Supplement "Advances in Musculoskeletal Radiology"
More infoCalcific tendinopathy of the rotator cuff is a common condition caused by the deposition of calcium crystals in the tendons of the rotator cuff. This study aimed to analyze the effectiveness of ultrasound-guided puncture and aspiration in calcific tendinopathy of the should in 86 patients treated at our center and to determine the factors associated with poor prognosis after this treatment.
Material and methodsThis retrospective descriptive study included 86 patients with calcific tendinopathy of the rotator cuff treated with ultrasound-guided puncture and aspiration between 2015 and 2019 for whom clinical and radiological variables were collected 1, 3, 6, and 12 months after the procedure.
ResultsOne year after treatment, 81.4% patients showed clinical improvement and 96.5% showed radiological improvement. Complications were observed in 34.9%; all complications were mild.
ConclusionsUltrasound-guided puncture and aspiration is an effective treatment for calcific tendinopathy of the shoulder, resulting in a high rate of clinical and radiological improvement and a low rate of minor complications. This technique has additional advantages, such as interaction with the patient and the lack of ionizing radiation.
La tendinopatía calcificante del manguito rotador es una patología frecuente producida por el depósito de cristales de calcio en los tendones del manguito rotador. El objetivo de nuestro estudio reside en analizar la efectividad de la técnica PAPE en la tendinopatía calcificante del hombro en 86 pacientes tratados nuestro centro y analizar los factores de mal pronóstico tras este tratamiento.
Material y métodosSe ha realizado un estudio descriptivo retrospectivo que incluyó a 86 pacientes con TCH tratados mediante PAPE desde 2015 a 2019, de los que se recogieron variables clínicas y radiológicas a los 1, 3, 6 y 12 meses de seguimiento.
ResultadosTras un año de seguimiento se observó mejoría clínica en el 81,4% de los pacientes y mejoría radiológica en el 96,5%, con una tasa de complicaciones de un 34,9%, todas ellas de carácter leve.
ConclusionesLa PAPE es un tratamiento efectivo para la tendinopatía calcificante del hombro, con una alta tasa de mejoría clínica y radiológica, y un bajo nivel de complicaciones leves, aportando además ventajas adicionales como la interacción con el paciente y el uso de radiaciones no ionizantes.
Calcific tendinitis of the shoulder (CTS) is a pathology of unknown aetiology, characterised by the pathologic deposition of calcium hydroxyapatite crystals in one or more rotator cuff tendons. It is one of the most common causes of shoulder pain, with a prevalence of between 3% and 10% in the adult population.1
Regarding pathophysiology, Uhthoff and Loehr2 proposed that CTS progresses in three stages: precalcification, calcification and postcalcification. The calcification stage is composed of the formative phase, the resting phase and the resorptive phase.
The resorptive phase of calcific tendonitis is the most painful, which entails the patient's most functional repercussions. During this phase, calcifications tend to migrate to different locoregional structures, most commonly to intratendinous and locoregional soft tissue locations, such as the subacromial-subdeltoid bursa.3 According to Moseley,4 the different stages of calcific tendonitis of the rotator cuffs are: a) a silent phase whereby calcium deposits contained by the tendon are produced with scarcely any clinical repercussion for the patient; b) a mechanical second phase in which calcium deposits increase in size and evolve in different progressive states from an initial elevation in bursal serum to a sub-bursal rupture of calcium deposits, and finally intrabursal rupture of the same; during this phase, many inflammatory phenomena are produced which cause significant clinical repercussions and pain for the patient; c) the third phase of adhesive periarthritis in which the shoulder usually presents with painful adduction contracture and internal rotation contracture, and d) a fourth phase of intraosseous loculation of the calcium deposits.
In the majority of cases, CTS follows a relatively benign self-limited course. Thus, first-line treatment should be conservative, with significant clinical improvement achieved for 90% of patients.5 In our experience, patients who evolve favourably without treatment may take weeks to months to recover, but it is impossible to generalise, as much depends on each patient's specific conditions. If the patient does not respond adequately to medical treatment, the next therapeutic step entails minimally-invasive therapies, such as ultrasound-guided percutaneous needle aspiration (PCNA) and shock wave (SW) therapy. In cases resistant to minimally invasive treatment, surgical treatment should be considered a definitive option, with arthroscopic surgery being the approach of choice.
