Caregivers of people with autism spectrum disorder (ASD) are chronically exposed to high levels of stress. In turn, such stress is associated with high rates of negative health outcomes. However, few studies have analyzed the effects of psychotherapeutic interventions in improving health in this population. The main aim of the present study was to evaluate the effectiveness of a cognitive-behavioral intervention program, based on the model proposed by Ruiz-Robledillo and Moya-Albiol (2014a). For this, we used a sample of 17 informal caregivers of people diagnosed with ASD. The study was based on a pre-post design. Caregivers had lower levels of burden immediately after the intervention than at baseline, while both immediately after the intervention and at 1 month of follow-up, they had fewer somatic symptoms, lower levels of depression, and better mood states than at baseline. These results provide evidence of the efficacy of the cognitive-behavioral intervention developed for reducing stress and health complaints in chronically stressed caregivers. Additionally, the program could be useful in early stages of the caring process, to provide caregivers with effective skills for preventing future health problems. The integration of the program in general psychosocial interventions would be highly beneficial for this population.
Los cuidadores de personas con trastorno del espectro autista (TEA) están crónicamente expuestos a altos niveles de estrés. Este hecho está asociado al padecimiento de numerosos problemas de salud. Sin embargo, pocos estudios han analizado los efectos de intervenciones psicoterapéuticas en la mejora de su salud. El objetivo del presente estudio fue evaluar la eficacia de un programa de intervención cognitivo-conductual, basado en el modelo propuesto por Ruiz-Robledillo y Moya-Albiol (2014a). Para ello, se utilizó una muestra de 17 cuidadores informales de personas con TEA. El estudio se basó en un diseño pre-post. Los cuidadores presentaron menores niveles de sobrecarga después de la intervención en comparación con la línea base. Después, y tras un mes de la finalización de la intervención, presentaron menores síntomas somáticos, depresión y un mejor estado de ánimo que en la línea base. Estos resultados refuerzan la eficacia de la intervención cognitivo-conductual implementada en la reducción del estrés y los problemas de salud en cuidadores crónicamente estresados. El programa podría ser útil en las primeras etapas del proceso de cuidado, proporcionando a los cuidadores habilidades efectivas para la prevención de futuros problemas de salud. La integración del programa en intervenciones psicosociales generales sería altamente beneficioso para esta población.
The prevalence of autism spectrum disorder (ASD), characterized by difficulties in socialization, communication, and repetitive and restricted interests and behavior (American Psychiatric Association, 2013), has increased dramatically in recent years (Elsabbagh et al., 2012). Given the nature of the disorder and its chronic nature, individuals with ASD need long-term caregivers. Due to the early symptoms manifestation in ASD, caregivers are usually close family members, more specifically, their parents (Karst & Van Hecke, 2012; Lovell, Moss, & Wetherell, 2012a; Ruiz-Robledillo et al., 2012; Ruiz-Robledillo & Moya-Albiol, 2012; Seguí, Ortiz-Tallo, & De Diego, 2008). This is an important social issue, as family caregivers often face a range of psychosocial problems including legal hurdles, and financial and work-related complications, as well as challenges associated with the care process itself (Lavelle et al., 2014; Ruiz-Robledillo et al., 2012; Seguí et al., 2008). All of these problems may arise in the case of informal caregivers of people with ASD. While coping with these problems, caregivers are under high levels of chronic stress, with negative consequences not only for their quality of life but also for their health. In line with this, they have been found to have more somatic symptoms, higher levels of anxiety and depression, and poorer perceived general health than the general population (Andrés-García, Moya-Albiol, & González-Bono, 2012; Johnson, Frenn, Feetham, & Simpson, 2011; Khanna et al., 2011; Lovell, Moss, & Wetherell, 2012a; Ruiz-Robledillo, González-Bono, & Moya-Albiol, 2014; Ruiz-Robledillo & Moya-Albiol, 2013; Ruiz-Robledillo & Moya-Albiol, 2014a). On the other hand, several psychosocial and psychological factors have been demonstrated to ameliorate these negative health consequences (Ruiz-Robledillo & Moya-Albiol, 2014a). Indeed, caregivers with high levels of social support, adaptive coping skills, a high emotional regulation capacity, and resilience have fewer health complaints (Bekhet, Johnson, & Zauszniewski, 2012; Boyd, 2002; Lai & Oei, 2014; Lovell, Moss, & Wetherell, 2012b; Ruiz-Robledillo, De Andrés-García, Pérez-Blasco, González-Bono, & Moya-Albiol, 2014; Ruiz-Robledillo & Moya-Albiol, 2013; Ruiz-Robledillo & Moya-Albiol, 2014b).
