To comprehensively analyze national trends in sarcoidosis mortality in Spain between 1999 and 2023, with a focus on demographic differences and changes over time.
Material and methodsThis nationwide ecological study analyzed death registry data for sarcoidosis (ICD-10 code D86) from the Spanish National Institute of Statistics. Age-standardized mortality rates (ASMRs) were calculated by sex and age. Joinpoint regression assessed temporal trends and annual percentage changes (APCs).
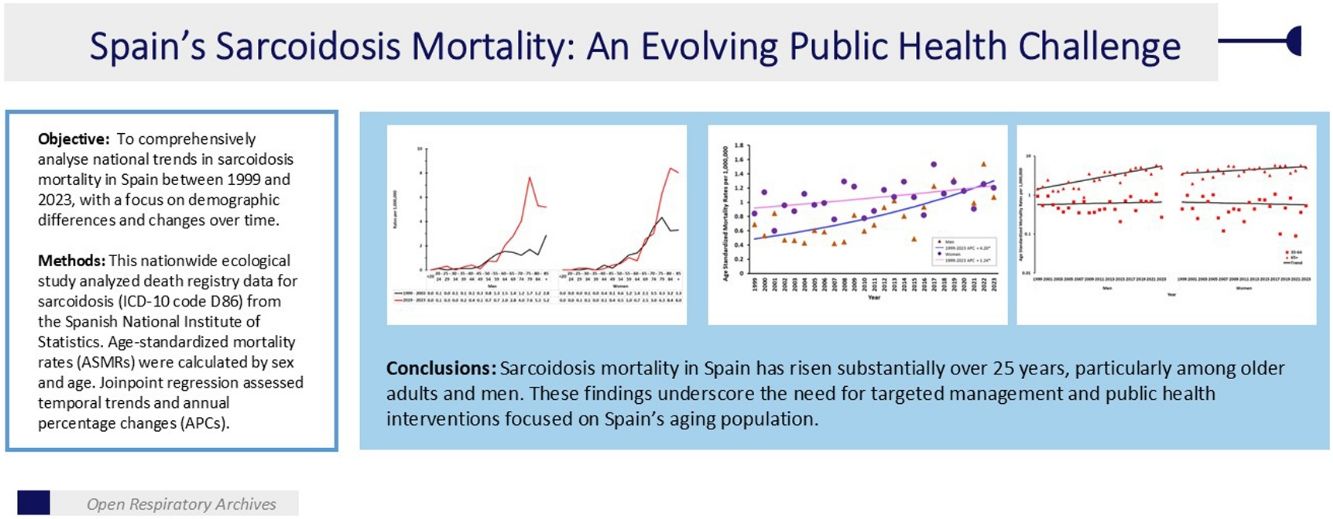
ResultsSpain recorded 1053 sarcoidosis deaths between 1999 and 2023, with women accounting for 61.8%. Overall deaths rose, peaking at 72 in 2022. Mortality was heavily concentrated among those aged≥65 years (75.8% of deaths). Age-specific mortality rates were negligible under 35, increasing markedly with age. Comparing 1999–2003 and 2019–2023 revealed rising mortality, especially among older adults; for example, men aged 70–74 saw rates increase from 1.22 to 4.06 per million, and women aged 80–84 from 3.24 to 8.40 per million. The male-to-female mortality ratio shifted over time, indicating a growing relative burden among men in several age groups. Joinpoint analysis showed steady ASMR increases: men's overall APC was +4.20%, driven by a 5.81% rise among those ≥65 years, while women's APC was +1.24%, primarily among those ≥65 years.
ConclusionsSarcoidosis mortality in Spain has risen substantially over 25 years, particularly among older adults and men. These findings underscore the need for targeted management and public health interventions focused on Spain's ageing population.
Analizar de manera exhaustiva las tendencias nacionales de mortalidad por sarcoidosis en España entre 1999 y 2023, con especial atención a las diferencias demográficas y a los cambios a lo largo del tiempo.
