According to numerous studies, using emergency medical services (EMS) to transport stroke patients to hospitals decreases diagnostic and treatment delays.
ObjectivesTo determine the frequency of use of EMS by stroke patients in Bizkaia (Spain), analyse the factors associated with using EMS, and study the impact of EMS on time to care.
MethodsWe gathered data from 545 patients hospitalised for acute ischaemic stroke and recruited consecutively. Data were obtained from the patients’ medical histories and interviews with the patients themselves or their companions. We studied the following variables: previous health status, stroke symptoms and severity (NIHSS), type of transport, and time to medical care. Univariate and multivariate analyses were performed to identify factors associated with use of EMS and care delays.
ResultsPatients transported to hospital by the EMS accounted for 47.2% of the total. Greater stroke severity, arriving at the hospital at night, and poor functional status at baseline were found to be independently associated with use of EMS. Use of EMS was linked to earlier arrival at the hospital. Door-to-imaging times were shorter in the EMS group; however, this association disappeared after adjusting for stroke severity. Revascularisation was more frequent among patients transported by the EMS.
ConclusionsEMS transport was associated with shorter prehospital delays. Effective health education programmes should be developed to promote EMS transport for patients with stroke symptoms. In-hospital stroke management should also be improved to reduce time to medical care.
Numerosos estudios han establecido que el traslado al hospital de los pacientes con ictus por los servicios de transporte sanitario urgente (TSU) implica demoras menores hasta el diagnóstico y tratamiento.
ObjetivosDeterminar la frecuencia de uso de TSU por los pacientes con ictus en Bizkaia (España), qué factores se asocian con el mismo y el impacto del medio de transporte en los tiempos de atención.
MétodosSe analizaron los datos de 545 pacientes con ictus isquémico agudo hospitalizados y reclutados consecutivamente. Se obtuvieron datos por entrevista a pacientes o acompañantes y de historia clínica. Se estudiaron variables sobre situación previa, síntomas y gravedad (NIHSS) del ictus, modalidad de traslado y tiempos de atención. Se realizaron análisis univariados y multivariados para identificar factores asociados al uso de TSU y con las demoras.
ResultadosEl 47,2% de los pacientes llegaron al hospital trasladados por TSU. Una mayor gravedad del ictus, la llegada al hospital en horario nocturno y un peor estado funcional previo resultaron asociados de forma independiente con el TSU. El TSU se asoció a una llegada más precoz al hospital. La demora puerta-imagen fue menor en el grupo TSU, pero la asociación desapareció al ajustar por gravedad. La revascularización fue más frecuente entre los trasladados por TSU.
ConclusionesEl TSU se asoció a menor demora prehospitalaria. Es necesario desarrollar programas efectivos de educación sanitaria para incrementar el uso de TSU ante los síntomas del ictus. Debe mejorarse la gestión intrahospitalaria del ictus para reducir los tiempos de atención.
Increased understanding of the nature of ischaemic stroke and the recent advances in diagnosis and treatment have put stroke in the spotlight of neurological care. Delays in patients’ arrival at hospital constitute one of the main challenges to increasing revascularisation rates.1–4 Short transport times are also beneficial for patients who are ineligible for revascularisation, as they increase the effectiveness of such other measures as monitoring of oxygenation, arterial pressure, glycaemia, temperature, or cardiac function.5–7 Organisational barriers within hospitals or the healthcare network may be a factor in the low rate of revascularisation.5,8 Dispatching emergency medical transport (EMT) has been shown to shorten the time to diagnosis and treatment and to increase the frequency of revascularisation.9–21 According to several studies conducted in Europe and the US, 50% to 70% of patients are transported to hospital by EMT.9–11,14,15,17,18,22–24 Prehospital and in-hospital code stroke protocols contribute to earlier arrival at hospital, enable prenotification, and increase the likelihood of revascularisation.3,25–28
In our setting, no data are available on the type of transport stroke patients use to travel to hospital or the impact of transport type on the hospital care received.
This study aims to determine: 1) the frequency of EMT use by patients admitted to acute care hospitals in Biscay due to ischaemic stroke, 2) the characteristics differentiating EMT users from non–EMT users, and 3) the effectiveness of EMT for reducing times to hospital and to neuroimaging studies.
