Supplement "Advances in Musculoskeletal Radiology"
More infoIntraneural ganglion cysts are very uncommon lesions, whose diagnosis has increased since the articular theory and the description of the MRI findings were established. We present a case report of a 59-year-old man with symptoms of tarsal tunnel syndrome. Foot and ankle MRI demonstrated the presence of an intraneural cystic lesion in the posterior tibial neve and its connection with the subtalar joint through an articular branch. The identification of the specific radiological signs like the «signet ring sign» allowed establishing an adequate preoperative diagnosis, differentiating it from an extraneural lesion and facilitating the articular disconnection of the nerve branch during surgery.
Los gangliones intraneurales son lesiones muy infrecuentes, que han empezado a ser diagnosticadas gracias al establecimiento de la teoría articular para explicar su patogénesis y la definición de los signos radiológicos en la resonancia magnética (RM). Presentamos el caso de un varón de 59 años con clínica indicativa de síndrome del túnel del tarso. El estudio de RM de tobillo y pie demostró la presencia de un ganglión intraneural dependiente del nervio tibial posterior y su conexión con la articulación subastragalina a través de una rama nerviosa articular. La adecuada interpretación de signos radiológicos específicos como el «signo del anillo de sello» permitieron establecer un adecuado diagnóstico preoperatorio, diferenciándolo de una lesión extraneural y facilitando la desconexión articular de la rama nerviosa durante la cirugía.
Ganglion cysts are most commonly located in the periarticular region and present as palpable, firm masses that can be either painful or painless. They are diagnosed by ultrasound.1
Intraneural ganglion cysts are much rarer and are secondary to traumatic or degenerative joint damage. An intraneural lesion arises from the articular branch of a peripheral nerve that connects to the joint capsule. Following joint damage, joint fluid spreads along the epineurium of the articular nerve branch reaching the main nerve and some of its branches.2
Most originate in the superior tibiofibular joint and involve the common peroneal nerve. There are few reported cases of intraneural ganglion cysts in the tarsal tunnel that involve the tibial nerve and its branches.3