Although the negative consequences of caring for people with a diagnosis of ASD have been widely analyzed, few studies have evaluated the effectiveness of psychotherapeutic interventions for reducing health complaints and stress levels in this population. The high effectiveness of several intervention approaches in reducing health complaints and stress perception in different samples of informal caregivers has been shown (López & Crespo, 2007; Sorrell, 2014; Mierlo, Meiland, Van der Roest, & Dröes, 2012). Indeed, problem-solving therapy, psychoeducation, counseling, peer support interventions, and respite programs have been effective reducing stress perception and its negative effects, as well as significantly improving quality of life and well-being (Cheon, Chang, Kong, & Song, 2011; Martín-Carrasco et al., 2009; Rivera, Elliott, Berry, & Grant, 2008; Shilling et al., 2013; Sorensen, Waldorff, & Waldemar, 2008). However, the majority of studies analyzed samples of caregivers taking care of dementia or cancer patients or stroke survivors, whereas the effectiveness in samples of ASD patients’ caregivers has been little studied. In this sense, most studies conducted in these informal caregivers analyzed the effects on the caregiver status of interventions focused on the management of behavioral problems and autistic symptoms in the care recipient, with positive outcomes (Drew et al., 2002; Salt, Shemit, Sellars, Boyd, & Coulson, 2002; Smith, Groen, & Wynn, 2000; Tonge et al., 2006). Other studies have evaluated the effectiveness of multi-component treatments, namely, interventions oriented to the treatment of symptoms of both care recipients and caregivers. This type of intervention has shown high effectiveness lessening perceived stress and improving health status in caregivers of people with developmental disabilities compared to interventions focusing only on care recipients (Singer, Ethridge, & Aldana, 2007). Other treatment strategies, such as mutual help groups (Huws, Jones, & Ingledew, 2001), and more recent interventions, such as mindfulness-based approaches, have also been reported to be effective improving the quality of life in informal ASD patients caregivers (Dykens, Fisher, Taylor, Lambert, & Miodrag, 2014; Ruiz-Robledillo, Sariñana-González, Pérez-Blasco, González-Bono, & Moya-Albiol, in press). However, little research has been carried out for specific psychotherapeutic interventions aiming to teach cognitive and behavioral stress management strategies to ASD patient caregivers. In this regard, the effectiveness of cognitive-behavioral therapy (CBT) in this population is poorly studied. Recent revisions of several meta-analysis pointed out the high efficacy of this type of intervention in different problems (Butler, Chapman, Forman, & Beck, 2006; Hoffman, Asnaani, Vonk, Sawyer, & Fang, 2012). CBT is effective for the treatment of depression, anxiety disorders, insomnia, and several stress related disorders (Butler et al., 2006; Hoffman et al., 2012). Furthermore, this type of treatment has shown a higher efficacy than other intervention strategies, demonstrating its higher effectiveness when compared with other therapeutic approaches (Butler et al., 2006; Hoffman et al., 2012). As indicated, most studies were conducted in dementia patient caregivers, with significant positive results (Akkerman & Ostwald, 2004; Arango-Lasprilla et al., 2014; Selwood, Johnston, Katona, Lyketsos, & Livingston, 2007). Regarding ASD patient caregivers, few studies demonstrated the effectiveness of CBT in the reduction of health complaints and perceived stress (Bristol, Gallagher, & Holt, 1993; Hastings & Beck, 2008). To date, however, no specific CBT program focusing on stress management has been developed for and evaluated in family caregivers of people with ASD.
Recent research has identified several risk and protective factors for health outcomes in informal caregivers of people with ASD (Ruiz-Robledillo & Moya-Albiol, 2014a). These findings suggest that it would be worthwhile to develop and implement psychotherapeutic strategies based on these factors. The present study aimed to analyze the effectiveness of a CBT intervention program in reducing burden, somatic symptoms, and depression, and improving mood state in family caregivers of people with ASD. We hypothesized that caregivers would have fewer somatic and depressive symptoms after the intervention and at one-month follow-up and lower burden immediately after the intervention than at baseline (Bristol et al., 1993; Hastings & Beck, 2008; Ruiz-Robledillo et al., in press; Salt et al., 2002). Furthermore, we expected to find a significant reduction in negative mood states over the course of the whole intervention program, as has been previously described (Ruiz-Robledillo et al., in press).