Material y métodosEste estudio ecológico a nivel nacional analizó los datos del registro de defunciones por sarcoidosis (código CIE-10 D86) del Instituto Nacional de Estadística. Se calcularon las tasas de mortalidad estandarizadas por edad (TMEA) según sexo y grupo etario. Se utilizó la regresión JoinPoint® para evaluar las tendencias temporales y los cambios porcentuales anuales (CPA).
ResultadosEntre 1999 y 2023, se registraron en España 1.053 muertes por sarcoidosis, con un 61,8% de los fallecimientos en mujeres. El número total de defunciones aumentó, alcanzando un máximo de 72 en 2022. La mortalidad se concentró en gran medida en personas de ≥65 años (75,8% de los fallecimientos). Las tasas de mortalidad específicas por edad fueron insignificantes en los menores de 35 años, aumentando notablemente con la edad. Al comparar los periodos 1999-2003 y 2019-2023, se observó un aumento de la mortalidad, especialmente entre los adultos mayores; por ejemplo, los varones de 70-74 años pasaron de 1,22 a 4,06 por millón, y las mujeres de 80-84 años de 3,24 a 8,40 por millón. La razón de mortalidad varón/mujer cambió a lo largo del tiempo, indicando una carga relativa creciente entre los varones en varios grupos etarios. El análisis JoinPoint® mostró aumentos constantes en las TMEA: el CPA global en los varones fue del +4,20%, impulsado por un aumento del 5,81% en los mayores de 65 años, mientras que en mujeres fue del +1,24%, principalmente en ese mismo grupo de edad.
ConclusionesLa mortalidad por sarcoidosis en España ha aumentado considerablemente en los últimos 25 años, especialmente entre los adultos mayores y los varones. Estos hallazgos subrayan la necesidad de intervenciones específicas en salud pública, y estrategias de manejo dirigidas a la población envejecida de España.
Sarcoidosis is a chronic, multisystem inflammatory disease characterized by the formation of non-caseating granulomas in affected organs. Although its exact aetiology remains elusive, the condition is widely understood to result from a complex interplay of genetic susceptibility, environmental exposures, and immune dysregulation.1,2 Clinical presentations range from asymptomatic forms to progressive disease with life-threatening complications. Pulmonary fibrosis, cardiac involvement, and neurosarcoidosis are among the most serious manifestations and represent the leading causes of sarcoidosis mortality.3,4
The global epidemiology of sarcoidosis exhibits notable geographical and demographic variability. According to data from the Global Burden of Disease (GBD) 2021 study, the age-standardized incidence and mortality rates for pulmonary sarcoidosis have shown an upward trend since 1990. In 2021, an estimated 390,000 new cases were recorded worldwide, with the highest rates observed among men, older adults (≥65 years), and populations in high-income regions, including North America and the Asia-Pacific.5 While part of this apparent increase may be attributable to enhanced diagnostic capabilities and heightened disease awareness, especially in countries with high sociodemographic indices, true incidence may also be rising due to ageing populations.5,6
In Spain, sarcoidosis epidemiology has followed a similarly evolving pattern. A population-based study conducted in northern Spain reported an incidence of 3.58 cases per 100,000 person-years, with a rising mean age at diagnosis and no significant sex disparities.7 Marked regional differences in mortality have been observed, with higher rates reported in northern areas such as Cantabria and Asturias, and lower rates in southern regions like Murcia.7–9 Between 1999 and 2013, age-adjusted mortality due to sarcoidosis in Spain remained relatively stable, although higher rates were consistently noted among women.10 In contrast, sarcoidosis related hospital admissions tripled between 2001 and 2020, reflecting increased healthcare utilization. Notably, in-hospital mortality remained steady at around 2.3%, potentially indicating improvements in clinical management.11
As sarcoidosis mortality predominantly affects older adults,5,12 analysing trends in the context of demographic ageing has become increasingly critical. This is particularly relevant for Spain, where the population is undergoing a rapid shift towards older age structures.
Therefore, this study aims to provide an updated and comprehensive analysis of national sarcoidosis mortality trends in Spain from 1999 to 2023, with a focus on demographic differentials and temporal dynamics.