These lesions are now recognised thanks to the unifying articular theory. Spinner et al.4 state that intraneural lesions arise from the articular branch of a peripheral nerve, which connects the peripheral nerve to the joint capsule. Following damage to the joint capsule, joint fluid spreads along the epineurium of the joint nerve branch to reach the main nerve and its branches.
Radiological diagnosis of these lesions is difficult; the relationship between the lesions and surrounding nerve structures must be identified. Knowing the pathogenesis and a familiarity with radiological signs on magnetic resonance imaging (MRI) helps to differentiate them from extraneural ganglion cysts, which are much more common and whose radiological findings are widely known.
Case studyA 59-year-old male patient with pain in the right foot for five months and paraesthesia on the bottom of his first three toes.
On examination, the patient complained of neuropathic pain in the right ankle, an antalgic gait, tactile hypoaesthesia in the territory of the medial plantar nerve (first and second toes and medial aspect of the third toe), and no motor impairment. Tinel's test for tarsal tunnel syndrome was positive.
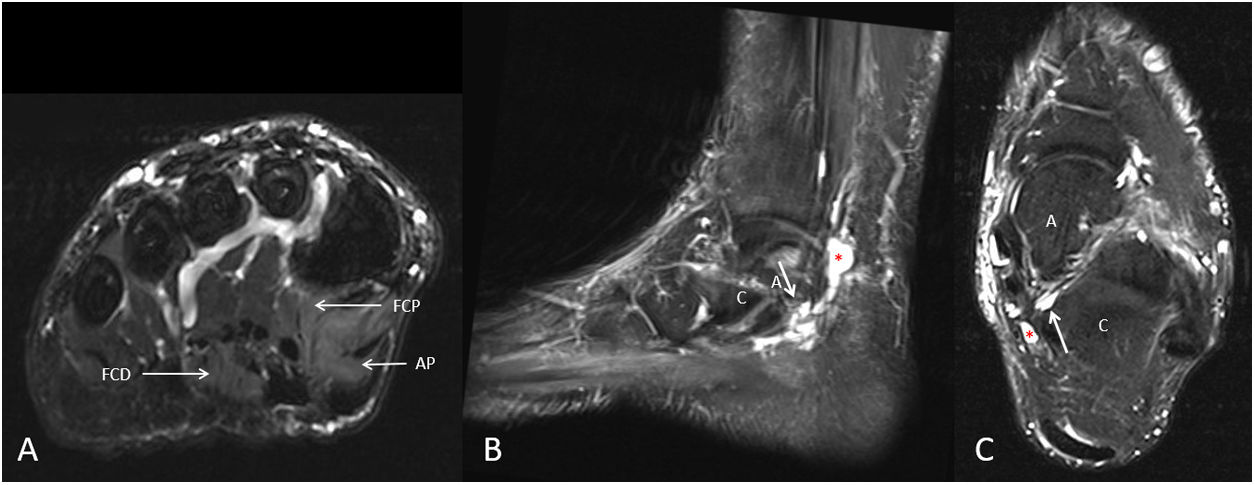
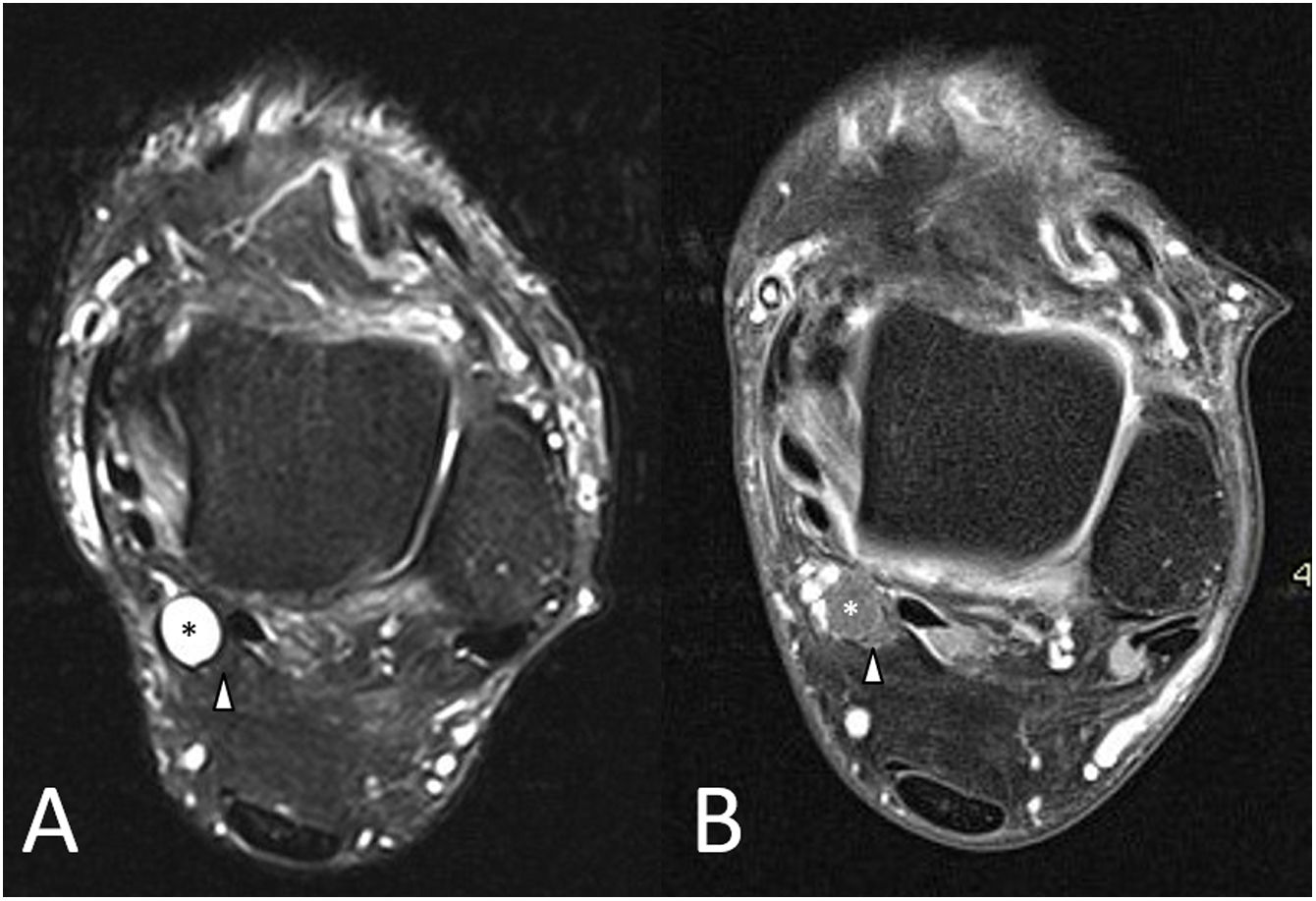
Given the clinical suspicion of tarsal tunnel neuropathy, an MRI of the foot and ankle was performed which revealed signs of acute denervation in the foot musculature, innervated by the medial plantar nerve (Fig. 1A). The ankle study revealed a polylobulated cystic lesion at the level of the tarsal tunnel, following the course of the posterior tibial nerve and the medial plantar nerve (Fig. 1B). MRI identified the ‘tail sign’, demonstrating the origin of the lesion in the subtalar joint (Fig. 1B and C) and the ‘signet ring sign’ in the proximal portion of the lesion (Fig. 2), confirming the intraneural location. The diagnostic study was completed with an electromyogram, which showed demyelination and moderate axonal loss in the tibial nerve (mainly in the medial plantar nerve) in the tarsal tunnel, with signs of denervation in the abductor muscle of the first toe.
