100 | 23 | 46 | |
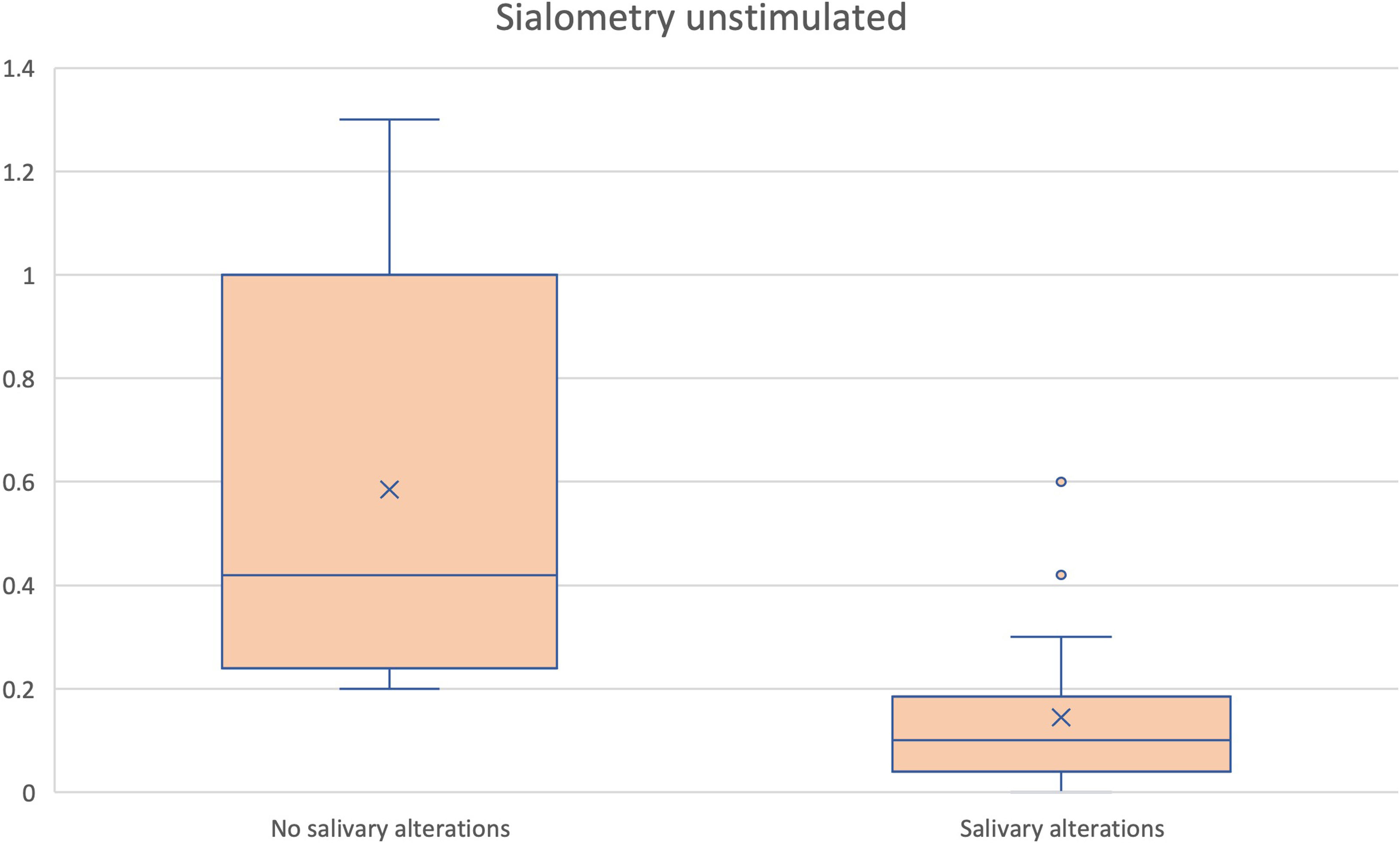
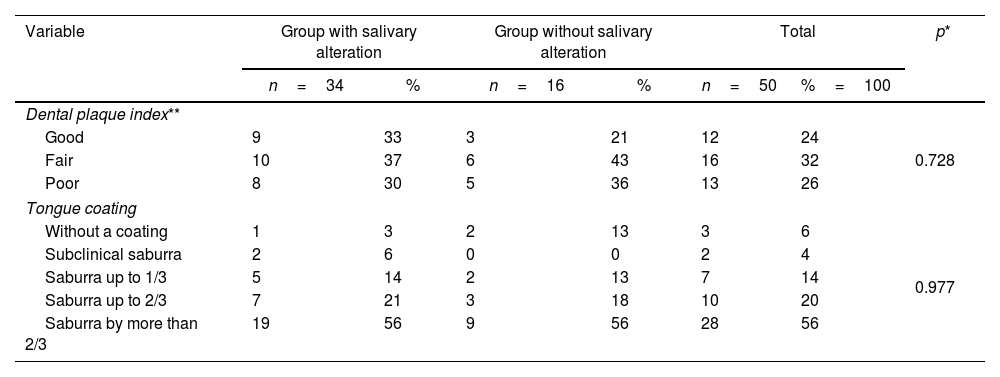
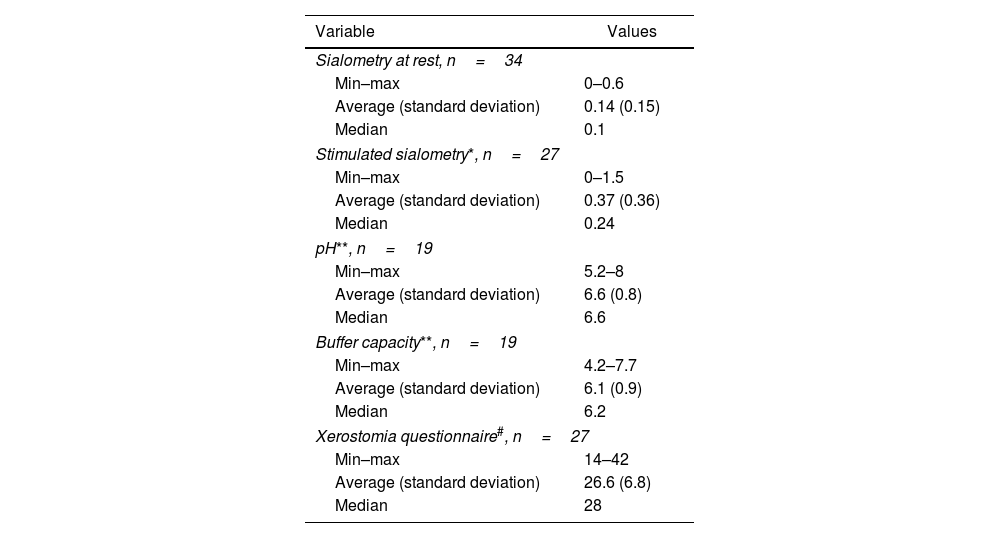
Resting sialometry results were collected in both groups, ranging from 0.2 to 1.3mL/min, with a mean of 0.6mL/min in G2 and 0 to 0.6mL/min in G1, showing a significant difference (p<0.001) (Fig. 2). The dental plaque index was regular, with the majority in both groups exhibiting grade 4 saburra (Table 2). No oral lesions were identified during the extraoral and intraoral physical examination. Data pertaining to salivary alterations, obtained through resting and stimulated sialometry, xerostomia, pH index, and saliva buffering capacity, are detailed in Table 3.
Description of the sample according to the oral profile based on the plaque index and tongue coating.
| Variable | Group with salivary alteration | Group without salivary alteration | Total | p* | |||
|---|---|---|---|---|---|---|---|
| n=34 | % | n=16 | % | n=50 | %=100 | ||
| Dental plaque index** | |||||||
| Good | 9 | 33 | 3 | 21 | 12 | 24 | 0.728 |
| Fair | 10 | 37 | 6 | 43 | 16 | 32 | |
| Poor | 8 | 30 | 5 | 36 | 13 | 26 | |
| Tongue coating | |||||||
| Without a coating | 1 | 3 | 2 | 13 | 3 | 6 | 0.977 |
| Subclinical saburra | 2 | 6 | 0 | 0 | 2 | 4 | |
| Saburra up to 1/3 | 5 | 14 | 2 | 13 | 7 | 14 | |
| Saburra up to 2/3 | 7 | 21 | 3 | 18 | 10 | 20 | |
| Saburra by more than 2/3 | 19 | 56 | 9 | 56 | 28 | 56 | |
Distribution of the sample according to the salivary profile of the group with salivary alterations.