Material and methodsStudy design and data sourcesWe conducted a nationwide, ecological time-trend study to examine sarcoidosis mortality in Spain over the 25-year period from 1999 to 2023. Mortality data were obtained from the Spanish National Institute of Statistics (Instituto Nacional de Estadística, INE), identifying deaths in which sarcoidosis was recorded as the underlying cause (ICD-10 code D86). Annual mid-year population estimates stratified by sex and single-year age groups were retrieved from the INE's publicly accessible database (https://www.ine.es/) for rate calculations.
Mortality rate calculationWe calculated crude and age-specific mortality rates per 1,000,000 population by sex. To account for changes in population age structure and enable comparisons over time, age-standardized mortality rates (ASMRs) were computed using the direct standardization method with the 2013 European Standard Population as the reference. Additionally, truncated ASMRs were calculated for individuals aged 35–64 years and ≥65 years, given the higher sarcoidosis burden observed in these age groups.
Trend analysisTemporal trends in ASMRs were assessed using Joinpoint regression analysis (Joinpoint Regression Program, version 5.2.0.0, U.S. National Cancer Institute). This method identifies statistically significant changes in linear trends (termed “joinpoints”) and estimates the annual percentage change (APC) for each segment. The average annual percentage change (AAPC) was computed to summarize the overall trend across the study period. Analyses were stratified by sex and truncated age groups (35–64 and ≥65 years). Pairwise comparisons of sex-specific trends were also performed. Statistical significance was defined as a two-sided p-value<0.05; trends with non-significant APCs were considered stable.
ResultsBetween 1999 and 2023, a total of 1053 deaths in Spain were officially attributed to sarcoidosis as the underlying cause, highlighting the disease's contribution to national mortality. Women accounted for a substantial majority of these deaths, with 651 cases (61.8%), compared to 402 deaths among men (38.2%). Annual mortality counts fluctuated, ranging from a low of 25 deaths in both 2001 and 2007 to a peak of 72 in 2022, revealing a general upward trend in recent years (Fig. 1A). Throughout the study period, the yearly number of deaths among men varied between 6 and 35, while among women, it ranged from 12 to 41.
Mortality was overwhelmingly concentrated among older adults (≥65 years), underscoring the impact of sarcoidosis on ageing populations. Individuals aged 65 years or older accounted for 75.8% of all sarcoidosis deaths, representing 66.9% of male deaths and 81.3% of female deaths (Fig. 1B). This age-based concentration was reflected in age-specific mortality rates, which remained negligible for individuals under 35 and increased progressively in middle-aged and older groups (Fig. 2).
A comparison between two time periods—1999–2003 (early) and 2019–2023 (most recent)—revealed a general rise in age-specific mortality rates for both sexes, especially among older adults (≥65 years) (Fig. 2). Mortality rates among men under the age of 30 remained consistently low across both periods. However, mortality rates increased substantially from the age of 60 onwards. In particular, the rate in the 70–74 age group rose sharply from 1.22 to 4.06 per 1,000,000 population. A similar trend was observed in the 75–79 age group, where mortality escalated from 1.70 to 7.68 per 1,000,000, and among men aged 85 and older, where it increased from 2.87 to 5.20 per 1,000,000. In contrast, younger and some middle-aged male groups showed minimal changes or slight decreases in mortality rates.
Among women, mortality remained low below age 30. While rates in middle-aged groups were generally stable or slightly decreased, significant increases were seen in older age groups. In the 75–79 group, mortality increased from 4.34 to 6.31 per 1,000,000, while in women aged 80–84, rates more than doubled, rising from 3.24 to 8.40 per 1,000,000. Among those aged 85 and older, mortality increased from 3.31 to 8.05 per 1,000,000 (Fig. 2).