Material and methodsWe performed a multicentre, prospective, observational study of ischaemic stroke patients admitted to the 4 public acute care hospitals of Biscay. The Clinical Research Ethics Committee of the Basque Country approved the research protocol.
The participating centres were Hospital Universitario Basurto, Hospital Universitario Cruces, Hospital Galdakao-Usansolo, and Hospital San Eloy. These hospitals provide care to 96% of patients with stroke in Biscay (1150000 inhabitants); the first 3 have stroke units. In the area covered by Hospital San Eloy, patients eligible for revascularisation are transferred to Hospital Universitario Cruces, either directly when they arrive by EMT or by Hospital San Eloy's emergency department when they arrive by other means. For the purposes of this study, Hospital Universitario Cruces and Hospital San Eloy have been treated as a single centre since they act as a single functional unit for stroke care in the region.
The study population comprised all patients older than 18 who were admitted to the neurology departments of the participating hospitals (or the internal medicine department in the case of Hospital San Eloy) due to ischaemic stroke or transient ischaemic attack. In Biscay, only around 10% of patients with brain haemorrhages are treated at neurology departments; these patients were therefore not included in our study.
We excluded all cases of stroke during hospitalisation, patients who could not be stabilised, and those with whom it was not possible to establish sufficient communication.
Published data on symptom-to-door time and door-to-imaging time from patients arriving by EMT and by other means were used as a reference for calculating the sample size. We aimed to detect a 20% difference and calculated a sufficient sample to obtain estimates for each centre with α=0.05 (bilaterally) and ß=0.10. We used stratified sampling with proportional allocation to reflect the proportion of patients admitted to each hospital.
Recruitment period. Patients were recorded consecutively beginning on 12 January 2015. We included all patients meeting the inclusion criteria until the desired sample size was reached, which occurred on 25 June at Hospital Universitario Basurto, on 27 May at Hospital Universitario Cruces, on 20 July at Hospital Galdakao-Usansolo, and on 25 May at Hospital San Eloy.
Data collection. During the recruitment period, we prospectively recorded data from patients’ daily examinations, requested informed consent, and interviewed patients or their companions. We recorded the following data: functional status before stroke (modified Rankin Scale [mRS]),29 whether the patient was with somebody else at symptom onset, symptom interpretation by the patient/companion, and type of transport to hospital. We also used clinical histories to collect data on the age, sex, address, medical history (stroke, cardiovascular risk factors), time of symptom onset (according to the patient/companion [96%], or last time the patient was seen to be asymptomatic in the case of symptom onset upon waking [4%]), time of arrival at the hospital, time of neuroimaging study, whether the patient underwent revascularisation, and revascularisation technique used, where applicable. For patients transferred to Hospital Universitario Cruces from the Hospital San Eloy emergency department, we recorded the time and means of arrival at the latter. To avoid delays, neuroimaging studies were performed at Hospital Universitario Cruces. We also gathered data on symptoms, stroke severity at admission (National Institutes of Health Stroke Scale [NIHSS]),30 and stroke type. Each patient was assigned a socioeconomic level (Medea index)31 based on the census section corresponding to their home address. Data related with the EMT (time of telephone call, departure point, and activation of prehospital code stroke, where applicable) were obtained from the records of the Basque Health Service's emergency medical transport network.
In Biscay, prehospital code stroke is activated in cases of suspected stroke with a progression time of less than 6hours, but not for patients with severe impairment prior to stroke. Prehospital code stroke is activated by the emergency services physician, who answers the telephone call and notifies the on-call neurologist; the latter activates the in-hospital code stroke protocol for diagnosis and treatment.
We calculated the mean driving distance between the departure point and the hospital using Google Maps.
We gathered data on variables related to the care process: symptom-to-door time and door-to-imaging time. This study does not analyse door-to-revascularisation time due to the wide range of revascularisation techniques and the small number of patients receiving this treatment.
Regarding transport, we established 3 groups: Group 1: patients transported from the place of symptom onset to hospital by an EMT vehicle (ambulance, dispatched immediately, with capacity to alert emergency departments of prehospital code stroke) and attended exclusively by emergency department professionals. Group 2: patients previously attending other healthcare services (primary care physician, continuous care, private healthcare providers) and transported either by an EMT ambulance, a patient transport vehicle, or a private vehicle. Group 3: patients arriving at the hospital by other means, without consulting any healthcare professionals. In some parts of the analysis, groups 2 and 3 were classified into a single category, “non-EMT,” in contrast with the category “EMT”, which corresponds to group 1.