MethodParticipants and ProcedureThe sample comprised 17 parents of ASD-diagnosed people (10 women and 7 men) who had cared for their offspring for approximately 14 years. Participants mean age was 52 years, most of them were married (76%) and with a high educational level (64.7%). With regard to the care recipients, 13 were males and 4 females with a mean percentage of disability of 75%. Caregivers were recruited from members of an association of relatives of people with ASD (Asociación Valenciana de Padres de Personas con Autismo, APNAV) in the region of Valencia (Spain). Firstly, a meeting was conducted with caregivers to explain the aim of the research and the criteria for participation, namely, being the mother or father of an individual with a clinical diagnosis of an ASD; living at home with the care recipient; and having been the primary caregiver (that is, the person with the greatest responsibility for the daily care and rearing of the child) for at least two years before the study. In this meeting, parents were told about the content and procedure of the intervention program. After indicating that they wished to participate in the study, selected parents were interviewed to collect demographic data and information about their caregiving status. They all took part in the study voluntarily and completed an informed consent form in accordance with the ethical principles for research involving human subjects (Declaration of Helsinki).
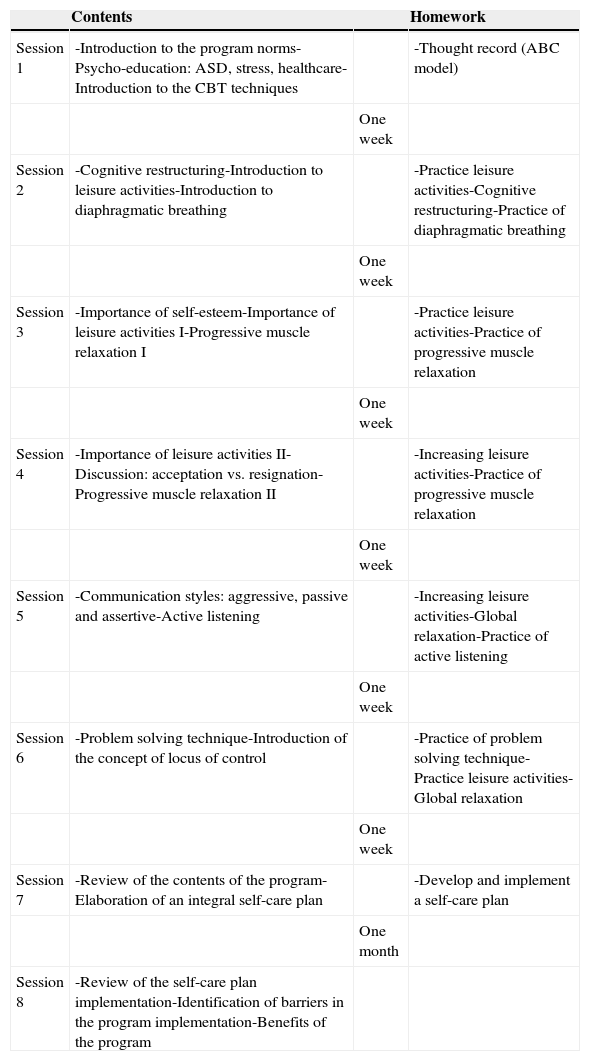
The intervention program consisted of eight 2-hour sessions once a fortnight. The program is fundamentally based on a cognitive-behavioral approach, employing therapeutic strategies that have demonstrated efficacy in stress reduction. Further, the therapy was adapted to the ASD care context, taking into account factors that have been shown to be modulators of health status in family caregivers of people with ASD, in order to increase its effectiveness in this population. The development of the content and the implementation of the program were undertaken by the first author, with the supervision of the second author. The content of the intervention is summarized in Table 1.
Content of the CBT program.
| Contents | Homework | ||
|---|---|---|---|
| Session 1 | -Introduction to the program norms-Psycho-education: ASD, stress, healthcare-Introduction to the CBT techniques | -Thought record (ABC model) | |
| One week | |||
| Session 2 | -Cognitive restructuring-Introduction to leisure activities-Introduction to diaphragmatic breathing | -Practice leisure activities-Cognitive restructuring-Practice of diaphragmatic breathing | |
| One week | |||
| Session 3 | -Importance of self-esteem-Importance of leisure activities I-Progressive muscle relaxation I | -Practice leisure activities-Practice of progressive muscle relaxation | |
| One week | |||
| Session 4 | -Importance of leisure activities II-Discussion: acceptation vs. resignation-Progressive muscle relaxation II | -Increasing leisure activities-Practice of progressive muscle relaxation | |
| One week | |||
| Session 5 | -Communication styles: aggressive, passive and assertive-Active listening | -Increasing leisure activities-Global relaxation-Practice of active listening | |
| One week | |||
| Session 6 | -Problem solving technique-Introduction of the concept of locus of control | -Practice of problem solving technique-Practice leisure activities-Global relaxation | |
| One week | |||
| Session 7 | -Review of the contents of the program-Elaboration of an integral self-care plan | -Develop and implement a self-care plan | |
| One month | |||
| Session 8 | -Review of the self-care plan implementation-Identification of barriers in the program implementation-Benefits of the program |
Mood state. Mood was evaluated using the abbreviated version of the Profile of Mood States (POMS), developed by Fuentes, Balaguer, Meliá, & García-Merita, 1995. This version is composed of 29 items configured by adjectives that respond to the question ‘How are you feeling right now?’ Items are grouped in five subscales: tension (e.g., tense, nervous), depression (e.g., sad, unhappy), anger (e.g. angry, bad-tempered), vigor (e.g., lively, energetic), and fatigue (e.g. fatigued, exhausted). A total score was also calculated by summing scores on all subscales, subtracting the vigor scale score and adding a constant of 100. The higher the total score, the worse the mood. Cronbach's alpha of this instrument is higher than .80.