Analysis of mortality trends over time by sex revealed notable shifts. In 1999–2003, the male-to-female mortality rate ratio (M/F ratio)—calculated as the mortality rate in men divided by that in women—remained below one across most older age groups, reflecting a higher mortality burden among women. By 2019–2023, this pattern reversed in several age cohorts, suggesting a growing relative burden for men. For instance, the M/W ratio increased from 0.33 to 3.96 in the 40–44 age group, from 0.34 to 1.35 in the 70–74 group, and from 0.39 to 1.22 in the 75–79 group. Conversely, the 45–49 group showed an inverse trend, with the M/W ratio declining from 2.02 to 0.25, indicating higher mortality in women within this bracket. Despite these shifts, women consistently exhibited higher mortality rates in the oldest age groups (80–84 and ≥85 years), although the disparity between sexes narrowed over time.
Joinpoint regression analysis indicated steady linear trends in age-standardized mortality rates (ASMRs) throughout the study period, with no abrupt changes. Among men, the overall ASMR (all ages combined) increased annually by 4.20% on average (annual percentage change, APC) (Fig. 3). This rise was driven primarily by men aged 65 and older, who experienced an APC of 5.81%, indicating a sustained increase in mortality over time. Men aged 35–64 exhibited a lower annual percent change (APC) of 0.62%, suggesting minimal variation in mortality rates throughout the study period (Fig. 4). Among women, the overall ASMR also increased but at a slower pace, with an APC of 1.24%. This trend was largely influenced by women aged 65 and older, who had an APC of 1.68%, indicating a moderate rise in mortality. In contrast, women aged 35–64 showed stable mortality, with an APC of −0.65% (Fig. 4).
This nationwide ecological study offers the most comprehensive and up-to-date analysis of sarcoidosis mortality trends in Spain from 1999 to 2023. Our findings significantly expand upon earlier regional and national reports, including insights from Cantabria and Catalonia, by revealing a significant and sustained increase in age-standardized sarcoidosis mortality rates.7–10 This upward trend is particularly pronounced among older adults and men, highlighting an evolving epidemiological profile of sarcoidosis that mirrors Spain's ageing population and shifting demographic patterns. These mortality trends are noteworthy given the generally low to moderate incidence of sarcoidosis in Spain, typically ranging from 1 to 4 per 100,000 per year, which is characterized by frequent thoracic and cutaneous involvement and notable regional variation in clinical presentation.7,13–15
The observed increase in sarcoidosis mortality in Spain—reflected by a rise in annual deaths from 25 to 72 and annual growth in age-standardized mortality rates (ASMRs) of 4.20% in men and 1.24% in women—parallels trends reported in international studies.5,6 While women showed higher absolute mortality counts throughout most of the study period, the age-standardized mortality rates revealed a steeper relative increase among men. This apparent discrepancy reflects the different baseline mortality rates between sexes and the standardization process that accounts for population age structure differences. For instance, in the United States, sarcoidosis ASMR climbed from 3.9 per 100,000 in 1999 to 6.4 in 2020, exhibiting three distinct phases: a sharp increase (1999–2001), a plateau (2001–2018), and a resurgence (2018–2020).16 This recent increase in the US has been attributed to changes in coding practices, improved diagnostic imaging—such as high-resolution computed tomography (HRCT) and positron emission tomography (PET) imaging—and persistent challenges in managing advanced sarcoidosis-associated pulmonary fibrosis (SAPF).16 Similarly, upward trends have been reported in England, where age- and sex-standardized incidence rates increased from 6.65 to 7.73 per 100,000 person-years between 2003 and 2023, with the steepest rise occurring between 2010 and 2016.17 Japan also experienced a 2.46-fold increase in age-adjusted sarcoidosis mortality.18 These international observations collectively suggest that Spain's experience is part of a broader epidemiological shift occurring in many developed countries.
