Meningioma is the most common primary intracranial tumor, originating from the protective membranes known as the meninges. Specifically, it arises from arachnoid cells attached to the dura mater, making it extra-axial. Meningiomas are characterized by their potential to grow large, cause hyperostosis, and infiltrate or erode bone. They account for about 36% of all brain tumors, with a prevalence ratio of 2:1 between women and men. The problems associated with meningiomas depend on their location, size, and involvement with surrounding tissue structures.
ObjectiveTo develop a perioperative nursing care plan for a patient with WHO grade II atypical meningioma.
MethodsThis study used a case study design and included a review of the literature on WHO grade II atypical meningioma. We used the NANDA, NIC, and NOC maintenance guidelines to complement the Roy Adaptation Model. This approach provided specific diagnoses for developing interventions and publishing results in clinical maintenance practice.
ResultsThe patient was treated for seven days. Postoperatively, the patient reported decreased headache and eye redness, reduced proptosis, controlled infection, and a clean surgical wound with no drainage seepage. By the third day, the Barovac drain was set to 1/2 vacuum, and the lumbar drain was removed by the fifth day. The patient gradually mobilized, reducing the risk of falls.
ConclusionThe Roy Adaptation Model can be effectively used in the nursing care of patients with meningioma. Roy views humans as open and adaptive systems capable of responding to internal and external stimuli throughout their lives.
El meningioma es el tumor intracraneal primario más común, que se origina en las membranas protectoras denominadas meninges. De manera específica procede de las células aracnoideas anexas a la duramadre, lo cual las convierte en extraaxiales. Los meningiomas se caracterizan por su potencial de crecimiento grande, causando hiperostosis, con infiltración o erosión ósea. Representan alrededor del 36% de todos los tumores cerebrales, con una ratio de prevalencia de 2:1 entre mujeres y hombres. Los problemas asociados a los meningiomas dependen de su localización, tamaño y compromiso de las estructuras tisulares circundantes.
ObjetivoDesarrollar un plan de cuidados enfermeros perioperatorios para un paciente con meningioma atípico en estadio ii de la OMS.
MétodosEsta investigación utilizó un diseño de estudio de caso, e incluyó una revisión de la literatura sobre el meningioma atípico en estadio ii de la OMS. Utilizamos las guías de mantenimiento NANDA, NIC y NOC para complementar el modelo de adaptación de Roy. Dicho enfoque aportó diagnósticos específicos para el desarrollo de intervenciones y publicación de resultados en la práctica de mantenimiento clínico.
ResultadosEl paciente fue tratado durante 7 días. Postoperatoriamente, reportó una reducción de la cefalea y enrojecimiento ocular, disminución de la proptosis, control de la infección y limpieza de la herida quirúrgica sin filtración del drenaje. El tercer día se ajustó el drenaje Barovac a medio vacío, retirándose el drenaje lumbar al quinto día. El paciente se movilizó gradualmente, reduciéndose el riesgo de caídas.
ConclusiónEl modelo de adaptación de Roy puede utilizarse de manera efectiva en el cuidado enfermero de los pacientes con meningioma. Roy contempla a los humanos como sistemas abiertos y adaptativos capaces de responder a los estímulos internos y externos a lo largo de sus vidas.