The objective of this study was to analyse the clinical and radiological results of the treatment of calcific tendonitis of the shoulder by means of PCNA in 86 patients and to evaluate the factors associated with poor prognosis following this treatment.
Material and methodsStudy designA retrospective descriptive study was proposed based on the review of patients diagnosed with CTS and treated at our centre with PCNA from the start of this technique in June 2015 to April 2018. The treated patients were followed up for a year with clinical interviews at radiology appointments and with radiological controls with ultrasounds and plain shoulder radiographs (AP projection) at one month, three months, six months and one year. Other post-treatment imaging tests (such as magnetic resonance imaging) were not required due to the absence of serious complications that would make it necessary to carry out a more complex study than ultrasound or plain radiography.
Study population- 1
Inclusion criteria:
- •
Patients diagnosed with symptomatic CTS who agreed to the procedure after verbal and written consent.
- •
Calcium deposits greater than 5mm visible on plain radiography and ultrasound.
- •
Patients who adequately completed follow-up up to one year.
- •
The patients included in our study attended, in the first instance, an appointment with their traumatologist or rehabilitation specialist who initiated conservative medical treatment. If the patient did not respond adequately and the pain persisted for months with no response to drugs or rehabilitation, based on the clinical judgement of the responsible physician, it was decided to opt for PCNA or SW therapy.
- •
- 2
Exclusion criteria:
- •
Presence of another obvious cause of the pain and/or functional disability of the affected shoulder in locations other than the pathology of the rotator cuff itself (degenerative changes in acromioclavicular joint, adhesive capsulitis, etc.).
- •
Presence of contraindications: infection, coagulation disorder, allergy to medication used, pregnancy, etc.
- •
Lack of follow-up or lack of information about the patient or any of the planned controls.
- •