Somatic symptoms. Somatic symptoms were assessed with the revised Spanish version of the Somatic Symptoms Scale (ESS-R) created by Sandín and Chorot (1995). This instrument is composed of 80 items focused on the frequency of immunological (e.g., influenza, general state of low energy), cardiovascular (e.g., tachycardia, elevated blood pressure), respiratory (e.g., repetitive sneezing, difficult breathing), gastrointestinal (e.g. nausea, constipation), neurosensory (e.g., gait instability, dizziness), muscular (e.g., backache, joint pain), dermatological (e.g., eczema, pimples on the skin), and genito-urinary (e.g., discomfort when urinating, difficulty urinating) complaints. Each scale is composed of ten items ranked on a five-point Likert scale from 0 (never) to 4 (more than five times in the last 2 years), with reliability coefficients ranging from .79 to .84. The total number of symptoms is also calculated.
Depressive symptoms. Depressive symptomatology was evaluated by the Beck Depression Inventory (Beck & Steer, 1993). This questionnaire assesses the intensity and severity of emotional, cognitive, and somatic aspects of depressive symptomatology through 21 self-report items ranked on a four-point Likert scale (e.g., crying: I don¿t cry anymore than I used to/I cry more than I used to/I cry over every little things/I feel like crying, but I can¿t; sadness: I do not feel sad/I feel sad much of the time/I am sad all the time/I am so sad or unhappy that I can¿t stand it). It has a reliability coefficient of .83.
Burden. Burden on the caregivers was evaluated using the Burden Interview created by Zarit, Reever, and Bach-Peterson (1980). This instrument is composed of 22 items ranked on a five-point Likert scale from 0 (never) to 4 (nearly always) with a maximum score of 88. The reliability coefficient is .92. The items are related to health, social, and personal lifestyle, and interpersonal relations with the care recipient who has functional and behavioral disabilities (e.g., “Do you feel that your relative currently affects our relationships with other family members or friends in a negative way?” “Do you feel your health has suffered because of your involvement with your relative?” “Do you feel that your social life has suffered because you are caring for your relative?”). For each of these domains, caregivers express their feelings of burden with the higher scores representing a greater burden.