‘Tail sign’. T2-weighted MRI images with fat saturation showing oedema in the musculature innervated by the medial plantar nerve (A; coronal image of foot). Sagittal and axial MRI images of the ankle (B and C) show a tubular cystic lesion (red asterisk), extending proximally from the distal portion of the posterior tibial nerve and distally to the medial plantar nerve. A pedicle connecting the lesion to the subtalar joint is also visible (white arrow in B and C).
A: talus; C: calcaneus; AP: abductor hallucis; FCD: flexor digitorum brevis; FCP: flexor hallucis brevis.
‘Signet ring sign’. Axial T2-weighted MRI images of the ankle at the level of the posterior tibial nerve with fat saturation (A) and T1-weighted images with fat saturation after administration of intravenous contrast (B). They show the lateral displacement of the nerve fascicles (arrowheads), which take on a crescent morphology, and the absence of a fatty plane interposed between the nerve and the lesion (asterisks in A and B). White arrowhead: posterior tibial nerve.
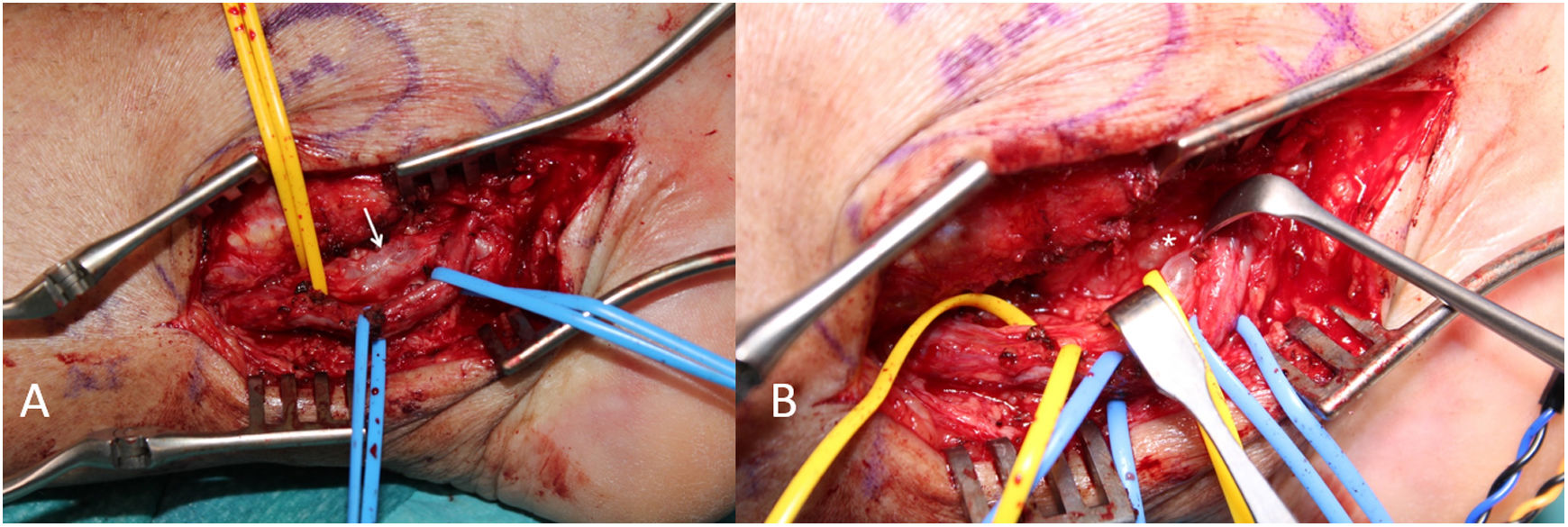
Excision was performed on the basis of the diagnosis, intraneural ganglion cyst in the tarsal tunnel with neuropathy affecting the posterior tibial nerve and its branches. Intraoperative findings confirmed an intraneural cystic lesion in the tarsal tunnel (Fig. 3A), and the articular connection of the cyst from the medial plantar nerve to the subtalar joint (Fig. 3B).