The technique was performed by two radiologists from the musculoskeletal unit with more than 10 years of experience, who implemented this technique in our centre in 2015, following the guidelines and recommendations of other authors listed in the existing bibliography. The collection of data and the drafting of the work was conducted by radiology residents and final year medicine students.
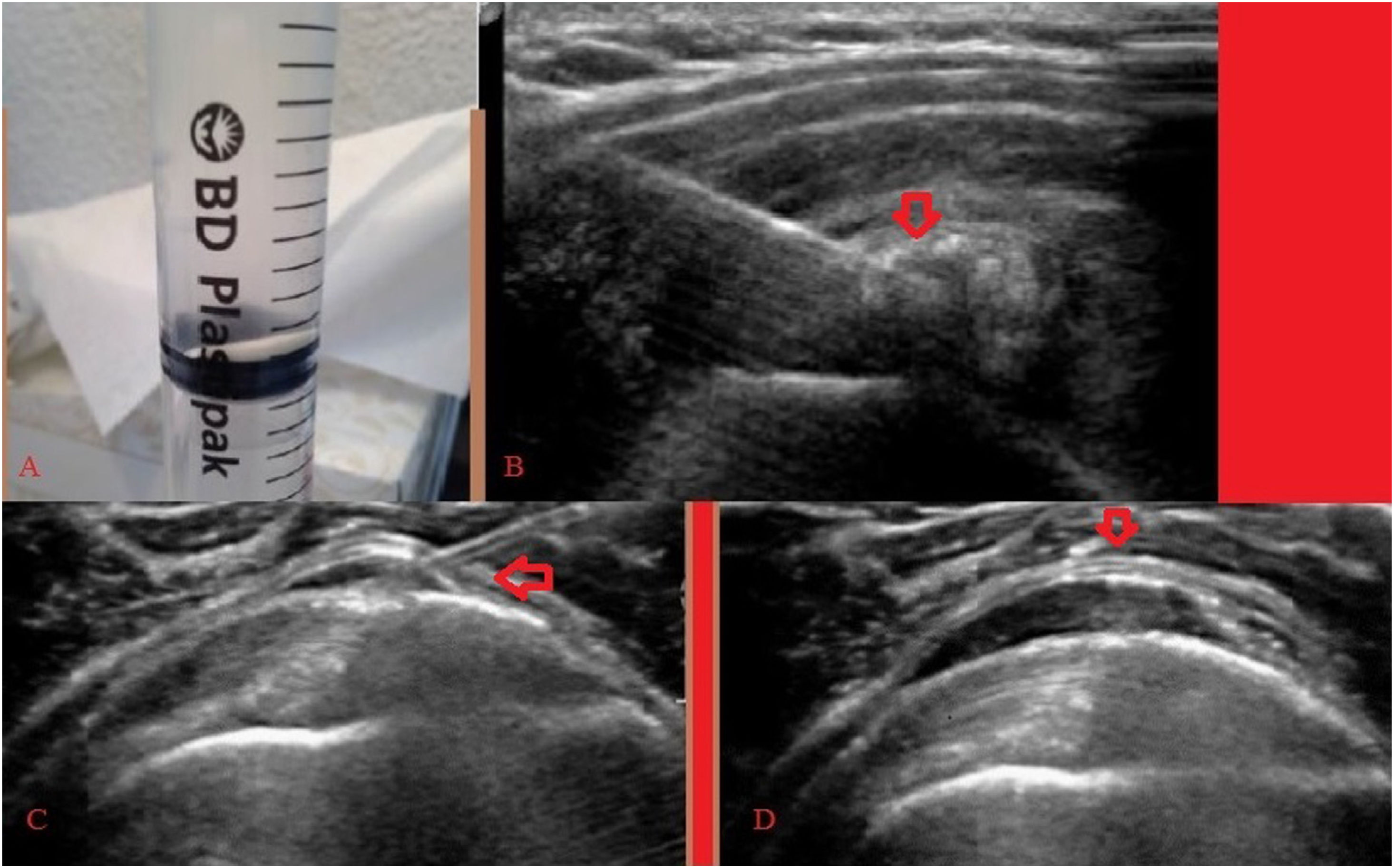
Description of the technique (Fig. 1)The specific material used to carry out this technique consists of: Fig. 1
- •
Canon-Toshiba Aplio a550 ultrasound machine, 10MHz high frequency probe.
- •
21G intramuscular needle without introducer.
- •
10ml LuerLock cone syringes.
- •
10ml mepivacaine injectable ampoule.
- •
40mg/ml triamcinolone acetonide ampoule.
Firstly, with the patient seated in a semi-sitting position on a stretcher, a general ultrasound examination was performed, and once the puncture site had been decided on, 10ml of 1% mepivacaine was administered into the puncture tract, followed by the introduction of an intramuscular needle up to the calcification with ultrasound control. The calcification was perforated and lavage of the calcifications was conducted using small percussions with the plunger as many times as necessary until the entry and exit of clear physiological saline was verified or until cavity formation and complete rupture of calcification was confirmed.
Finally, a corticosteroid was injected into the subacromial-subdeltoid bursa (in our case we always inject 40mg of undiluted triamcinolone, equivalent to one ampoule).
Following the completion of the procedure, the first radiological control of the calcifications was carried out a month after the PCNA. Relative rest without overloading the limb, and local control measures, such as the application of ice in the event of inflammation or pain, were prescribed.
In patients with subacromial-subdeltoid bursitis, when starting treatment, a PCNA technique can be performed if there is identifiable calcification, or an aspiration attempt can be performed if only fragments are observed in the bursa.
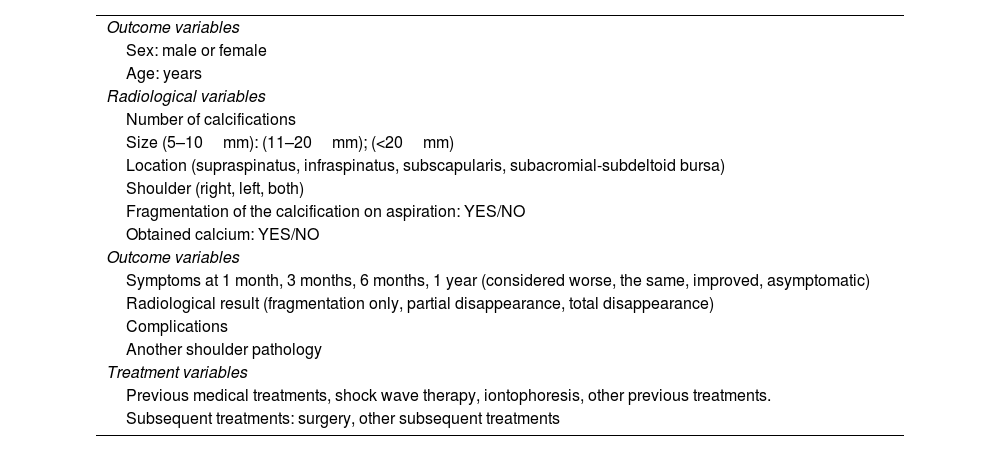
Variables studiedDemographic, radiological, outcome and treatment variables were collected, and these are summarised in Table 1.