Statistical analysis. Categorical variables are expressed as frequencies (percentages). Quantitative variables were not normally distributed; we therefore calculated medians (Me) and the 25th and 75th percentiles (P25, P75). We performed a univariate analysis to compare patient characteristics by transport type, using the Mann–Whitney U test for quantitative variables and the chi-square test for categorical variables. We performed a multivariate analysis using binary logistic regression to identify the variables independently associated with type of transport; mRS and NIHSS scores were regarded as dichotomous variables (0-1 vs 2-5 and 0-3 vs ≥ 4, respectively). The median was used as the cut-off point. A logistic regression analysis was performed to determine whether transportation by EMT is associated with shorter symptom-to-door and door-to-imaging times; these outcome variables were regarded as being dichotomous (≤ 3h vs > 3h and ≤ 25min vs > 25min, respectively). The logistic regression analysis included the variables with P-value<.10 in the univariate analysis. The threshold of statistical significance was set at an alpha level of 0.05 for all analyses. Statistical analysis was performed using SPSS Statistics version 21 (IBM; Chicago, US).
ResultsUse of EMT. The study included 545 patients; 257 (47.2%) were transported directly to hospital by EMT (group 1), 120 (22.0%) consulted other healthcare professionals before arriving at the hospital (group 2), and 168 (30.8%) arrived at hospital by other means (group 3). In group 2, 67% of patients arrived at the hospital by EMT ambulance or patient transport vehicle.
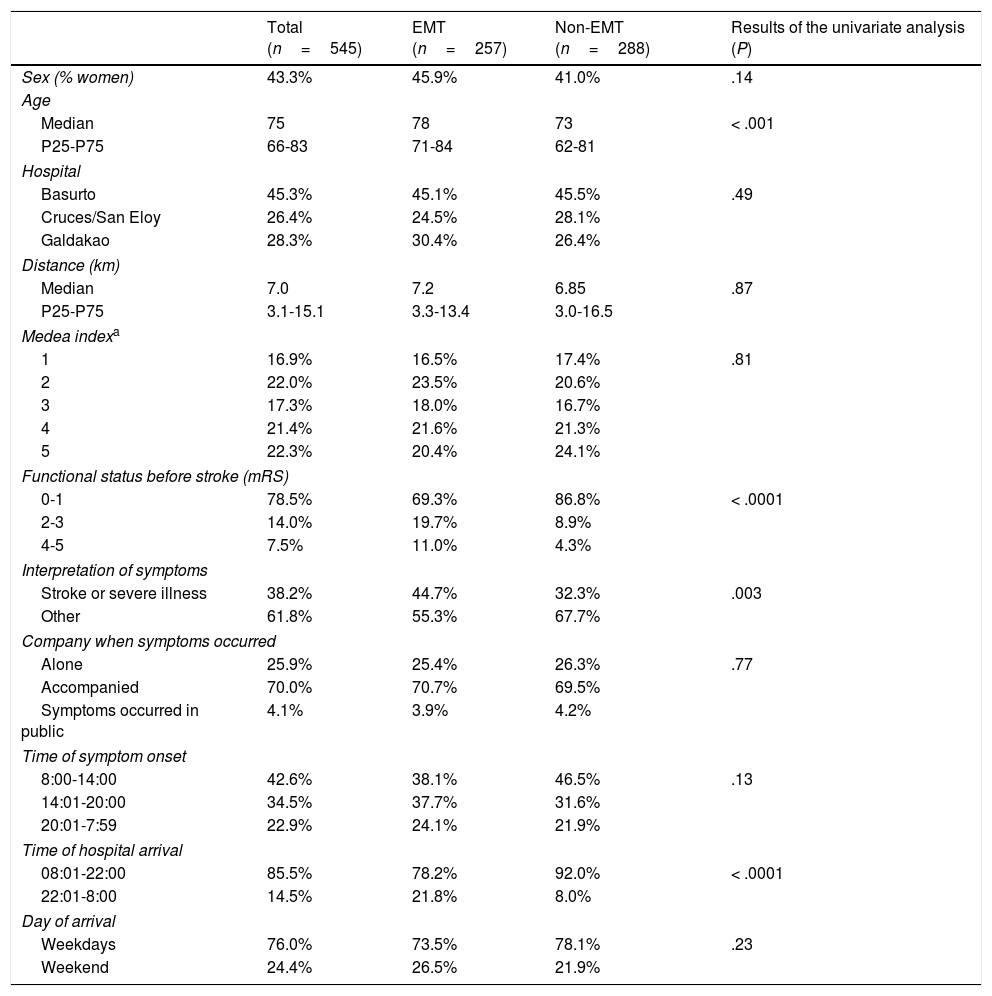
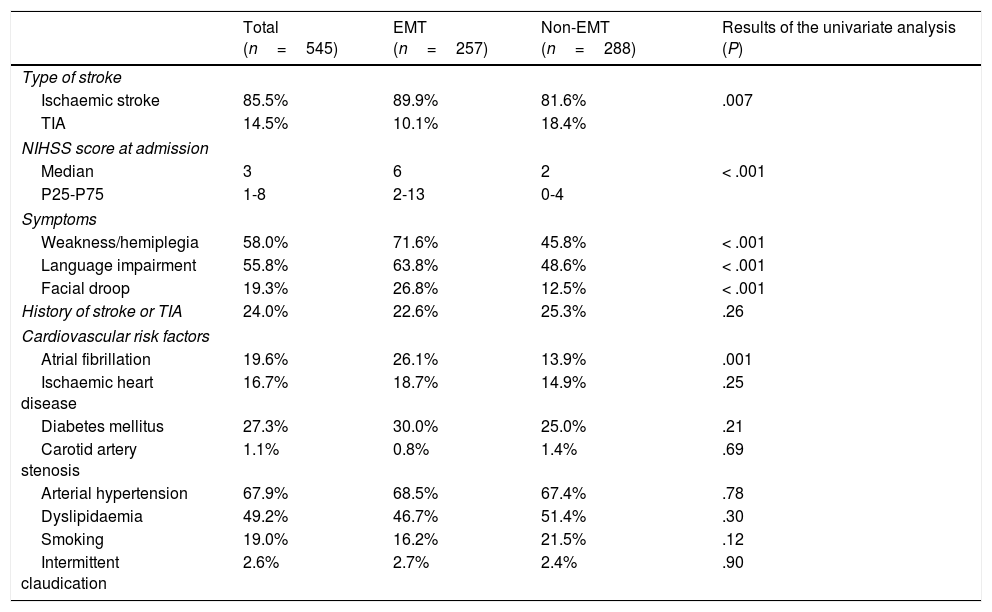
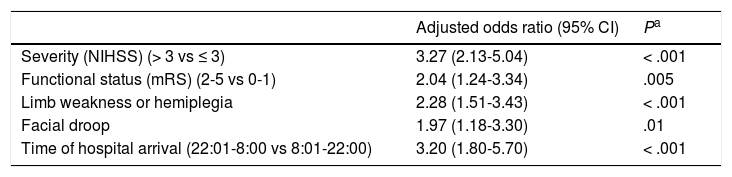
Factors associated with EMT use.Tables 1 and 2 show the results of the study variables and the univariate comparison between categories “EMT” (group 1) and “non-EMT” (groups 2 and 3). Stroke severity, functional status prior to stroke, symptoms of weakness/hemiplegia, facial droop, and arriving at hospital at night were independently associated with use of EMT (Table 3).
Sociodemographic variables and circumstances related to symptom onset. Overall data and comparison between EMT users (transported by the emergency services without the involvement of other healthcare professionals) and non-users (arriving at the hospital by other means or after contacting other healthcare professionals).