With increasing life expectancy and technological advances, the incidence of brain tumors continues to rise. Meningioma, a primary brain tumor of the central nervous system, is becoming more prevalent, leading to neurological deficits, changes in mental status, and a significant social burden.1,2 Meningiomas account for approximately 36% of all brain tumors, with an incidence estimated at 98 per 100,000 people. The estimated female-to-male ratio is 2:1, and the incidence increases with age.2 Data from National Brain Hospital's medical records from January 2022 to November 2022 reported 86 meningioma cases out of 241 brain tumor cases.3 Gebler et al. found that 90% of meningiomas are located intracranially, supratentorially along the dural venous sinuses, including convex areas (45%), the cerebral falx (26%), the tentorium (9%), and the lateral sphenoid wings (20%).4
Meningiomas grow from the meninges and are typically benign, slow-growing tumors found in the intracranial region. However, they can sometimes be extra-axial malignant, originating from arachnoid cells attached to the dura mater. These tumors can grow large, often producing hyperostosis, infiltration, or bone erosion. According to the World Health Organization (WHO) guidelines (2016) for the classification of central nervous system tumors, meningiomas are classified into three grades: benign (WHO Grade I) comprising 80–90%, atypical (WHO Grade II) making up 10–18%, and malignant (WHO Grade III) around 2–4%.5 Clinical manifestations depend on the tumor's location, size, and impact on surrounding tissue structures. General symptoms can result from edema and increased intracranial pressure (ICP), including headaches, papilledema, nausea, vomiting, seizures, and changes in mental status.6 Local symptoms may arise from damage, irritation, or compression of the brain area where the tumor is located, causing ipsilateral visual disturbances, proptosis, afferent pupillary defects, color vision disturbances, visual field defects, optic disc edema, and eyeball movement disorders. Additional symptoms include hearing loss, smell and speech impairments, limb weakness/hemiparesis, impaired coordination, and sensory disturbances such as anesthesia or paresthesia.7
Management of meningioma depends on the tumor's location and size and is highly individualized due to the variable nature of meningiomas and differences in patient outcomes. Therapeutic options include observation with serial computed tomography (CT) scans or magnetic resonance imaging (MRI) and surgery. For small (<3cm) and asymptomatic tumors, observation is recommended based on guidelines from the European Association of Neuro-oncology (EANO) and the National Comprehensive Cancer Network (NCCN). Surgery is the primary treatment for all types of meningiomas, with goals including palliation and tumor resection.8 Complete resection, which includes removing the tumor, surrounding soft tissue, dura mater border, and involved skull, provides better results and reduces recurrence rates. Nursing care, guided by Roy's Adaptation Theory, involves assessment, diagnosis, intervention, implementation, and evaluation to support patients with neurological disorders to adapt to changes in their health status.9 This case study aimed to develop a perioperative nursing care plan for a patient with WHO grade II atypical meningioma.
Presentation of the case studyData was collected from when the patient entered the outpatient clinic for planned surgery until the patient was discharged after surgery. The patient was asked for consent to participate in the study. The ethical approval number for this study was Ket-196/UN2.F12.D1.2.1/PPM.00.02/2021
Mr. EW is a 33-year-old Javanese. He is married, Muslim, educated in high school, and a farmer. He is addressed Metro Lampung Tengah, Lampung Province. In September–October 2022, routine control patients go to the neurosurgery polyclinic on the 2nd floor of Prof. National Brain Center Hospital. Dr. dr. Mahar Mardjono Jakarta, accompanied by his wife. The neurosurgeon in charge of the patient scheduled the patient for craniotomy surgery on November 2, 2022. The patient was admitted to the 6B operating room to prepare for craniotomy surgery on October 30, 2022, at 16.00 WIB, with complaints of headaches since June 2021. The pain is increasing, as is weakness in the left side of the body, inability to see both eyes and protruding right eye (proptosis/exophthalmos). November 2, 2022, at 07.00 WIB, the patient was taken to the operating room, then the operation was carried out at 07.30 WIB and finished at 16.30 WIB. After the process, the patient was transferred to the Intensive Care Unit (ICU) to stabilize his post-recovery condition. The patient was treated in the ICU for two days. On November 4, 2022, at 08.00 WIB, the patient was moved to surgery room 6B for further treatment until the patient returned for five days.