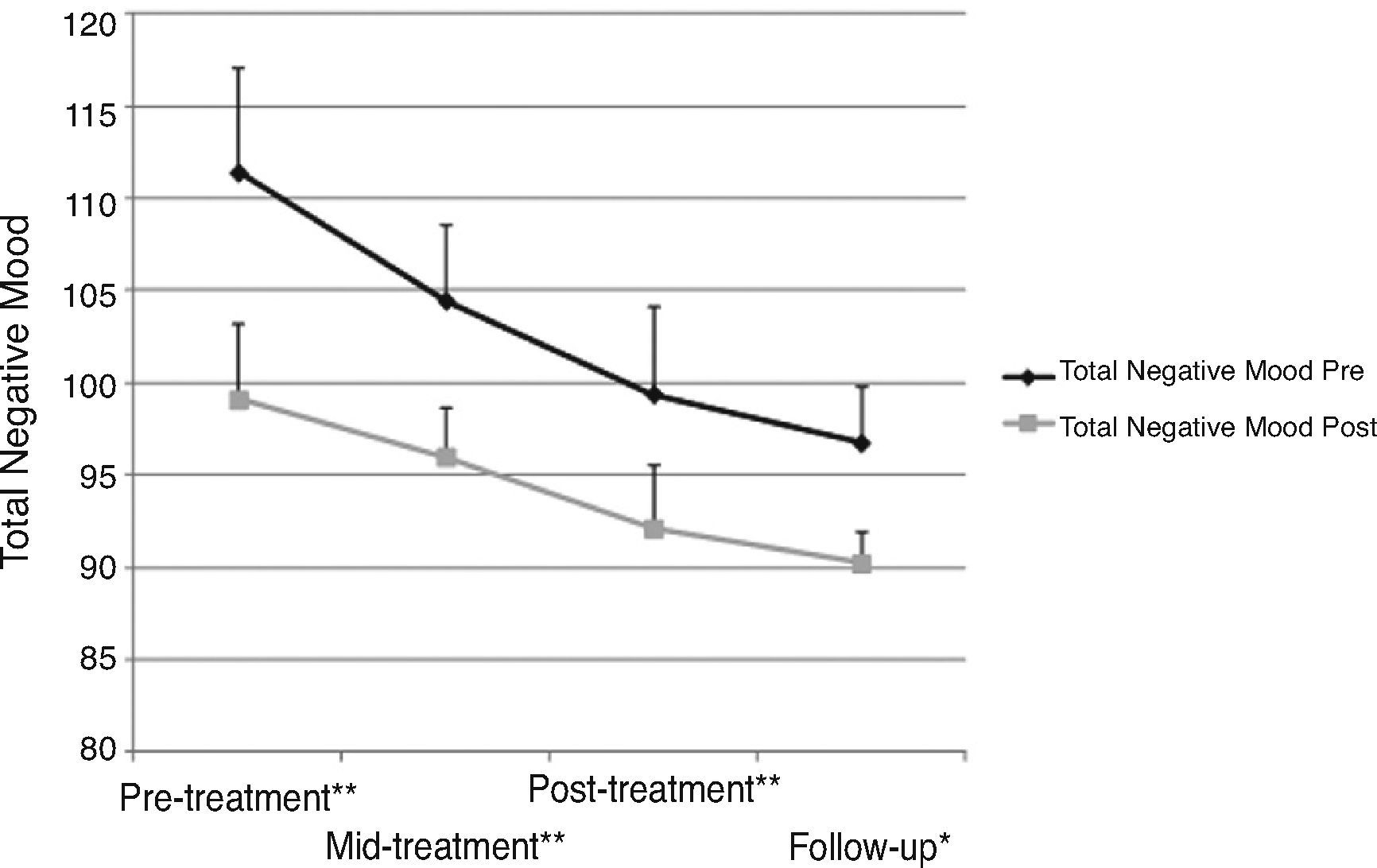
Evaluation ProcedureBurden was evaluated before and after the intervention. Somatic symptoms and depression were evaluated before the implementation of the intervention, immediately after the intervention and at 1 month of follow-up. Mood state was evaluated in session 1 (pre-treatment), session 4 (mid-treatment), and session 8 (post-treatment), and again 1 month later during the follow-up session. In the case of mood state, each participant completed the mood questionnaire before and after each of the aforementioned sessions.
Statistical AnalysesANOVA for repeated measures was performed to explore changes over time in somatic and depressive symptoms (comparing pre-treatment, post-treatment and follow-up scores) and in mood state (comparing pre-treatment, mid-treatment, post-treatment and follow-up scores). Greenhouse-Geisser adjustments to degrees of freedom and Bonferroni adjustments for multiple contrasts were applied as appropriate. For burden, a paired-sample t-test was employed (assessing differences between pre-and post-treatment scores).
All statistical analyses were performed using IBM SPSS Statistics (version 21.0), considering p < .05 to be significant. The descriptive values are expressed as mean and standard deviation (M and SD, respectively).
ResultsWas the Intervention Program Effective in Caregivers?- a)
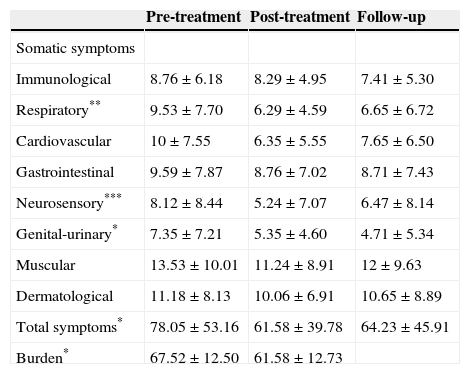
Somatic symptoms. There were significant changes over time in respiratory symptoms, F(1.845, 29.525) = 6.602, p = .005, η2partial = .292; neurosensory symptoms, F(1.824, 29.188) = 9.787, p = .001, η2partial = .380; and genito-urinary symptoms, F(1.777, 28.431) = 5.234, p = .014, η2partial = .246; as well as the total number of symptoms, F(1.435, 22.968) = 6.361, p = .011, η2partial = .284. For respiratory, neurosensory and total number of symptoms, post-hoc analyses revealed differences between pre-treatment scores and both post-treatment (p = .029, p =.004, and p = .050, respectively) and follow-up (p = .013, p =.050, and p = .006, respectively) scores. In all cases, caregivers had fewer symptoms post-treatment and at follow-up than pre-treatment. With regard to genito-urinary symptoms, caregivers had significantly fewer symptoms at follow-up than pre-treatment (p = .033) (Table 2).
Table 2.Scores (mean and standard deviation) in Somatic Symptoms and Burden in Pre- and Post-treatment and One Month Follow-up for Caregivers.