| Total (n=545) | EMT (n=257) | Non-EMT (n=288) | Results of the univariate analysis (P) | |
|---|---|---|---|---|
| Sex (% women) | 43.3% | 45.9% | 41.0% | .14 |
| Age | ||||
| Median | 75 | 78 | 73 | < .001 |
| P25-P75 | 66-83 | 71-84 | 62-81 | |
| Hospital | ||||
| Basurto | 45.3% | 45.1% | 45.5% | .49 |
| Cruces/San Eloy | 26.4% | 24.5% | 28.1% | |
| Galdakao | 28.3% | 30.4% | 26.4% | |
| Distance (km) | ||||
| Median | 7.0 | 7.2 | 6.85 | .87 |
| P25-P75 | 3.1-15.1 | 3.3-13.4 | 3.0-16.5 | |
| Medea indexa | ||||
| 1 | 16.9% | 16.5% | 17.4% | .81 |
| 2 | 22.0% | 23.5% | 20.6% | |
| 3 | 17.3% | 18.0% | 16.7% | |
| 4 | 21.4% | 21.6% | 21.3% | |
| 5 | 22.3% | 20.4% | 24.1% | |
| Functional status before stroke (mRS) | ||||
| 0-1 | 78.5% | 69.3% | 86.8% | < .0001 |
| 2-3 | 14.0% | 19.7% | 8.9% | |
| 4-5 | 7.5% | 11.0% | 4.3% | |
| Interpretation of symptoms | ||||
| Stroke or severe illness | 38.2% | 44.7% | 32.3% | .003 |
| Other | 61.8% | 55.3% | 67.7% | |
| Company when symptoms occurred | ||||
| Alone | 25.9% | 25.4% | 26.3% | .77 |
| Accompanied | 70.0% | 70.7% | 69.5% | |
| Symptoms occurred in public | 4.1% | 3.9% | 4.2% | |
| Time of symptom onset | ||||
| 8:00-14:00 | 42.6% | 38.1% | 46.5% | .13 |
| 14:01-20:00 | 34.5% | 37.7% | 31.6% | |
| 20:01-7:59 | 22.9% | 24.1% | 21.9% | |
| Time of hospital arrival | ||||
| 08:01-22:00 | 85.5% | 78.2% | 92.0% | < .0001 |
| 22:01-8:00 | 14.5% | 21.8% | 8.0% | |
| Day of arrival | ||||
| Weekdays | 76.0% | 73.5% | 78.1% | .23 |
| Weekend | 24.4% | 26.5% | 21.9% | |
Stroke characteristics and medical history. Overall data and comparison between EMT users (transported by the emergency services without the involvement of other healthcare professionals) and non-users (arriving at the hospital by other means or after contacting other healthcare professionals).
| Total (n=545) | EMT (n=257) | Non-EMT (n=288) | Results of the univariate analysis (P) | |
|---|---|---|---|---|
| Type of stroke | ||||
| Ischaemic stroke | 85.5% | 89.9% | 81.6% | .007 |
| TIA | 14.5% | 10.1% | 18.4% | |
| NIHSS score at admission | ||||
| Median | 3 | 6 | 2 | < .001 |
| P25-P75 | 1-8 | 2-13 | 0-4 | |
| Symptoms | ||||
| Weakness/hemiplegia | 58.0% | 71.6% | 45.8% | < .001 |
| Language impairment | 55.8% | 63.8% | 48.6% | < .001 |
| Facial droop | 19.3% | 26.8% | 12.5% | < .001 |
| History of stroke or TIA | 24.0% | 22.6% | 25.3% | .26 |
| Cardiovascular risk factors | ||||
| Atrial fibrillation | 19.6% | 26.1% | 13.9% | .001 |
| Ischaemic heart disease | 16.7% | 18.7% | 14.9% | .25 |
| Diabetes mellitus | 27.3% | 30.0% | 25.0% | .21 |
| Carotid artery stenosis | 1.1% | 0.8% | 1.4% | .69 |
| Arterial hypertension | 67.9% | 68.5% | 67.4% | .78 |
| Dyslipidaemia | 49.2% | 46.7% | 51.4% | .30 |
| Smoking | 19.0% | 16.2% | 21.5% | .12 |
| Intermittent claudication | 2.6% | 2.7% | 2.4% | .90 |
EMT: emergency medical transport; NIHSS: National Institutes of Health Stroke Scale; TIA: transient ischaemic attack.
Factors independently associated with use of emergency medical transport.
| Adjusted odds ratio (95% CI) | Pa | |
|---|---|---|
| Severity (NIHSS) (> 3 vs ≤ 3) | 3.27 (2.13-5.04) | < .001 |
| Functional status (mRS) (2-5 vs 0-1) | 2.04 (1.24-3.34) | .005 |
| Limb weakness or hemiplegia | 2.28 (1.51-3.43) | < .001 |
| Facial droop | 1.97 (1.18-3.30) | .01 |
| Time of hospital arrival (22:01-8:00 vs 8:01-22:00) | 3.20 (1.80-5.70) | < .001 |
Adjusted for age, type of stroke, language impairment, atrial fibrillation, and recognition of symptoms as stroke or severe illness.