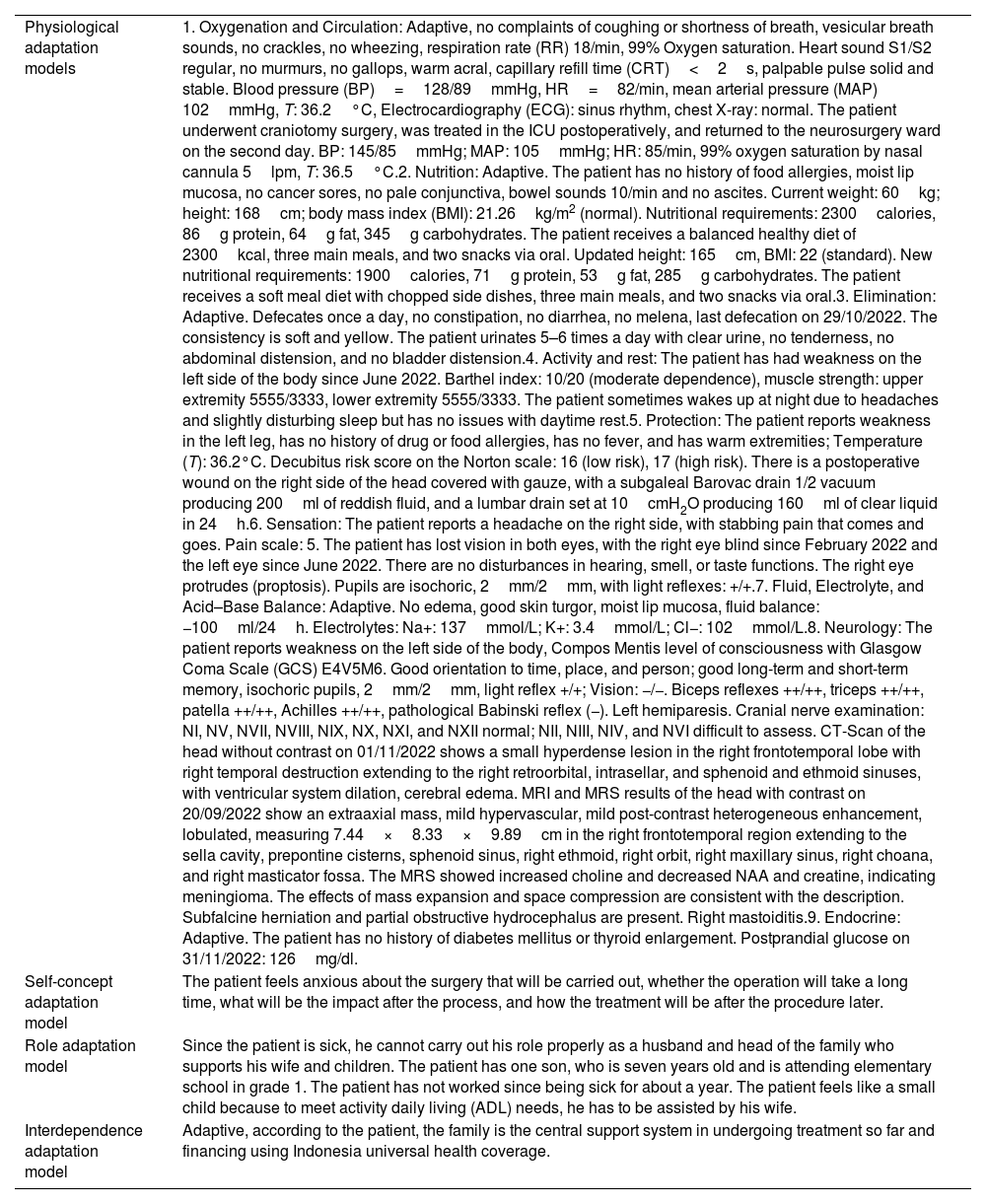
According to Roy's adaptation model, it is necessary to assess the patient's behavior and stimulus.