Epidemiological and radiological variables, outcome variables and treatment used in our study.
| Outcome variables |
| Sex: male or female |
| Age: years |
| Radiological variables |
| Number of calcifications |
| Size (5–10mm): (11–20mm); (<20mm) |
| Location (supraspinatus, infraspinatus, subscapularis, subacromial-subdeltoid bursa) |
| Shoulder (right, left, both) |
| Fragmentation of the calcification on aspiration: YES/NO |
| Obtained calcium: YES/NO |
| Outcome variables |
| Symptoms at 1 month, 3 months, 6 months, 1 year (considered worse, the same, improved, asymptomatic) |
| Radiological result (fragmentation only, partial disappearance, total disappearance) |
| Complications |
| Another shoulder pathology |
| Treatment variables |
| Previous medical treatments, shock wave therapy, iontophoresis, other previous treatments. |
| Subsequent treatments: surgery, other subsequent treatments |
The patient's subjective sensation regarding pain and functional disability, categorised as “worse”, “the same”, “improved” and “asymptomatic”, was recorded at one month, three months, six months and 12 months or more (patients who needed more than one aspiration).
The data was analysed using the SPSS statistical package (IBM Corp. Released 2017. IBM SPSS Statistics for Windows Version 25.0). Quantitative variables are presented with the mean and standard deviation, and qualitative variables according to their frequency distribution. Pearson’s χ2 test was used to analyse the association between the qualitative variables. Lastly, a multivariate logistic regression study was performed, with the dependent variable being the clinical results (improvement, no improvement). Values p<0.05 were considered to be statistically significant.
ResultsDescriptive statisticsDemographic variables106 patients were selected, of whom 20 were excluded because they had a shoulder pathology other than that of the rotator cuff (13 patients), allergies to the medication used (two patients) and resolution of symptoms at the time of arrival at our clinic (five patients). Therefore, 86 patients were included in the study, 59 of them women (68.6%) and 27 men (31.4%), with an age range between 28 and 76 years and a mean age of 52.3 years (SD 10.1). Of these 86 patients, 15 had pathology in both rotator cuffs, 50 patients had unilateral involvement of the right shoulder and 21 patients had unilateral involvement of the left shoulder.
A total of 101 shoulders were treated with 155 aspiration and lavage procedures.
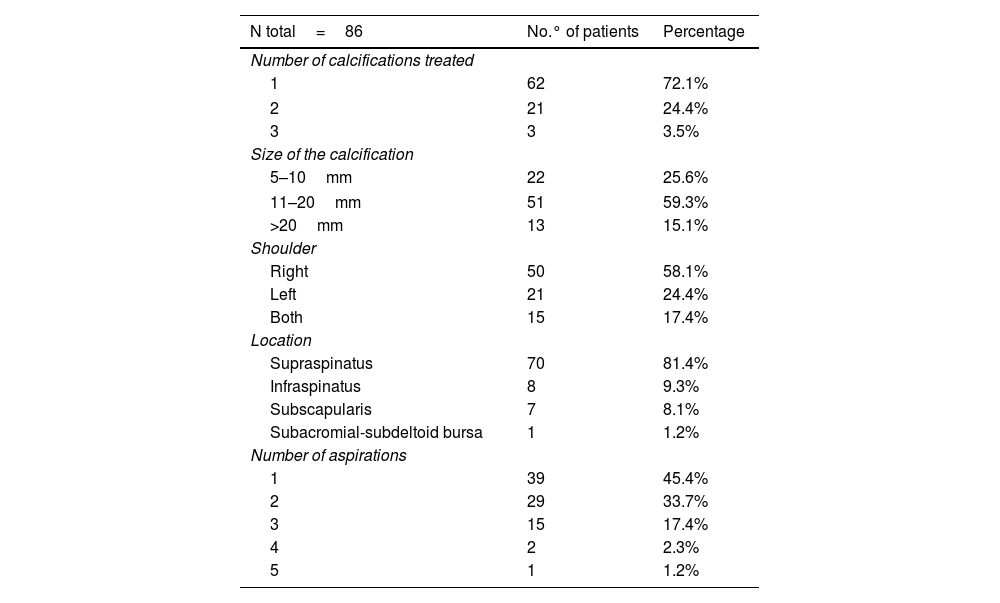
Variables in relation to the pathologyVariables collected at the time of treatment (Table 2).