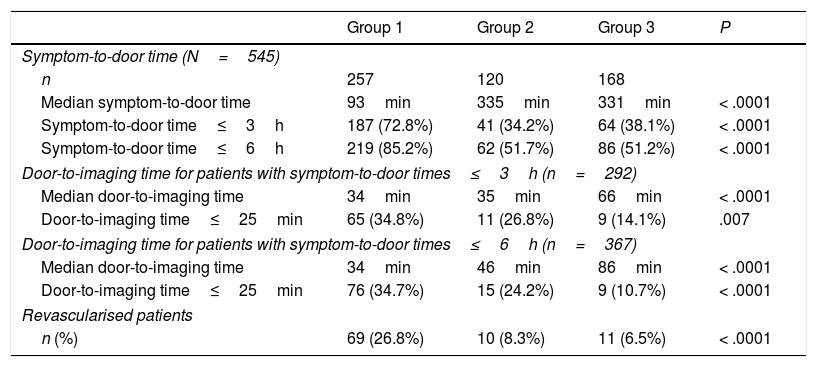
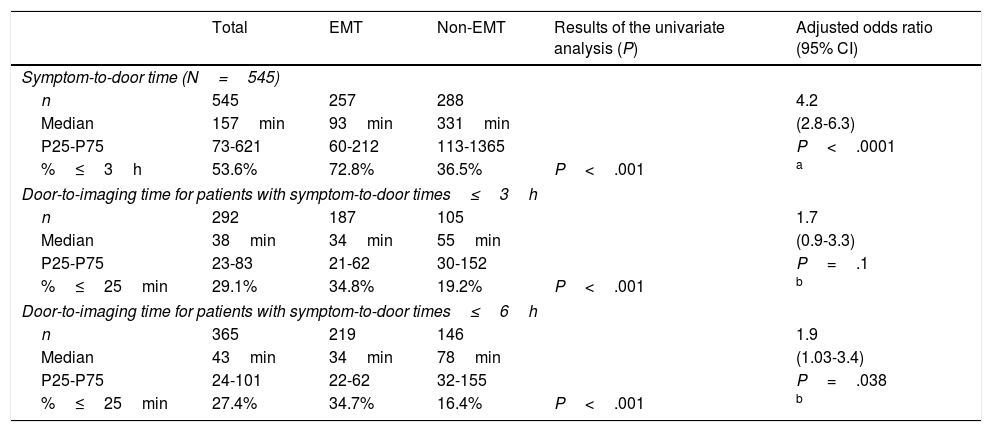
Time to care. In group 1, emergency calls were made within 90minutes of symptom onset in 67% of cases (Me, 46min; P25, 16; P75, 154). The median time between the telephone call and arrival at the hospital was 41minutes (P25, 34; P75, 52). Patients arrived at hospital within 3hours of symptom onset in 53.6% of cases and within 6hours in 67%. The median door-to-imaging time for the total sample was 60minutes (P25, 30; P75, 145). Table 4 shows the delays and the percentages of patients undergoing revascularisation according to transport type. A total of 90 patients underwent revascularisation, with a frequency 3.7 times higher in the EMT group than in the non-EMT group. Intravenous thrombolysis was performed in 43.3% of these patients, mechanical thrombectomy in 37.8%, and a combination of both in 18.9%. Table 5 shows the differences in time to care between EMT users and non-users; both symptom-to-door time and door-to-imaging time were shorter in EMT users than in non-users. Delays in time to care were not significantly different between centres; the variable “hospital” was therefore not included in the multivariate analysis. In the multivariate analysis, use of EMT was found to be independently associated with arrival at hospital within 3hours of symptom onset. Among patients arriving at hospital within the first 3hours, neuroimaging studies were more frequently performed within 25minutes in EMT users; however, this association was not found to be significant after adjusting for other variables. The association was statistically significant in patients with symptom-to-door times≤6hours (adjusted OR=1.8 [95% CI, 1.03-3.4]). Stroke severity (NIHSS score) was the variable with the greatest impact on door-to-imaging time (adjusted OR=6.9 [95% CI, 3.6-13.5]).