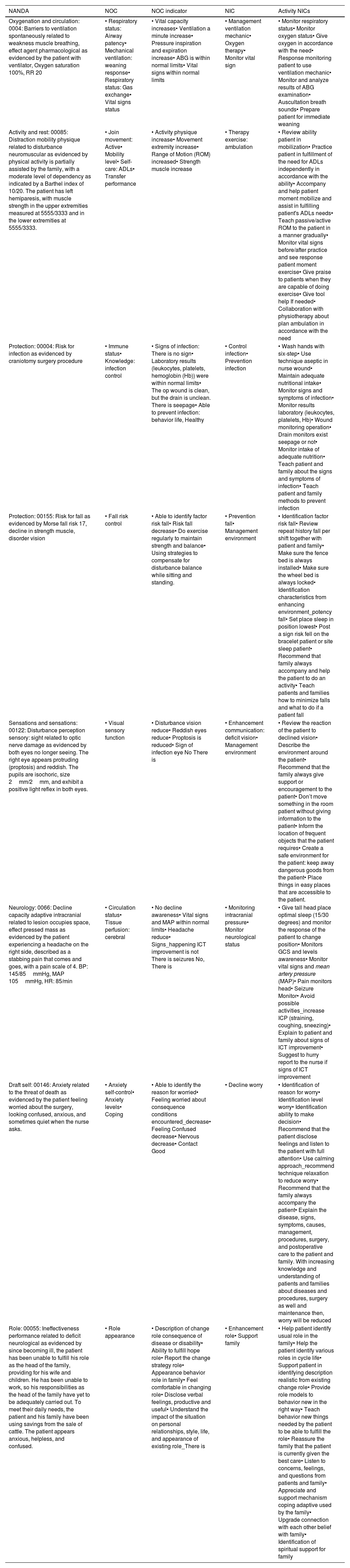
Based on the identified manufacturing diagnoses NANDA, NOC, and NIC, the pattern best suited to the patient's situation is selected and used to create a formation plan, as shown in Tables 1 and 2.
Nursing assessment according to Roy's Adaptation Model: assessment of behavior and stimulus.
| Physiological adaptation models | 1. Oxygenation and Circulation: Adaptive, no complaints of coughing or shortness of breath, vesicular breath sounds, no crackles, no wheezing, respiration rate (RR) 18/min, 99% Oxygen saturation. Heart sound S1/S2 regular, no murmurs, no gallops, warm acral, capillary refill time (CRT)<2s, palpable pulse solid and stable. Blood pressure (BP)=128/89mmHg, HR=82/min, mean arterial pressure (MAP) 102mmHg, T: 36.2°C, Electrocardiography (ECG): sinus rhythm, chest X-ray: normal. The patient underwent craniotomy surgery, was treated in the ICU postoperatively, and returned to the neurosurgery ward on the second day. BP: 145/85mmHg; MAP: 105mmHg; HR: 85/min, 99% oxygen saturation by nasal cannula 5lpm, T: 36.5°C.2. Nutrition: Adaptive. The patient has no history of food allergies, moist lip mucosa, no cancer sores, no pale conjunctiva, bowel sounds 10/min and no ascites. Current weight: 60kg; height: 168cm; body mass index (BMI): 21.26kg/m2 (normal). Nutritional requirements: 2300calories, 86g protein, 64g fat, 345g carbohydrates. The patient receives a balanced healthy diet of 2300kcal, three main meals, and two snacks via oral. Updated height: 165cm, BMI: 22 (standard). New nutritional requirements: 1900calories, 71g protein, 53g fat, 285g carbohydrates. The patient receives a soft meal diet with chopped side dishes, three main meals, and two snacks via oral.3. Elimination: Adaptive. Defecates once a day, no constipation, no diarrhea, no melena, last defecation on 29/10/2022. The consistency is soft and yellow. The patient urinates 5–6 times a day with clear urine, no tenderness, no abdominal distension, and no bladder distension.4. Activity and rest: The patient has had weakness on the left side of the body since June 2022. Barthel index: 10/20 (moderate dependence), muscle strength: upper extremity 5555/3333, lower extremity 5555/3333. The patient sometimes wakes up at night due to headaches and slightly disturbing sleep but has no issues with daytime rest.5. Protection: The patient reports weakness in the left leg, has no history of drug or food allergies, has no fever, and has warm extremities; Temperature (T): 36.2°C. Decubitus risk score on the Norton scale: 16 (low risk), 17 (high risk). There is a postoperative wound on the right side of the head covered with gauze, with a subgaleal Barovac drain 1/2 vacuum producing 200ml of reddish fluid, and a lumbar drain set at 10cmH2O producing 160ml of clear liquid in 24h.6. Sensation: The patient reports a headache on the right side, with stabbing pain that comes and goes. Pain scale: 5. The patient has lost vision in both eyes, with the right eye blind since