Descriptive variables of treated calcifications.
| N total=86 | No.° of patients | Percentage |
|---|---|---|
| Number of calcifications treated | ||
| 1 | 62 | 72.1% |
| 2 | 21 | 24.4% |
| 3 | 3 | 3.5% |
| Size of the calcification | ||
| 5–10mm | 22 | 25.6% |
| 11–20mm | 51 | 59.3% |
| >20mm | 13 | 15.1% |
| Shoulder | ||
| Right | 50 | 58.1% |
| Left | 21 | 24.4% |
| Both | 15 | 17.4% |
| Location | ||
| Supraspinatus | 70 | 81.4% |
| Infraspinatus | 8 | 9.3% |
| Subscapularis | 7 | 8.1% |
| Subacromial-subdeltoid bursa | 1 | 1.2% |
| Number of aspirations | ||
| 1 | 39 | 45.4% |
| 2 | 29 | 33.7% |
| 3 | 15 | 17.4% |
| 4 | 2 | 2.3% |
| 5 | 1 | 1.2% |
Regarding the response to treatment categories “improved” and “asymptomatic” reported by the patients, the effectiveness of the treatment can be considered to be 80.2% at a month, 55.8% at three months, 67.4% at six months and 81.4% at a year.
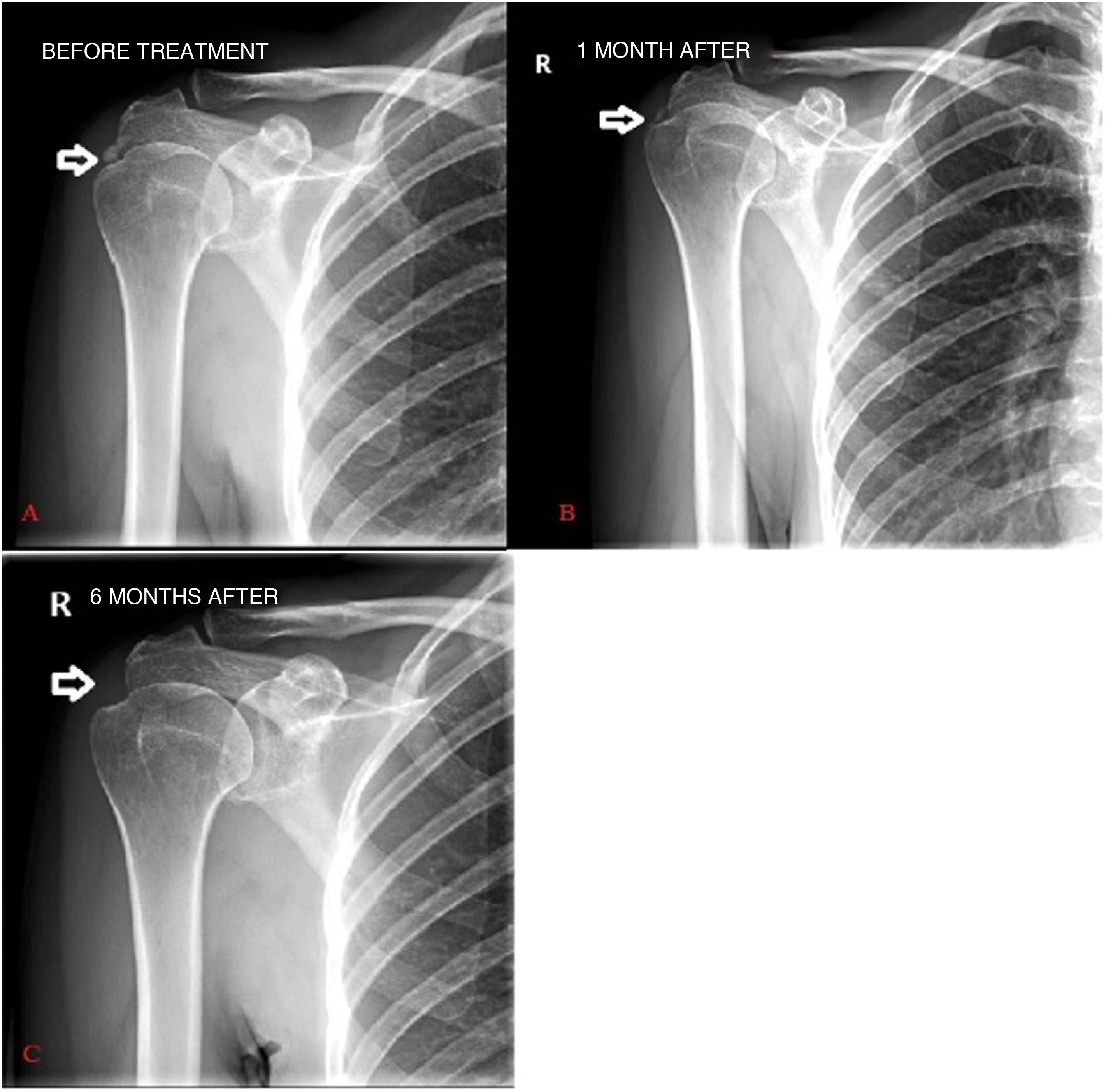
Radiological resultsAfter one year of follow-up, 34.88% of the patients presented with the total disappearance of the calcification, 61.63% with a partial disappearance (minimal remains on radiology or ultrasound), while only 3.49% experienced no change or only fragmentation without a decrease in the overall size of the calcification (Fig. 2).
Considering the results based on the total number of calcifications treated, 75% of patients who responded to treatment had a single treated calcification, while only 24% of patients with two or more treated calcifications responded adequately to treatment.
Other treatmentsAll patients received symptomatic medical treatment for pain before conducting the PCNA. In addition to this treatment, 5.8% of patients were treated beforehand with shock wave therapy, 3.5% with iontophoresis, and 30.2% received another type of rehabilitation treatment, with up to 3.5% having received more than one of these previous treatments. PCNA was the first treatment other than medical in 64% of cases.
ComplicationsThe most frequent complication was bursitis, described as increased bursal wall thickening on ultrasound, with a higher incidence in those patients who needed to undergo aspiration again. De Conti et al.6 postulated that bursitis is caused by the migration of microcrystals from calcium deposits into the bursa. The development of complications was not related to a worse clinical outcome at the end of the follow-up.
The classification of bursitis as mild, moderate and calcific bursitis was conducted according to subjective visual judgement. In the event that a patient presents with calcific bursitis as a complication following PCNA, treatment and follow-up is carried out directly in our radiology department without the need for the patient to see other professionals.