Symptom-to-door and door-to-imaging times and number and proportion of revascularised patients according to transport type.
| Group 1 | Group 2 | Group 3 | P | |
|---|---|---|---|---|
| Symptom-to-door time (N=545) | ||||
| n | 257 | 120 | 168 | |
| Median symptom-to-door time | 93min | 335min | 331min | < .0001 |
| Symptom-to-door time≤3h | 187 (72.8%) | 41 (34.2%) | 64 (38.1%) | < .0001 |
| Symptom-to-door time≤6h | 219 (85.2%) | 62 (51.7%) | 86 (51.2%) | < .0001 |
| Door-to-imaging time for patients with symptom-to-door times≤3h (n=292) | ||||
| Median door-to-imaging time | 34min | 35min | 66min | < .0001 |
| Door-to-imaging time≤25min | 65 (34.8%) | 11 (26.8%) | 9 (14.1%) | .007 |
| Door-to-imaging time for patients with symptom-to-door times≤6h (n=367) | ||||
| Median door-to-imaging time | 34min | 46min | 86min | < .0001 |
| Door-to-imaging time≤25min | 76 (34.7%) | 15 (24.2%) | 9 (10.7%) | < .0001 |
| Revascularised patients | ||||
| n (%) | 69 (26.8%) | 10 (8.3%) | 11 (6.5%) | < .0001 |
Group 1: patients attended by emergency service professionals exclusively before hospital arrival. Group 2: patients attended by other healthcare professionals before hospital arrival. Group 3: patients not attended by any healthcare professional before hospital arrival.
Times to care according to use of emergency medical transport. Univariate comparison and adjusted odds ratio for emergency medical transport (EMT vs non-EMT).
| Total | EMT | Non-EMT | Results of the univariate analysis (P) | Adjusted odds ratio (95% CI) | |
|---|---|---|---|---|---|
| Symptom-to-door time (N=545) | |||||
| n | 545 | 257 | 288 | 4.2 | |
| Median | 157min | 93min | 331min | (2.8-6.3) | |
| P25-P75 | 73-621 | 60-212 | 113-1365 | P<.0001 | |
| %≤3h | 53.6% | 72.8% | 36.5% | P<.001 | a |
| Door-to-imaging time for patients with symptom-to-door times≤3h | |||||
| n | 292 | 187 | 105 | 1.7 | |
| Median | 38min | 34min | 55min | (0.9-3.3) | |
| P25-P75 | 23-83 | 21-62 | 30-152 | P=.1 | |
| %≤25min | 29.1% | 34.8% | 19.2% | P<.001 | b |
| Door-to-imaging time for patients with symptom-to-door times≤6h | |||||
| n | 365 | 219 | 146 | 1.9 | |
| Median | 43min | 34min | 78min | (1.03-3.4) | |
| P25-P75 | 24-101 | 22-62 | 32-155 | P=.038 | |
| %≤25min | 27.4% | 34.7% | 16.4% | P<.001 | b |
95% CI: 95% confidence interval; EMT: emergency medical transport.
Ten patients in group 2 underwent revascularisation; 9 of these had been transported to hospital by an EMT ambulance or patient transport vehicle.
Prehospital code stroke was activated for 133 of the 307 patients transported by the emergency services (43.3%). No difference was found in time from the emergency telephone call to hospital arrival between patients with or without prehospital code stroke activation. Neuroimaging studies were performed within 25minutes of arrival in 38% of the patients for whom prehospital code stroke was activated and 24% of the patients without prehospital code stroke activation (P=.005). Revascularisation was performed in 36.1% of the patients for whom prehospital code stroke was activated, compared to 16.7% of those without code stroke activation (P<.001).
DiscussionOnly half of the patients admitted due to stroke in our setting were transported to hospital by EMT; this is a low proportion considering the rates of EMT use reported in other studies (50%-70%).9–11,14,15,17,18,22–24 Our results show a direct association between stroke severity and use of emergency services; this is consistent with the findings of other studies.11,17,20,32 EMT users are usually older and have poorer functional status before stroke; this poorer health status and greater experience with healthcare services may have contributed to a better reaction to stroke. Patients not using EMT, in contrast, tend to be younger and healthier; this should be taken into account for educational programmes.