Our results diverge from earlier Spanish data spanning 1999–2013, which indicated relatively stable ASMR.10 This difference likely stems from our longer study period and refined diagnostic methodologies, enabling us to capture more recent increases in mortality. Importantly, our findings are consistent with the documented threefold increase in sarcoidosis-related hospital admissions in Spain between 2001 and 2020, with crude rates rising annually by 4–6% for both sexes. This significant rise in hospital admissions points to heightened disease recognition and diagnosis, which could partially explain the increasing reported mortality despite stable in-hospital fatality rates, hovering around 2.3%.11
A notable feature of our findings is the burden of sarcoidosis deaths in older adults (≥65 years), with individuals aged 65 years and older accounting for over three-quarters of all fatalities. Mortality rates are very low in younger populations but rise sharply with age, especially in women aged 75–84 and men aged 70–74. This late-life increase likely reflects several factors, including longer life expectancy, better recognition of sarcoidosis as a cause of death, and higher rates of comorbidities such as cardiovascular disease, diabetes, and chronic lung conditions. Gender-specific factors may also play a role, as older women (≥65 years) are more prone to chronic progressive pulmonary sarcoidosis and severe extrapulmonary complications. This observation aligns with prior studies indicating that sarcoidosis mortality disproportionately affects the elderly.5,12 This pattern is also consistent with Spanish epidemiological data showing a trend towards increasing age at diagnosis over time, with a second incidence peak emerging in the 60–69 age group for both sexes.7 Crucially, elderly patients (≥65 years) in Spain experience particularly poor outcomes, with a sarcoidosis mortality rate of 6.4% compared to 1.3% in younger patients. These older individuals are more likely to present with advanced pulmonary involvement (Scadding stage III/IV), isolated extrapulmonary disease, and less frequently with the favourable Löfgren syndrome phenotype. They also exhibit lower rates of remission and a higher incidence of pulmonary fibrosis, directly contributing to the elevated mortality risk observed in our study.19
The more than threefold increase in mortality among men aged 70–74 and the doubling of rates among women aged 80–84 between 1999–2003 and 2019–2023 underscore the growing public health impact of sarcoidosis within ageing populations. The seemingly paradoxical finding of higher female absolute mortality but steeper male mortality trends reflects several factors: (1) women's longer life expectancy results in a larger population at risk in older age groups where sarcoidosis mortality peaks; (2) men started from a lower baseline mortality rate, making relative increases appear more pronounced; and (3) recent convergence in mortality rates suggests changing disease patterns or diagnostic practices that may disproportionately affect men. Spain's demographic shift towards an older age structure further suggests that the absolute number of sarcoidosis deaths may continue to rise even if age-standardized rates stabilize. This observation is also consistent with post-2020 trends, where a surge in mortality was observed among men aged ≥65 years, potentially reflecting the disproportionate impact of the COVID-19 pandemic on older sarcoidosis patients due to immunosuppression, disrupted care, or delayed diagnosis. This is consistent with recent population-based data from northern Spain, which also show a trend towards increasing age at diagnosis and a second incidence peak in the 60–69 age group.7
The marked increase in sarcoidosis mortality during 2020–2022, particularly among men aged 65+, likely reflects multiple pandemic-related factors: (1) Direct COVID-19 impact, as sarcoidosis patients may face increased susceptibility to severe COVID-19 due to immunosuppressive treatments and underlying pulmonary compromise, with the inflammatory nature of both conditions potentially creating synergistic effects that increase mortality risk; (2) Healthcare system disruptions, including delayed routine care, postponed specialist appointments, and reduced monitoring of immunosuppressive therapies, which may have led to disease progression and increased complications; (3) Diagnostic challenges, as COVID-19 and pulmonary sarcoidosis share similar radiological features, potentially leading to delayed or missed diagnoses, inappropriate treatment decisions, or misattribution of cause of death; and (4) Indirect effects, such as social isolation, medication access issues, and delayed emergency care seeking, which may have disproportionately affected older adults with chronic conditions like sarcoidosis. The gender disparity observed during this period warrants further investigation, as it may reflect differences in healthcare-seeking behaviour, occupational exposures, or baseline cardiovascular risk factors that interact with both sarcoidosis and COVID-19.