Of the patients treated, 34.9% presented with mild complications, such as mild subacromial-subdeltoid bursitis (26.7%), moderate bursitis (4.7%), calcific bursitis (1.2%) and vasovagal reflex (1.2%).
Inferential statisticsRelationship between clinical and radiological resultsThere were no statistically significant differences (p=0.5) when comparing clinical results with radiological results at the end of the follow-up in the responder versus the non-responder group.
Relationship between clinical results and another shoulder pathologyAmong non-responders (19.6%), the majority had another shoulder pathology (83%), while responders (81.4%) presented with another pathology at a smaller percentage (58.5%), correlating significantly (p<0.05). According to the exclusion criteria, all those patients who presented with another obvious cause of the pain and/or functional disability of the shoulder in locations other than the pathology of the rotator cuff itself were eliminated. However, all patients had a greater or lesser degree of tendinitis. If the clinical picture did not improve when the calcium deposits disappeared, we reasoned that the tendinitis could be the main cause of the patient’s pain.
DiscussionThis study demonstrates that PCNA is an effective and safe treatment to achieve clinical and radiological improvement in patients with CTS. After follow-up for a year or more of 86 patients treated with PCNA, clinical improvement was observed in 81.4% of patients, with the partial or total disappearance of calcifications in 96.5%.
Current evidence on treatments for CTS remains low. Different meta-analyses have demonstrated that, within the minimally invasive treatments, both PCNA4 and SW therapy is effective and safe compared to placebo, with PCNA considered to be the most effective treatment to improve symptoms and reduce the size of the calcification.7–9 SW therapy requires multiple treatment sessions, so it can take longer and is less cost-effective.10,11
PCNA clinical efficacy results vary depending on the study, from 65% to 92%.1,12 This could be explained by study heterogeneity, with different sample sizes and the use of different validated scales, such as the Constant Score, the Shoulder Pain and Disability Index (SPADI), the L’Insalata Shoulder Questionnaire, the Numerical Rating Scale (NRS) for pain or the Visual Analogue Scale (VAS). At the same time, other authors express the results with a verbal description of the symptoms without using scales, as was our case. Our result falls within this range of efficacy, so it is consistent with previous evidence.