February 2022 and the left eye since June 2022. There are no disturbances in hearing, smell, or taste functions. The right eye protrudes (proptosis). Pupils are isochoric, 2mm/2mm, with light reflexes: +/+.7. Fluid, Electrolyte, and Acid–Base Balance: Adaptive. No edema, good skin turgor, moist lip mucosa, fluid balance: −100ml/24h. Electrolytes: Na+: 137mmol/L; K+: 3.4mmol/L; Cl−: 102mmol/L.8. Neurology: The patient reports weakness on the left side of the body, Compos Mentis level of consciousness with Glasgow Coma Scale (GCS) E4V5M6. Good orientation to time, place, and person; good long-term and short-term memory, isochoric pupils, 2mm/2mm, light reflex +/+; Vision: −/−. Biceps reflexes ++/++, triceps ++/++, patella ++/++, Achilles ++/++, pathological Babinski reflex (−). Left hemiparesis. Cranial nerve examination: NI, NV, NVII, NVIII, NIX, NX, NXI, and NXII normal; NII, NIII, NIV, and NVI difficult to assess. CT-Scan of the head without contrast on 01/11/2022 shows a small hyperdense lesion in the right frontotemporal lobe with right temporal destruction extending to the right retroorbital, intrasellar, and sphenoid and ethmoid sinuses, with ventricular system dilation, cerebral edema. MRI and MRS results of the head with contrast on 20/09/2022 show an extraaxial mass, mild hypervascular, mild post-contrast heterogeneous enhancement, lobulated, measuring 7.44×8.33×9.89cm in the right frontotemporal region extending to the sella cavity, prepontine cisterns, sphenoid sinus, right ethmoid, right orbit, right maxillary sinus, right choana, and right masticator fossa. The MRS showed increased choline and decreased NAA and creatine, indicating meningioma. The effects of mass expansion and space compression are consistent with the description. Subfalcine herniation and partial obstructive hydrocephalus are present. Right mastoiditis.9. Endocrine: Adaptive. The patient has no history of diabetes mellitus or thyroid enlargement. Postprandial glucose on 31/11/2022: 126mg/dl. |
| Self-concept adaptation model | The patient feels anxious about the surgery that will be carried out, whether the operation will take a long time, what will be the impact after the process, and how the treatment will be after the procedure later. |
| Role adaptation model | Since the patient is sick, he cannot carry out his role properly as a husband and head of the family who supports his wife and children. The patient has one son, who is seven years old and is attending elementary school in grade 1. The patient has not worked since being sick for about a year. The patient feels like a small child because to meet activity daily living (ADL) needs, he has to be assisted by his wife. |
| Interdependence adaptation model | Adaptive, according to the patient, the family is the central support system in undergoing treatment so far and financing using Indonesia universal health coverage. |
Nurses’ assessment of patients with WHO grade II atypical meningioma according to NANDA, NOC, and NIC taxonomy.