Intraoperative images of the surgical technique. (A) The tibial nerve (yellow marker) and the posterior tibial vascular bundle (blue marker) after releasing the tarsal tunnel. The cystic formation on the tibial nerve is evident (white arrow). (B) The articular connection of the cyst to the subtalar joint (asterisk) was identified by removing the nerve.
After surgery, the patient showed immediate improvement both in terms of pain and hypoaesthesia, with complete recovery after two months.
DiscussionIntraneural ganglion cysts are rare lesions, especially in the ankle and foot region. In the latest systematic review conducted in 2016, of the 648 cystic lesions included, almost 400 (60%) were dependent on the common peroneal nerve or its deep and superficial branches, 20 (3.1%) on the tibial nerve, and only 2 (0.3%) were located in the distal third of the tibial nerve and medial plantar nerve.2
In our case, the lesion originated in the subtalar joint, with involvement of the tibial nerve and medial plantar nerve. In the literature, only two cases have been reported with involvement of these two nerves,5 causing us to suspect that the disease is underdiagnosed.
There are several radiological signs on MRI that enable a diagnosis of intraneural ganglion cysts.6 The first, the ‘tail sign’, consists of identifying the connection of the lesion to the subtalar joint. This sign demonstrates the articular origin of the lesion, but in most cases it does not distinguish between intraneural and extraneural lesions.
The other identifiable sign, much more specific for demonstrating their intraneural location, is the ‘signet ring sign’.5,6 In our case, this sign can be identified in the proximal portion of the lesion, where the lesion can be seen to occupy the epineurium of the posterior tibial nerve, laterally displacing the nerve fascicles and interposed fat, resulting in an image with a crescent morphology adjacent to the lesion, reminiscent of this figure. In other cases, there may be no fatty plane separating the nerve fascicles from the lesion. This sign can be identified on axial sequences, and is more likely to be identified on fluid-sensitive sequences, and after contrast administration.
In extraneural lesions, the crescent shape is not usually present, and the fatty plane between the nerve fascicles and the lesion is preserved.
Thin-slice MRI can help identify the joint nerve branch. T2-weighted sequences with fat saturation are essential to recognise the lesion and establish its morphology, extent and relationship to the nerve branches and the joint.6 In addition, pre- and post-contrast T1-weighted sequences can discriminate between intra- and extraneural cystic lesions.
Ganglion cysts in the tarsal tunnel can also be diagnosed by ultrasound, the technique of choice for accessible regions due to its equivalent specificity and greater sensitivity compared with MRI for the detection of peripheral nerve lesions.7 However, it is harder to demonstrate the relationship intraneural lesions have with the articular nerve branch.
There are several therapeutic options for this type of lesions, some of which are minimally invasive, such as ultrasound-guided puncture-drainage with or without corticosteroid injection into the nerve sheath,8 and other invasive options such as surgical excision. Both options have a high recurrence rate because success depends on disconnecting the articular nerve branch or carrying out joint debridement at the point where it originates.9
For this reason, a familiarity with the radiological characteristics of these lesions is essential in order to correctly diagnose them and carry out adequate pre-surgical planning to resolve the condition and avoid recurrences.
Author contributionsJuan José Jover-Sánchez has participated in developing the study concept and design, gathering data and interpreting the results of the complementary tests. He was involved in the drafting of the article and the critical review of the radiological content. He was also involved in approving the final version of the article.
Lara Cristóbal-Velasco oversaw the drafting of the article and critically reviewed the surgical content. She was involved in approving the final version of the article.
Ester Benza-Villarejo oversaw the drafting of the article and carried out the critical review of the radiological content. She was involved in approving the final version of the article.
Andrés A. Maldonado-Morillo was involved in developing the study concept and design, gathering data and interpreting the results of the complementary tests. He was involved in the drafting of the article and the critical review of the surgical content. He was also involved in approving the final version of the article.
FundingThis research has not received funding support from public sector agencies, the business sector or any non-profit organisations.
Conflicts of interestNone.