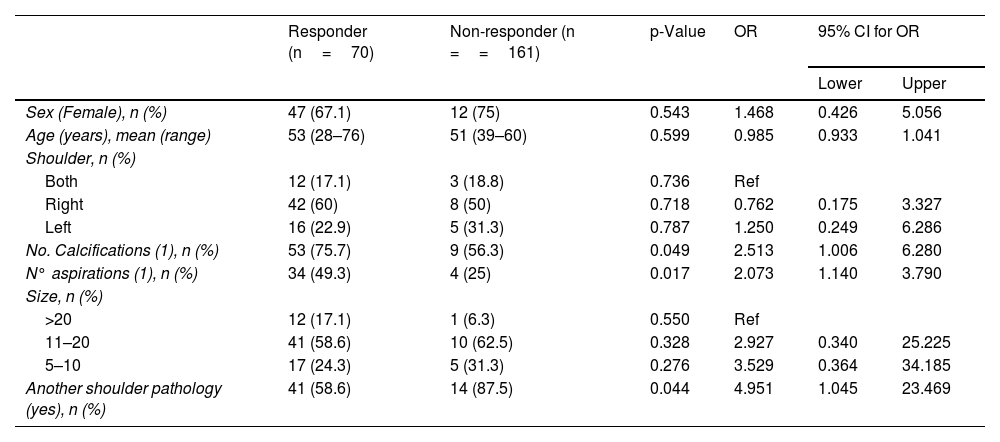
According to the literature consulted, PCNA is the treatment that has been shown to be most effective in reducing the size and subsequent disappearance of calcifications in calcific tendinitis of the shoulder.5,7–9 In our study, a partial or total disappearance was observed in 96.5% of cases, in accordance with the evidence. However, when comparing the epidemiological and pathological variables with the clinical response at one year of follow-up, in the face of a greater number of calcifications, a worse response to treatment was observed, and a greater number of aspirations were required, obtaining a significant value (p<0.05) (Table 3).
Multivariate analysis of variables associated with clinical response. Only includes one treated calcification, one aspiration in relation to statistically significant results (p<0.05).
| Responder (n=70) | Non-responder (n ==161) | p-Value | OR | 95% CI for OR | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Sex (Female), n (%) | 47 (67.1) | 12 (75) | 0.543 | 1.468 | 0.426 | 5.056 |
| Age (years), mean (range) | 53 (28–76) | 51 (39–60) | 0.599 | 0.985 | 0.933 | 1.041 |
| Shoulder, n (%) | ||||||
| Both | 12 (17.1) | 3 (18.8) | 0.736 | Ref | ||
| Right | 42 (60) | 8 (50) | 0.718 | 0.762 | 0.175 | 3.327 |
| Left | 16 (22.9) | 5 (31.3) | 0.787 | 1.250 | 0.249 | 6.286 |
| No. Calcifications (1), n (%) | 53 (75.7) | 9 (56.3) | 0.049 | 2.513 | 1.006 | 6.280 |
| N° aspirations (1), n (%) | 34 (49.3) | 4 (25) | 0.017 | 2.073 | 1.140 | 3.790 |
| Size, n (%) | ||||||
| >20 | 12 (17.1) | 1 (6.3) | 0.550 | Ref | ||
| 11–20 | 41 (58.6) | 10 (62.5) | 0.328 | 2.927 | 0.340 | 25.225 |
| 5–10 | 17 (24.3) | 5 (31.3) | 0.276 | 3.529 | 0.364 | 34.185 |
| Another shoulder pathology (yes), n (%) | 41 (58.6) | 14 (87.5) | 0.044 | 4.951 | 1.045 | 23.469 |
CI: confidence interval; OR: odds ratio.