| NANDA | NOC | NOC indicator | NIC | Activity NICs |
|---|---|---|---|---|
| Oxygenation and circulation: 0004: Barriers to ventilation spontaneously related to weakness muscle breathing, effect agent pharmacological as evidenced by the patient with ventilator, Oxygen saturation 100%, RR 20 | • Respiratory status: Airway patency• Mechanical ventilation: weaning response• Respiratory status: Gas exchange• Vital signs status | • Vital capacity increases• Ventilation a minute increase• Pressure inspiration and expiration increase• ABG is within normal limits• Vital signs within normal limits | • Management ventilation mechanic• Oxygen therapy• Monitor vital sign | • Monitor respiratory status• Monitor oxygen status• Give oxygen in accordance with the need• Response monitoring patient to use ventilation mechanic• Monitor and analyze results of ABG examination• Auscultation breath sounds• Prepare patient for immediate weaning |
| Activity and rest: 00085: Distraction mobility physique related to disturbance neuromuscular as evidenced by physical activity is partially assisted by the family, with a moderate level of dependency as indicated by a Barthel index of 10/20. The patient has left hemiparesis, with muscle strength in the upper extremities measured at 5555/3333 and in the lower extremities at 5555/3333. | • Join movement: Active• Mobility level• Self-care: ADLs• Transfer performance | • Activity physique increase• Movement extremity increase• Range of Motion (ROM) increased• Strength muscle increase | • Therapy exercise: ambulation | • Review ability patient in mobilization• Practice patient in fulfillment of the need for ADLs independently in accordance with the ability• Accompany and help patient moment mobilize and assist in fulfilling patient's ADLs needs• Teach passive/active ROM to the patient in a manner gradually• Monitor vital signs before/after practice and see response patient moment exercise• Give praise to patients when they are capable of doing exercise• Give tool help If needed• Collaboration with physiotherapy about plan ambulation in accordance with the need |
| Protection: 00004: Risk for infection as evidenced by craniotomy surgery procedure | • Immune status• Knowledge: infection control | • Signs of infection: There is no sign• Laboratory results (leukocytes, platelets, hemoglobin (Hb)) were within normal limits• The op wound is clean, but the drain is unclean. There is seepage• Able to prevent infection: behavior life, Healthy | • Control infection• Prevention infection | • Wash hands with six-step• Use technique aseptic in nurse wound• Maintain adequate nutritional intake• Monitor signs and symptoms of infection• Monitor results laboratory (leukocytes, platelets, Hb)• Wound monitoring operation• Drain monitors exist seepage or not• Monitor intake of adequate nutrition• Teach patient and family about the signs and symptoms of infection• Teach patient and family methods to prevent infection |
| Protection: 00155: Risk for fall as evidenced by Morse fall risk 17, decline in strength muscle, disorder vision | • Fall risk control | • Able to identify factor risk fall• Risk fall decrease• Do exercise regularly to maintain strength and balance• Using strategies to compensate for disturbance balance while sitting and standing. | • Prevention fall• Management environment | • Identification factor risk fall• Review repeat history fall per shift together with patient and family• Make sure the fence bed is always installed• Make sure the wheel bed is always locked• Identification characteristics from enhancing environment_potency fall• Set place sleep in position lowest• Post a sign risk fell on the bracelet patient or site sleep patient• Recommend that family always accompany and help the patient to do an activity• Teach patients and families how to minimize falls and what to do if a patient fall |
| Sensations and sensations: 00122: Disturbance perception sensory: sight related to optic nerve damage as evidenced by both eyes no longer seeing. The right eye appears protruding (proptosis) and reddish. The pupils are isochoric, size 2mm/2mm, and exhibit a positive light reflex in both eyes. | • Visual sensory function | • Disturbance vision reduce• Reddish eyes reduce• Proptosis is reduced• Sign of infection eye No There is | • Enhancement communication: deficit vision• Management environment | • Review the reaction of the patient to declined vision• Describe the environment around the patient• Recommend that the family always give support or encouragement to the patient• Don’t move something in the room patient without giving information to the patient• Inform the location of frequent objects that the patient requires• Create a safe environment for the patient: keep away dangerous goods from the patient• Place things in easy places that are accessible to the patient. |