| Variable | Values |
|---|---|
| Sialometry at rest, n=34 | |
| Min–max | 0–0.6 |
| Average (standard deviation) | 0.14 (0.15) |
| Median | 0.1 |
| Stimulated sialometry*, n=27 | |
| Min–max | 0–1.5 |
| Average (standard deviation) | 0.37 (0.36) |
| Median | 0.24 |
| pH**, n=19 | |
| Min–max | 5.2–8 |
| Average (standard deviation) | 6.6 (0.8) |
| Median | 6.6 |
| Buffer capacity**, n=19 | |
| Min–max | 4.2–7.7 |
| Average (standard deviation) | 6.1 (0.9) |
| Median | 6.2 |
| Xerostomia questionnaire#, n=27 | |
| Min–max | 14–42 |
| Average (standard deviation) | 26.6 (6.8) |
| Median | 28 |
Individuals with mental disorders often face a higher prevalence of risk factors for oral alterations compared to the general population. This can be attributed to medication side effects, inadequate self-care, limited access to healthcare services, a negative attitude towards professional healthcare, and reluctance in dental treatments.13 Despite the awareness within the health sector about these challenges, no studies in the literature specifically address salivary alterations in this population resulting from mental disorders and their associated medications.
Results from this study indicate that a majority of the sample exhibited salivary alterations, including hyposalivation and/or xerostomia. Comparison between the two studied groups revealed a higher prevalence of salivary alterations in females, aligning with existing literature suggesting that salivary alterations are more common in women.8,14–21 While many studies focus on gender8,14–21 and age,2,4,14–16,18–23 skin color20 was considered in this study due to Brazil's diverse population.
While various studies have explored xerostomia and hyposalivation, this study diverges in terms of average age due to the inclusion of young adults.13,24,25 The prevalence of mental disorders is noted to initiate at an earlier age, with the first episodes of mood disorders expected around 20.5 years.24 Schizophrenia emerged as the most prevalent disorder in both groups, a complex and chronic condition with debilitating effects on patients and families.26 The high prevalence observed in this study is attributed to the critical diagnoses typical of those admitted to psychiatric clinics.
One of the primary risk factors for xerostomia and hyposalivation is medication use, with polypharmacy significantly influencing salivary flow.16,19,22,25,27 The study demonstrated a higher number of participants in the group with salivary alterations using three or more medications, reinforcing findings from similar studies.16,19,22,25,27 Psychotropic medications, particularly antipsychotics, were strongly associated with xerostomia in schizophrenia patients.
Comorbidities such as hypertension and diabetes, along with their respective medications, were considered potential contributors to salivary alterations.28,29 Smoking, a known risk factor for xerostomia,21 was reported by participants, though no significant difference was observed between smokers and non-smokers. Current classifications distinguish between xerostomia and salivary gland hypofunction, acknowledging their potential independence.15,22 Psychosomatic effects may explain the perceived dry mouth sensation, even in the absence of reduced salivary flow.17 A notable finding was that 21% of participants with normal sialometry values still reported xerostomia.
The study highlights the disparity in prevalence rates when separately considering xerostomia and hyposalivation. In this study, the coexistence of both conditions was observed in 40% of individuals. Poor oral hygiene, reflected in plaque index and tongue coating, was prevalent in both groups, possibly linked to the patients’ underlying mental health conditions affecting personal care habits.13,30 Salivary changes were found to significantly impact various aspects of oral health and overall well-being, including patient satisfaction, tooth loss, general health status, and psychological stress. Xerostomia and hyposalivation were strongly associated with altered taste, feelings of tension, difficulty relaxing, less satisfying life, impaired functionality, embarrassment, meal interruptions, and difficulty performing routine tasks.19
Study limitations included challenges in patient cooperation during tests, particularly sialometry. The study's sample size led to group imbalances, affecting statistical analysis. Nevertheless, the originality and relevance of this research in addressing the oral health challenges of patients with mental disorders underscore its significance in the literature. Future studies could explore alternative sialometry techniques and involve a larger participant pool to enhance the robustness of findings.
ConclusionsIndividuals undergoing psychiatric treatment commonly experience salivary alterations, particularly among females with white skin, averaging 44 years old, and diagnosed with schizophrenia. Those taking more than three medications and having comorbidities such as Diabetes Mellitus and/or Hypertension are also prevalent in this group. Descriptive analysis reveals a convergence of these factors contributing to reduced salivary production and/or xerostomia, diminished pH and buffering capacity, elevated plaque index, and increased tongue coating. Implementing treatment protocols is imperative to alleviate or mitigate the observed signs and symptoms in these patients, thereby enhancing their oral health and overall quality of life.
Ethical approvalThe study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee under CAAE register number: 21300719.6.0000.5243 for studies involving humans.
FundingThis research received no external funding.
Conflicts of interestsThe authors declare no conflict of interest.
Master's thesis presented with the title “Analysis of the oral and salivary profile of patients with mental disorders pharmacological therapy” on May 31, 2023.