Pre-treatment Post-treatment Follow-up Somatic symptoms Immunological 8.76 ± 6.18 8.29 ± 4.95 7.41 ± 5.30 Respiratory** 9.53 ± 7.70 6.29 ± 4.59 6.65 ± 6.72 Cardiovascular 10 ± 7.55 6.35 ± 5.55 7.65 ± 6.50 Gastrointestinal 9.59 ± 7.87 8.76 ± 7.02 8.71 ± 7.43 Neurosensory*** 8.12 ± 8.44 5.24 ± 7.07 6.47 ± 8.14 Genital-urinary* 7.35 ± 7.21 5.35 ± 4.60 4.71 ± 5.34 Muscular 13.53 ± 10.01 11.24 ± 8.91 12 ± 9.63 Dermatological 11.18 ± 8.13 10.06 ± 6.91 10.65 ± 8.89 Total symptoms* 78.05 ± 53.16 61.58 ± 39.78 64.23 ± 45.91 Burden* 67.52 ± 12.50 61.58 ± 12.73 *p < .05, **p < .01, ***p < .001
- b)
Burden, depression, and negative mood state. In the case of burden, a significant reduction was found after the intervention, t(16) = 2.775, p = .014, d = 0.47.
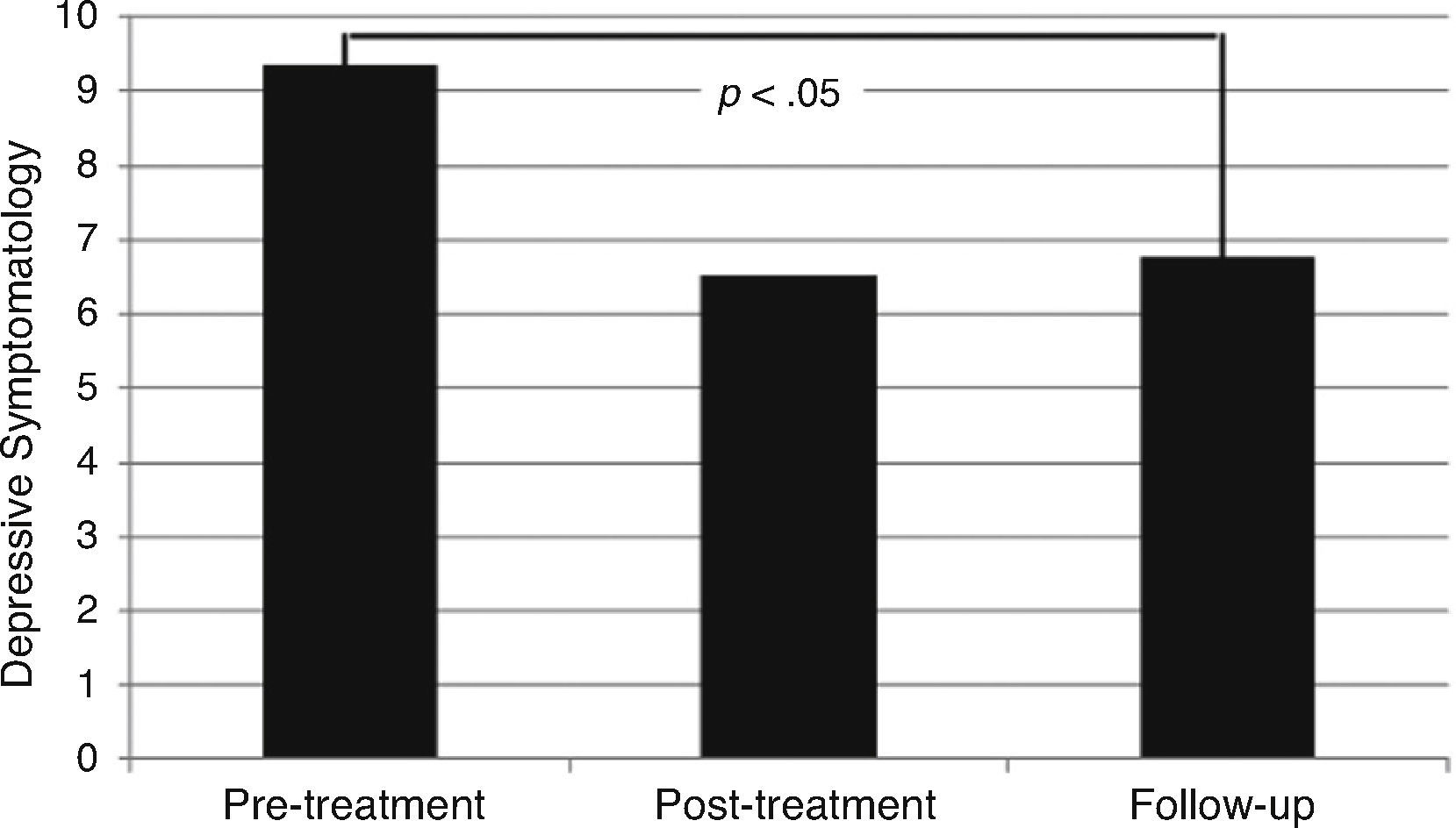
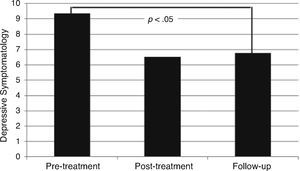
For depressive symptoms, changes over time were also significant, F(1.349, 21.581) = 5.329, p = .022, η2partial = .250, caregivers having fewer depressive symptoms at follow-up than pre-treatment (p =.014) (Figure 1).