| Neurology: 0066: Decline capacity adaptive intracranial related to lesion occupies space, effect pressed mass as evidenced by the patient experiencing a headache on the right side, described as a stabbing pain that comes and goes, with a pain scale of 4. BP: 145/85mmHg, MAP 105mmHg, HR: 85/min | • Circulation status• Tissue perfusion: cerebral | • No decline awareness• Vital signs and MAP within normal limits• Headache reduce• Signs_happening ICT improvement is not There is seizures No, There is | • Monitoring intracranial pressure• Monitor neurological status | • Give tall head place optimal sleep (15/30 degrees) and monitor the response of the patient to change position• Monitors GCS and levels awareness• Monitor vital signs and mean artery pressure (MAP)• Pain monitors head• Seizure Monitor• Avoid possible activities_increase ICP (straining, coughing, sneezing)• Explain to patient and family about signs of ICT improvement• Suggest to hurry report to the nurse if signs of ICT improvement |
| Draft self: 00146: Anxiety related to the threat of death as evidenced by the patient feeling worried about the surgery, looking confused, anxious, and sometimes quiet when the nurse asks. | • Anxiety self-control• Anxiety levels• Coping | • Able to identify the reason for worried• Feeling worried about consequence conditions encountered_decrease• Feeling Confused decrease• Nervous decrease• Contact Good | • Decline worry | • Identification of reason for worry• Identification level worry• Identification ability to make decision• Recommend that the patient disclose feelings and listen to the patient with full attention• Use calming approach_recommend technique relaxation to reduce worry• Recommend that the family always accompany the patient• Explain the disease, signs, symptoms, causes, management, procedures, surgery, and postoperative care to the patient and family. With increasing knowledge and understanding of patients and families about diseases and procedures, surgery as well and maintenance then, worry will be reduced |
| Role: 00055: Ineffectiveness performance related to deficit neurological as evidenced by since becoming ill, the patient has been unable to fulfill his role as the head of the family, providing for his wife and children. He has been unable to work, so his responsibilities as the head of the family have yet to be adequately carried out. To meet their daily needs, the patient and his family have been using savings from the sale of cattle. The patient appears anxious, helpless, and confused. | • Role appearance | • Description of change role consequence of disease or disability• Ability to fulfill hope role• Report the change strategy role• Appearance behavior role in family• Feel comfortable in changing role• Disclose verbal feelings, productive and useful• Understand the impact of the situation on personal relationships, style, life, and appearance of existing role_There is | • Enhancement role• Support family | • Help patient identify usual role in the family• Help the patient identify various roles in cycle life• Support patient in identifying description realistic from existing change role• Provide role models to behavior new in the right way• Teach behavior new things needed by the patient to be able to fulfill the role• Reassure the family that the patient is currently given the best care• Listen to concerns, feelings, and questions from patients and family• Appreciate and support mechanism coping adaptive used by the family• Upgrade connection with each other belief with family• Identification of spiritual support for family |
Diagnosis includes the preoperative phase, decreased intracranial adaptive capacity, impaired sensory perception, vision, poor physical mobility, risk of falling, anxiety, and ineffectiveness of role performance. The interventions provided are monitoring intracranial pressure and neurological status, improving communication, reducing vision and therapist mobility, controlling the risk of falling, reducing anxiety, and increasing role performance. Collaborative intervention by infusion of 4×125ml mannitol (iv) and 4×5mg dexamethasone injection (iv), condo gentamicin eye self 3×1, collaboration giving ceftriaxone injection 2×2g (iv). Shortly before the operation, the patient said he was no longer worried, and the patient said he accepted his current condition and accepted the new one.
The patient underwent craniotomy surgery postoperatively and was treated in the ICU room, and on the second day, the patient returned to the neurosurgery ward. Management of the development of the postoperative phase is emphasized by increasing spontaneous ventilation, monitoring vital signs, monitoring signs of increasing ICP, monitoring surgical wounds, monitoring drains for seepage or not, watching for signs of infection in the operating area, freeing up mobilization gradually, controlling the risk of falling and collaboration on the problem of visual sensory perception disorders. With well-planned expert care, we can keep patients free from postoperative complications. The patient was treated for seven days. Postoperatively, the patient said that the headache had decreased, the eye problem had decreased, the proptosis had decreased, and the infection had increased. Namely, there were no signs of disease, the surgical wound was clean, and there was no seepage in the drain. On day three, drain barovac 1/2 vacuum aff; on day 3, five lumbar drains aff mobilized gradually, and the risk of falls decreased.