No significant association was found between clinical and radiological outcomes; i.e., a radiological improvement has not been shown to translate into a clinical improvement, as some authors had previously described.13
The efficacy of a treatment can also be measured by the need for subsequent treatments. In our study, following treatment with PCNA and after completion of follow-up, 11.6% received SW therapy, while 4.7% required surgery. In addition, 22.1% were referred to rehabilitation. Most of the patients who required further treatment had not responded to PCNA treatment or had not achieved complete clinical resolution. All the patients who underwent surgery had another shoulder pathology that required surgical treatment, such as labral injury (three cases) or atraumatic shoulder instability (one case). Different authors recommend surgery for those patients who do not respond to previous lines of treatment, since it has been shown to be an effective treatment. Currently, surgery is the last line of treatment because it is an invasive therapy that involves a higher cost, greater risks and a slower recovery.14
In our study, a more significant clinical improvement was observed at one month (80.2%) than at three months (55.8%). This could be explained by the persistence of the analgesic effect of the corticosteroids injected into the subacromial bursa after the aspiration.
Considering these results, we recommend not delaying the start of therapy with PCNA in those patients who meet the criteria for it to be carried out and who have not responded to initial medical or rehabilitative treatment. PCNA can safely and effectively shorten the duration of symptoms and the time it takes for calcification to disappear. On the other hand, we recommend that the first follow-up visit be carried out at two months (instead of at a month) after aspiration and injection of corticosteroids into the bursa, so that the anti-inflammatory effect of the corticosteroids does not mask symptoms.
A recent meta-analysis on the results and complications of PCNA describes a rate of complications of 7%, with all complications being minor.14,15 In our study, the rate of complications observed was 34.9%, with bursitis being the most frequent. The difference in the rate of complications compared to the previous meta-analysis could be explained by the lack of description of bursitis as a complication secondary to treatment in most of the included studies and by the limit considered by the authors to define bursitis. With these results we can determine that PCNA is a safe treatment.
This study is the first of its kind to explore the presence of another shoulder pathology as a factor related to the clinical outcome after treatment with PCNA in CTS. Any change observed on imaging tests other than the inflammation of the tendon in which the calcification and degenerative changes of the acromioclavicular joint in very early stages were located was described as another shoulder pathology. The presence of another shoulder pathology is a poor prognostic factor for achieving clinical improvement in patients with CTS (p<0.05).
We must take into account certain limitations regarding the interpretation of our results. First, as in all retrospective studies, our data are partially influenced by their proper collection. In addition, biased selection is possible in some cases, since only patients who met the study criteria and had completed follow-up were selected. Secondly, the small sample size and the lack of use of standardised clinical and functional assessment scales, such as the VAS scale, could limit the results. Thirdly, since the results were not compared with an untreated control group, we cannot study the actual efficacy of treatment versus conservative treatment. Lastly, it is difficult to establish criteria for selecting the cases in which the presence of another shoulder pathology is considered and to determine if this pathology is truly responsible for the persistence of symptoms. We suggest conducting new long-term follow-up studies taking into account the presence of another shoulder pathology to determine better evidence of its association with a worse outcome. We propose that future studies use validated scales to study clinical improvement. Conducting clinical trials to compare the different treatments (conservative, PCNA and SW therapy) in the long term is necessary to obtain a higher level of evidence.
Taking into account the existing literature and the results obtained in our study, we can consider this technique to be one of the fundamental pillars of the non-invasive treatment of calcific tendinitis of the shoulder whilst being mindful that more studies with a larger sample size, with clinical assessment scales and with a group of untreated controls will be necessary to obtain further information on the effectiveness of this technique.
ConclusionsPCNA is an effective and safe treatment in CTS, since it produces significant clinical and radiological improvement in treated patients and also offers additional advantages such as interaction with the patient and use of non-ionising radiation.
The presence of another shoulder pathology, as well as a greater number of calcifications and the need for a greater number of aspirations, seem to be negative prognostic factors.
Authorship- 1
Responsible for the integrity of the study: ISL, BTC.
- 2
Study concept: SOA. CRB, ISL, BTC, NAG.
- 3
Study design: SOA. CRB, ISL, BTC, NAG.
- 4
Data collection: SOA, CRB.
- 5
Data analysis and interpretation: SOA, CRB, ISL, BTC, NAG
- 6
Statistical processing: CRB, SOA
- 7
Literature search: CRB
- 8
Drafting of the article: SOA. CRB, ISL, BTC, NAG.
- 9
Critical review of the manuscript with intellectually significant contributions: SOA. CRB, ISL, BTC, NAG.
- 10
Approval of the final version: SOA. CRB, ISL, BTC, NAG.
The authors declare that they have no conflicts of interest.