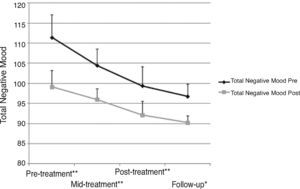
With regard to mood state, there were significant changes over time in scores for total negative mood, F(2.347, 37.559) = 9.913, p =.001, η2partial = .383, and all the subscales, namely, for depression, F(2.224, 35.583) = 7.568, p = .001, η2partial = .321; vigor F(2.484, 39.736) = 4.728, p = .010, η2partial = .228; anger, F(2.147, 34.347) = 4.833, p =.013, partial = .232); fatigue F(2.528, 0.447) = 3.762, p = .023, η2partial = .190); η2partial and tension, F(2.099, 33.590) = 5.845, p = .006, η2partial = .268). In the case of depression, vigor, and total negative mood, significant differences were observed from pre-treatment to mid-treatment (p = .010, p = .027, and p = .010 for each subscale respectively) and to follow-up(p = .004, p = .050, and p = .007 respectively). For fatigue and tension, differences were significant comparing pre-treatment and follow-up scores (p = .050 and p = .020, respectively). We only observed significant differences between post-treatment and follow-up in the case of total negative mood (p = .011). Post-hoc analyses did not identify any significant differences in anger. On all subscales except for vigor, scores fell progressively over the course of the whole intervention program. No significant interaction was observed between the time of measurement with respect to the session (pre-or post-session) and time of measurement with respect to the treatment (pre-/mid-/post-treatment or follow-up) for any of the mood scores evaluated (Figure 2)
DiscussionThe results of the present study demonstrate the effectiveness of the CBT program applied for reducing burden, somatic symptoms, depression, and mood disturbances in caregivers of people with ASD. The types of psychotherapeutic strategies employed in this study have also been found to be effective in previous studies conducted with informal caregivers (Losada-Baltar, Izal-Hernández, Montorio-Cerrato, Cobaleda, & Pérez-Rojo, 2004; Martínez et al., 2014). However, these earlier studies implemented interventions focusing on single techniques. In caregivers of people with dementia, two types of intervention, one oriented to the management of dysfunctional thoughts about informal caring and the other to problem-solving strategies, showed significant effectiveness for reducing stress levels, the program focusing on dysfunctional thoughts being more effective than those on problem-solving (Losada-Baltar et al., 2004). Problem-solving therapy was also found to be effective at reducing burden in caregivers of people with cerebral palsy (Martínez et al., 2014). In the present study, both skills were trained in the same integrated program. Probably the combination of these two types of skills, together with the other skills worked on during the program, increases the efficacy of the intervention. To our knowledge, this is the first study focused on the evaluation of a program integrating several cognitive-behavioral techniques adapted to the care context in caregivers of people with ASD.
The intervention applied focuses on strengthening skills that have been shown to be protective for health and reducing factors related to health deterioration in this population, following the model pro-posed by Ruiz-Robledillo and Moya-Albiol (2014a). There is evidence that depending on caregivers’ perception of the level of control they have over stressors, different coping strategies could be effective (Ruiz-Robledillo & Moya-Albiol, 2013). In the program, the following were discussed: the concept of locus of control, characteristics of the stressors, differences between acceptance and resignation, and effective coping depending on the perceived control of each stressor. In the case of high perceived control of the stressor, caregivers were encouraged to apply problem-solving strategies and active coping. On the other hand, leisure activities were encouraged and emotion regulation strategies, such as relaxation and cognitive restructuration, were worked on to help caregivers to manage stressors over which they had less control. This approach enables caregivers to pay less attention to negative feelings and acquire higher emotion regulation skills, which have been demonstrated to be directly related to better health status in this population (Ruiz-Robledillo & Moya-Albiol, 2014b). Increasing leisure activities and being present during these activities could help caregivers to reduce negative feelings, capitalizing on positive situations promoted by leisure activities. Furthermore, leisure activities could serve as a respite and an escape from the stress focus, something that has been shown to be related to positive health outcomes in this population (Ruiz-Robledillo & Moya-Albiol, 2013).