DiscussionThe patient's intracranial adaptive capacity has decreased due to a meningioma, resulting in increased ICP.10 According to the Monroe-Kellie doctrine, the skull's volume remains constant, meaning that an increase in one component (brain tissue, cerebrospinal fluid, or blood) necessitates a decrease in the others. This imbalance can reduce cerebral blood flow or cause brain herniation.6 Standard ICP ranges from 7 to 15mmHg, and maintaining adequate cerebral perfusion pressure (CPP) is crucial to prevent brain hypoxia and cell death. The patient presented clinical manifestations such as headaches, vision disturbances, and nausea, indicating increased ICP. Specialist nurses must closely monitor such patients, especially post-craniotomy, to manage cerebral edema and prevent complications.
Surgical procedures, including craniotomies, pose a significant risk of infection. Postoperative infections can present symptoms such as redness, persistent edema, pain, increased drainage, fever, and elevated white blood cells.10 Preventive measures are essential, starting with preoperative antibiotic prophylaxis. Administering antibiotics like cefazolin before surgery significantly reduces the risk of surgical site infections (SSI). In this case, the patient received a 2-g cefazolin injection to prevent infection. Effective infection control measures contribute to patient comfort, satisfaction, and reduced hospital stays, improving overall outcomes.
Post-craniotomy patients often experience impaired spontaneous ventilation due to muscle relaxants used during anesthesia, which necessitates mechanical ventilation.10 Studies indicate that a high percentage of post-craniotomy patients require ICU care to manage complications such as seizures, hypertension, and increased ICP.11 In addition, the patient faces impaired sensory perception of vision due to meningioma, leading to vision loss, proptosis, and other eye issues. Imaging studies confirmed the presence and impact of the meningioma, underscoring the need for careful monitoring and management of sensory impairments.
The patient's left-side weakness has led to impaired physical mobility, affecting daily activities.10 Early and structured mobilization is crucial for improving functional status and preventing complications like deep vein thrombosis. Fall prevention strategies include patient education, environmental modifications, and continuous monitoring. The patient also experiences anxiety related to the surgical procedure and its outcomes. Providing education, effective communication, and psychological support can reduce anxiety, improve patient satisfaction, and facilitate recovery. Family involvement is essential for emotional support and helping meet the patient's daily needs.
ConclusionNursing care for meningioma patients who have primary needs such as decreased intracranial adaptive capacity, impaired physical mobility, impaired sensory perception, risk of infection, risk of falls, anxiety, and ineffective role performance can utilize the NANDA, NOC, and NIC taxonomy to complement the Roy Adaptation Model. This approach provides specific diagnoses for developing interventions and evaluating outcomes in clinical nursing practice. The Roy Adaptation Model assumes that the basis of nursing science is understanding the human adaptation process in dealing with life situations. Roy views humans as open and adaptive systems that can respond to stimuli from both internal and external sources. This is evidenced by patients experiencing daily improvements in their condition, reduced complaints, absence of anxiety, and greater acceptance of their current role and condition. Consequently, the goal of nursing care is achieved, with patients reaching an adaptive condition about their illness.
Ethical statementNot applicable.
Funding sourcesNone.
Authors’ contributionStudy design: IMK, RR, LA.
Data collection: RR, EM, RBS.
Data analysis: IMK, RR, EM, RBS.
Study supervision: IMK, LA.
Manuscript writing: IMK, RR, IGJ.
Critical revisions for important intellectual content: IMK, RR, LA, EM, RBS, IGJ.
Conflict of interestsWe declare that there is no conflict of interest.
None.