Arguably the most striking finding is the evolving sex-specific pattern of sarcoidosis mortality observed over the course of the study period. Historically, sarcoidosis mortality has often been reported as higher in women, consistent with the overall female predominance in sarcoidosis incidence.12 In Spain, earlier studies from Catalonia reported a strong female predominance (3:1), although more recent cohorts from Barcelona show this ratio has narrowed to approximately 2:1, and population-based data from northern Spain show no significant gender predominance.7,8,13 According to international evidence, women consistently had higher ASMR than men in the United States from 1999 to 2020,16 and constituted 65.3% of sarcoidosis deaths in Japan between 2001 and 2020.18 Previous Spanish research also reported higher mortality rates among women.19
However, our data reveal a complex evolution in sex-specific mortality patterns that challenges these traditional assumptions in certain age groups and time periods. This evolution parallels the documented narrowing of the gender gap in Spanish hospitalization data, where women historically had higher incidence but the difference between sexes has decreased over time.11 The dramatic changes in male-to-female mortality ratios across age groups suggest fundamental shifts in disease presentation, severity, or management. Specifically, the emergence of higher male mortality in several middle-aged and older age cohorts may reflect distinct sex-specific disease characteristics becoming more pronounced over time. Research from Spanish cohorts indicates that age, gender, and ethnicity influence clinical presentation, with older patients showing more renal and metabolic involvement, which may contribute to worse outcomes in ageing male populations.20 Recent research also indicates men often present with more severe disease at a younger age, while women more commonly experience skin and salivary gland involvement.21
The 5.81% annual percentage change in ASMR among men aged 65 and older, compared to 1.68% in women of the same age group, strongly indicates that older men are experiencing disproportionately worse outcomes. This disparity could stem from several factors, including: delayed diagnosis due to differing clinical presentations, greater exposure to occupational or environmental factors more common in men, or inherent biological differences in disease progression and treatment response. The potential contribution of comorbidities in older adults should also be considered, although our dataset does not allow direct analysis of other causes of death. Future studies could leverage CMBD or regional hospital data to explore the interplay between sarcoidosis and comorbid conditions.
One hypothesis for the sharp increase in mortality among US men during 2018–2020 links it to delayed diagnosis, higher baseline comorbidity rates, and increased vulnerability during the COVID-19 pandemic.16 In Spain, COVID-19 has been identified as a key predictor of in-hospital mortality in sarcoidosis patients, particularly affecting older adults with comorbidities.11 It is also well-documented that sarcoidosis can manifest differently in men and women, with some studies suggesting more severe manifestations in men.2,21
The stability of ASMR in middle-aged groups (35–64 years) suggests that the growing overall burden of sarcoidosis mortality is mainly driven by older adults. This pattern may reflect improvements in early diagnosis and management for younger and middle-aged patients, resulting in better long-term outcomes. In contrast, older patients—often presenting with more comorbidities or advanced disease—face higher mortality risks.4,22 The clinical phenotype of sarcoidosis in Spain, characterized by frequent thoracic involvement as the most common presentation and skin, joints, and eyes as the most frequently affected extrathoracic sites, may contribute to these different long-term outcomes across age groups.7 The progression of sarcoidosis to severe forms such as pulmonary fibrosis, cardiac sarcoidosis, and neurosarcoidosis, which are major causes of death, is particularly relevant in this older population.3,4 The concurrent rise in incidence among men and individuals over 60 observed in England further highlights the need for healthcare systems to adjust to an ageing sarcoidosis population with increasingly complex care needs.17
Despite the low to moderate incidence of sarcoidosis in Spain compared to northern European countries—with Spain sharing the Mediterranean pattern of lower incidence rates but higher prevalence of skin involvement and Löfgren's syndrome—the significant increase in mortality we observed indicates that the disease burden extends beyond simple incidence metrics.14,15 While a threefold increase in hospital admissions in Spain between 2001 and 2020 and stable in-hospital mortality rates suggest advances in acute care management, our findings of increasing overall mortality point to a shift towards chronic, community-based complications.11 It is important to note that regional differences in sarcoidosis incidence and outcomes exist in Spain and future research should investigate geographic heterogeneity to understand potential environmental, healthcare, or demographic influences. Similar trends reported in England, with rising incidence among men and older adults, emphasize the importance of healthcare systems adapting to these demographic changes.17 Priorities should include long-term monitoring and management of chronic complications, particularly pulmonary fibrosis and cardiac involvement.3
Our study has several limitations. Relying solely on death certificate data may underestimate the true burden of sarcoidosis mortality due to potential underreporting or misclassification, especially when sarcoidosis is a contributing rather than the primary cause of death. The ICD-10 coding system may not fully capture deaths related to sarcoidosis complications such as pulmonary fibrosis or heart failure. Furthermore, we could not analyze disease phenotypes or severity, which might offer further explanations for the observed trends. Additionally, while our study utilized national mortality data from the Spanish National Institute of Statistics providing comprehensive coverage of all deaths in Spain, it does not capture potential regional variations in sarcoidosis mortality that may exist due to geographic, environmental, or healthcare access differences across Spain's autonomous communities. Unlike previous regional studies conducted in specific autonomous communities (e.g., Cantabria, Murcia)7,8,13 that we reference for comparison, our analysis encompasses the entire Spanish population, offering a broader epidemiological perspective but without the granular regional detail.