Patients recognising their symptoms as stroke or suspecting a severe illness more frequently called the emergency services, although the percentage was low; inadequate response despite recognising stroke has been reported by other authors.8,12,32
As reported in previous studies,11,18,24,33–36 history of stroke was not associated with greater use of EMT; this suggests ineffective health education following the first stroke. Hospitalisation following stroke should also aim to teach these patients and their caregivers to react appropriately in the event of a recurrence.37
Numerous studies have identified EMT transportation as one of the factors most strongly associated with shorter symptom-to-door and door-to-imaging times and higher revascularisation rates.8–20 In our study, use of EMT was strongly associated with hospital arrival within 3hours of symptom onset. Unlike other studies,11,13 we found no clear correlation between transport type and door-to-imaging time after adjusting for stroke severity. Door-to-imaging times were similar between groups 1 and 2 (Table 4); differences with group 3 were more marked. In group 2, 67% of patients were transported by either an EMT ambulance or a patient transport vehicle. The factor of arriving at the hospital with a healthcare professional and probably suspicion of stroke is partially present in the “non-EMT” category, which may have an impact on the differences in hospital times to care between EMT users and non-users. This may be explained by the strong impact of stroke severity on door-to-imaging time: once the patient arrives at the hospital, stroke severity is the most decisive factor in patient management and times to care. In any case, current guidelines suggest that performing a neuroimaging study within 25minutes of hospital arrival is associated with considerable improvements in patient health status.37
Our univariate analysis showed a correlation between revascularisation rate and transport type; the frequency of revascularisation was considerably higher in the EMT group (26.8% vs 7.3%). Given the low rate of revascularisation in our sample, this variable was not included in the multivariate analysis.
As in other studies,25–28,38 prehospital code stroke activation was associated with shorter door-to-imaging times and higher revascularisation rates. However, efforts should be made to improve prehospital code stroke response times, as only 38% of patients underwent neuroimaging studies within 25minutes of hospital admission.
Symptom-to-door time was less than 3hours in 53.6% of cases; this time frame is shorter than those reported by most studies.10–12,14,18,32,39–41 The median door-to-imaging time for all patients (60min) is also among the lowest reported.12–14,39
Our results coincide with previous studies observing that contact with the primary care physician by patients or their companions contributes to prehospital delays.8,10,15,32,33,36,42–44 In these cases, delays may be attributable to the patient, for taking too long to seek assistance; to the primary care physician; or to organisational issues, in cases of failure to recognise the emergency.45 The fact that 33% of the patients in group 2 travelled to hospital in private vehicles underscores the need for patient education.
Our study has some limitations. First, although we followed a strict patient recruitment procedure, we are aware that a small percentage of patients admitted due to stroke were not included in our sample; these were probably patients with mild stroke who were hospitalised for one or 2 days. Our study focuses on hospitalised patients; therefore, it does not include data on patients who visited the emergency department but were not admitted to hospital. In any case, we verified that the proportion of EMT users was similar in admitted and non-admitted patients. Patients who could not be stabilised were excluded from the study due to the difficulty obtaining informed consent. These were the patients most severely affected by stroke and the most frequent users of EMT. Excluding these patients may have led to an underestimation of EMT use. Although the risk factors analysed were not found to be significantly associated with EMT use (except for atrial fibrillation), other diseases not included in our analysis may have acted as confounding factors.
Our results confirm that contacting the emergency services is the best option when stroke symptoms are detected. There is a need to develop effective patient education programmes based on our knowledge of those patients who are less likely to use EMT. In-hospital stroke management should be improved to reduce times to care, in line with current recommendations. Our results provide a solid basis for evaluating the results of future interventions.
FundingThis study has received no public or private funding.
Conflicts of interestThe authors of this study have no conflicts of interest to declare.
The authors wish to thank all healthcare and emergency services professionals who collaborated in and supported this study.
Please cite this article as: Olascoaga Arrate A, Freijo Guerrero MM, Fernández Maiztegi C, Azkune Calle I, Silvariño Fernández R, Fernández Rodríguez M, et al. Utilización de transporte sanitario urgente por los pacientes con ictus isquémico e impacto en los tiempos de atención. Neurología. 2019;34:80–88.
This study has not been presented in any form at the Annual Meeting of the SEN or at any other meeting or congress.