To our knowledge, no previous interventions conducted with caregivers of people with ASD have integrated training in effective communication styles and assertiveness. These skills are especially relevant in caregivers of people with ASD, taking into account that they are constantly in contact with educational, health, and other public services due to their caring role. Specifically, training in effective communication styles could reduce social anxiety potentially associated with these interactions. In turn, this could also reduce stress and negative health outcomes. In dementia patient caregivers, communication difficulties predicted significantly the burden (Savundranayagam, Hummert, & Montgomery, 2005). Hence, in a recent study, effective communication styles and assertiveness were included as a one of the main components of a CBT program, with positive results (Arango-Lasprilla et al., 2014). In addition, the effects of communication training have been effective in family caregivers of dementia patients, reducing distress and improving significantly the interaction with the care recipient and the medical staff (Done & Thomas, 2001; Ripich, Ziol, Fritsch, & Durand, 2000). However, this fact had not been proven in ASD patients’ informal caregivers, although they also have to interact constantly with several clinicians. On the other hand, the fact that to participate in the program caregivers join a group of individuals with the same caring role in itself increases their level of social support, through the interaction with peers, offering opportunities to learn about strategies employed by other caregivers and identified in relation to the problems discussed during the sessions (Boyd, 2002). In this sense, previous research demonstrated the effectiveness of peer support interventions in family caregivers of chronic disabling children (Shilling et al., 2013). In ASD patients’ caregivers, peer support based on email interaction showed positive results (Huws et al., 2001). Hence, the contents of the interactions were based generally in giving a sense to autism, trough the discussion of searching for meaning, adjusting to changes, providing peer support and sharing individual experiences. In the present study, the inherent performance of the program encouraged participants to share experiences, creating a sense of group integrated by individuals with a similar problem. This fact, as previously studied, is one of the main mechanisms underlying the effectiveness of group treatment. Sharing the same social identity, being able to help others and being also helped could enormously benefit caregivers (Shilling et al., 2013).
Overall, the program provides participants with a range of effective coping strategies and skills for dealing with everyday challenges associated with the care situation. The observed improvements in health are probably directly related to increases in resilience and coping, previous research indicating the positive effects of these skills on health status and mood (Ruiz-Robledillo et al., 2014). This fact has important and significant clinical implications for informal caregivers and clinicians. Firstly, caregivers’ health status and quality of life are closely related to the quality of the care provided to care recipients. Improving health in caregivers results in an increase in the quality of the provided care and in turn, in a better functioning and quality of life of care recipients. Furthermore, the improvement of caregivers’ health could reduce their medical visits and medication consumption, lowering the economical costs of their medical health-care. Moreover, the potential burden of medical institutions could be reduced, especially if this type of interventions could be applied early after the diagnosis of the care recipient. This would prevent the health deterioration of informal caregivers, and therefore, the costs derived from the medical attention of this population
Although the present study represents an advance in our understanding of which psychotherapeutic approaches may be effective for reducing health complaints and negative mood states in informal caregivers of people with ASD, several limitations have to be taken into account. The relatively small sample size and the pre-post design limit the conclusions that can be drawn about causality and the generalization of the findings. On the other hand, informal caregivers usually have extreme difficulties in attending to therapeutic programs due to a lack of time and commitments related to their caring role. In line with this, relatively few data are available concerning the effectiveness of interventions in this population. We believe that the results obtained in this study contribute to filling this gap in the literature and encourage efforts to develop and implement comprehensive interventions for caregivers.
Future studies should attempt to replicate the results with a larger sample size. Furthermore, it could be interesting to explore differences in the effectiveness of different intervention modalities and whether the effectiveness can be increased by combining additional therapeutic approaches for reducing health complaints in caregivers. New psychotherapeutic strategies such as mindfulness and yoga are also producing good results in informal caregivers (Ruiz-Robledillo et al., in press; Waelde, Thompson, & Gallaguer-Thompson, 2004). It is reasonable to suppose that individual caregivers benefit more or less from specific interventions depending on their personality traits and other psychosocial and contextual variables. Future studies should evaluate which types of variables could be significant predictors of the success of particular interventions in caregivers of people with ASD.
Conflict of InterestThe authors of this article declare no conflict of interest.
Financial SupportThis study was financed by the Spanish Ministry of Science and Innovation (PSI2008-0448/PSIC), and the Committee for Business, Research, and Science of the Regional Government of Valencia, research groups and networks of excellence (ACOMP/2010/250; PROMETEO/2011/048; ISIC/2013/001). This research is part of the doctoral dissertation project of the first author, financed by the University of Valencia (“Atracció de Talents” VLCCAMPUS 2011).