Additionally, our mortality data cannot account for the documented regional variation in clinical presentation across different Spanish regions, from the higher frequency of Löfgren's syndrome in Catalonia to the distinct demographic patterns observed in northern Spain.
Nevertheless, the 25-year duration allows for detection of meaningful long-term trends. National death registry data provide comprehensive population coverage, minimizing selection bias common in hospital-based studies. Joinpoint regression offers robust trend analysis, and age standardization enables valid comparisons across time despite demographic shifts.
Our findings carry several important implications for clinical practice and public health planning. The predominance of sarcoidosis mortality among older adults underscores the need for geriatric-centred care strategies, incorporating comprehensive evaluation of comorbidities, potential drug interactions, and quality-of-life considerations. The evolving sex disparities we observed warrant further investigation into potential occupational, environmental, or genetic factors that may differentially affect men and women over time. Healthcare providers should be aware that traditional assumptions about female predominance in sarcoidosis mortality may no longer apply across all age groups and time periods. Given the established clinical phenotype of sarcoidosis in Spain, with its characteristic pattern of thoracic and cutaneous involvement and regional variations in presentation, targeted surveillance and management strategies should be developed that account for these specific epidemiological features.7,14,15 Research has also shown significant differences between sexes in health-related quality of life, highlighting the importance of gender-specific care approaches.23 The concentration of mortality in older adults particularly underscores the importance of long-term monitoring and management of chronic complications, especially pulmonary fibrosis and cardiac sarcoidosis.3
In conclusion, sarcoidosis mortality in Spain has risen significantly over the past 25 years, driven primarily by older adults and men. These trends occur within the context of Spain's distinctive sarcoidosis epidemiology, characterized by low to moderate incidence, evolving demographic patterns, and a clinical phenotype marked by frequent thoracic and cutaneous involvement with significant regional variation. These findings underscore the changing epidemiology of sarcoidosis and the urgent need for targeted public health interventions, improved diagnostic strategies, and specialized management for older patients. Future research should explore the underlying causes of these demographic shifts to ultimately reduce sarcoidosis mortality within ageing populations globally.
Ethics statementAll data were de-identified and publicly available, obviating the need for ethical approval. The study complies with the Declaration of Helsinki and follows STROBE reporting guideline.
Declaration of generative AI and AI-assisted technologies in the writing processChatGPT was used to assist with language and style editing during the preparation of this manuscript. The content was subsequently reviewed and edited by the authors, who take full responsibility for its accuracy and integrity.
FundingThere was not funding source for this study.
Authors’ contributionsLucia Cayuela: Conceptualization; Methodology; Visualization; Manuscript drafting; Data interpretation and discussion. Anna Michela Gaeta: Manuscript revision and editing; Data interpretation and discussion. Victoria Achaval Rodríguez: Data interpretation and discussion. Sara Cabrera Fernández: Data interpretation and discussion. Aurelio Cayuela: Conceptualization; Methodology; Visualization; Manuscript drafting; Data interpretation and discussion.
All authors critically revised the manuscript for important intellectual content. They approved the final version to be published and agree to be accountable for all aspects of the work, ensuring that any questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflicts of interestThe authors declare that they have not conflict of interest.
Data availabilityThe data for this study are publicly available through the https://www.ine.es/.