Partial tears of the rotator cuff were initially described by Codman in 1934.1 However, it was not until 2001 that Snyder coined the term PASTA to describe an avulsion-type injury on the articular side of the supraspinatus tendon, causing pain and functional disability, for which some patients had to undergo surgery for symptom relief and for avoidance of disease progression.2 The advent of magnetic resonance imaging allowed confirming that articular side tears are much more frequent than bursal side ones, questioning the strictly mechanical concept by Neer, who said that the rotator cuff damage was because the subacromial impingement.3 Many surgical strategies for PASTA lesions have been designed, all of which consist of re-attachment the tendon in the greater tuberosity either transtendon or completing it through the bursal side. Snyder started from the premise that what he observed in the arthroscopic view of the glenohumeral joint, was the supraspinatus tendon; consequently, any lesion in the crescent area, distal to the rotator cable seen through the articular side was considered as a tendinous lesion.
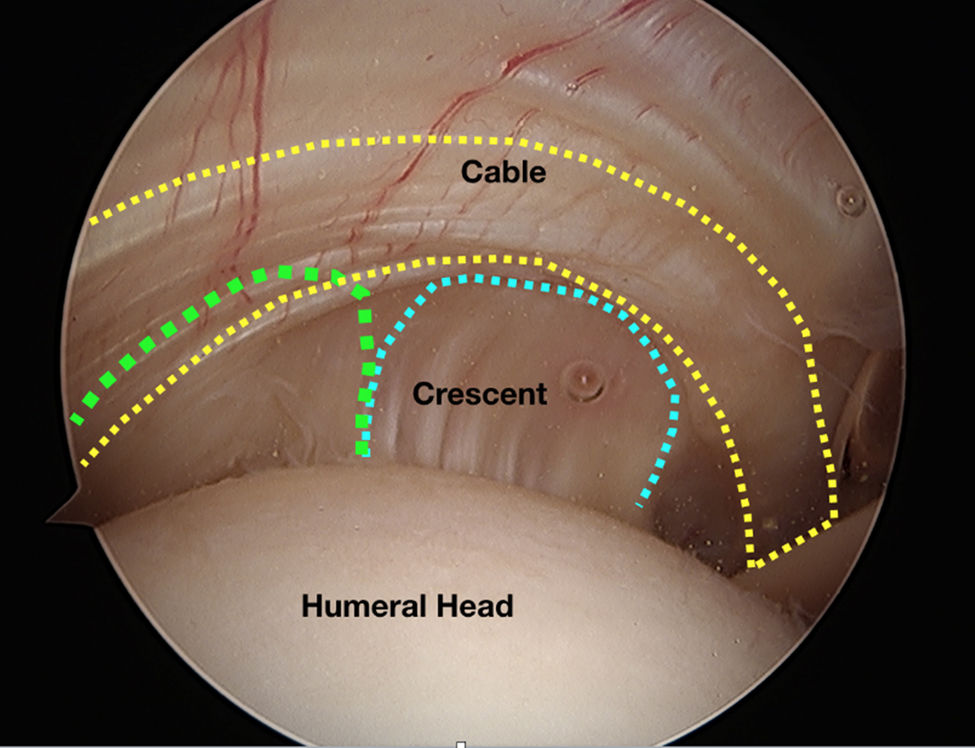
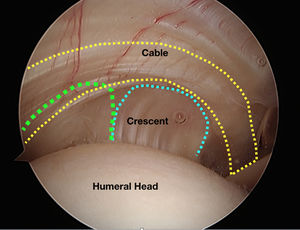
Recent anatomic descriptions by Mochizuki and Nimura have shown two important aspects of tendinous supraspinatus and infraspinatus insertions and their distribution area in the greater tuberosity.4,5 First, the insertion of the supraspinatus occupies a smaller area in the greater tuberosity than previously thought; it is located anteriorly and laterally and has no insertional relation to the medial border adjacent to the articular cartilage. Second and even more important, the articular capsule is the anatomic structure directly related to the articular cartilage, occupying a 20%-60% area of the greater tuberosity; its insertion is thinner in the anterior region and corresponds laterally with the supraspinatus insertion. Thus, intraarticular supraspinatus and infraspinatus visualization indeed correspond to the articular capsule (Figure 1). This finding was confirmed through arthroscopic assessments by Tanaka, who has found that more than 50% of the patients show delamination, leaving no doubt that the deep layer belongs to the articular capsule.6
In view of such evidence, we think the term PASTA should be reassessed, since what actually undergoes avulsion is the superior capsule-ligament complex, as had been previously suggested by Pouliart7. PASCA (Partial Articular Superior Capsule Avulsion) would be a more precise term because defines better the anatomy and induces a more rational management of the lesions. This implies that truly tendinous cuff lesions (i.e., injuries of the cuff itself) are those we have defined as bursal injuries, and what underlies such lesions is the articular capsule.
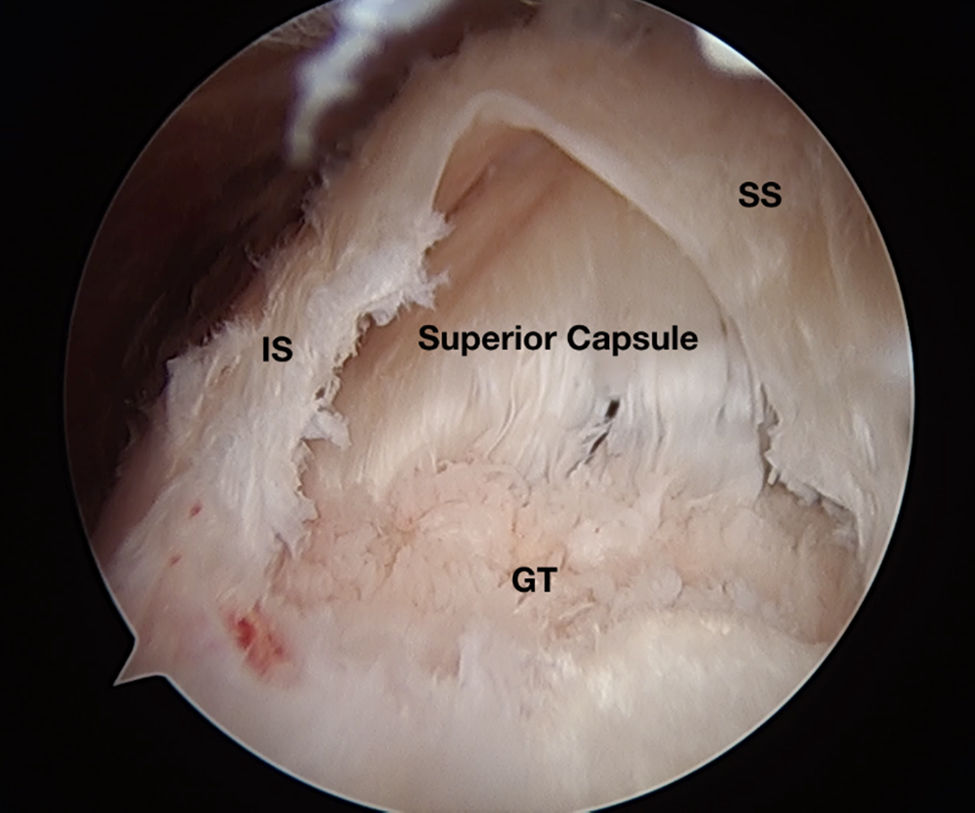
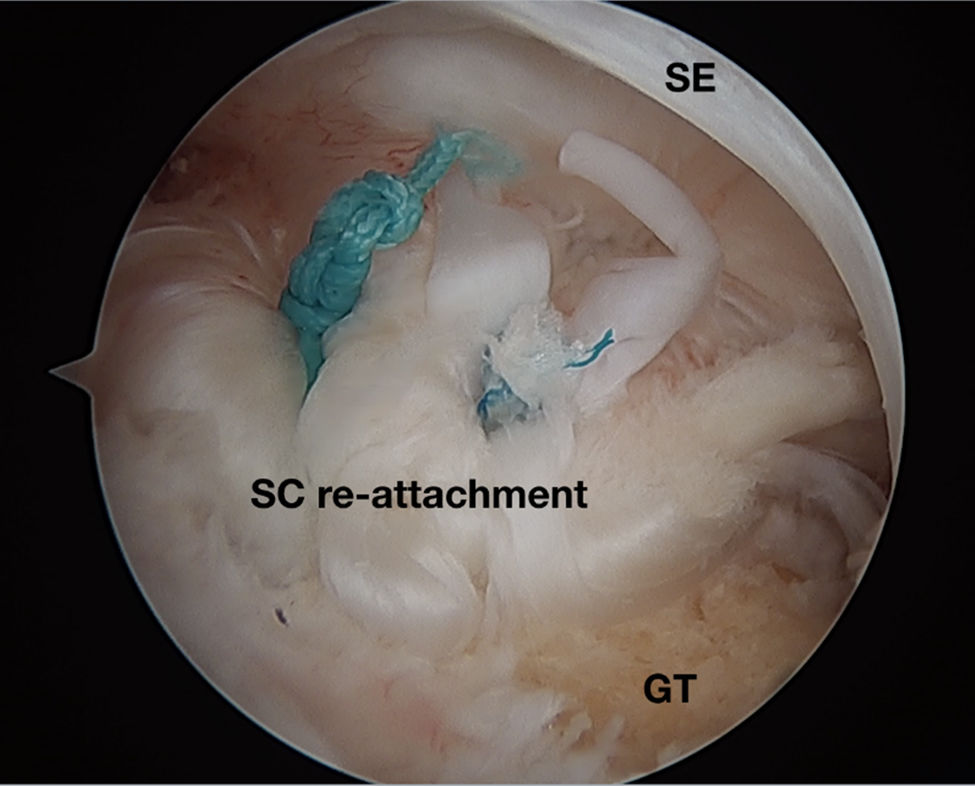
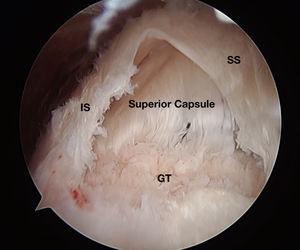
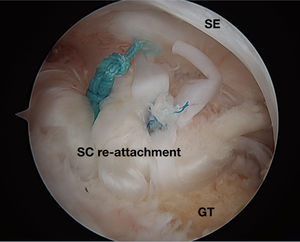
For delaminated tears (Figure 2), it would be reasonable to plan repairs independent of the medial (capsule) and the lateral rows (supra and infra tendon) (Figure 3), as was proposed by Mochizuki, who considers poor outcomes result from not recognizing this anatomic aspect.8
As described by Adams, the essential lesion is both a tendinous and a capsular injury, which are equally important regarding assessment and repair if we want to improve surgical results.9
Following Hanadás initial description of superior capsular reconstruction in paraplegic patients, Mihata has shown that in whom tendon and capsule have been irreversibly damaged, superior capsule reconstruction is the best option in patients followed up for 4 years.10,11 It acts as a fulcrum and avoids cephalic scape of the humeral head, allowing recovery of shoulder strength and mobility.12,13 Variations using different grafts and techniques -all of them aimed at reconstructing such an important anatomic structure in rotator cuff disease- have been reported.14–16
Despite replacing PASTA by PASCA is a semantic discussion, we do believe it alerts the orthopedics community to the need of reconsidering the anatomic basis of the rotator cuff and capsule insertion, and to be more agreeable with surgical treatment approaches.