Idiopathic intracranial hypertension (IIH) is a disease typically manifesting in young female patients with obesity. Obesity is thought to play a central role in its pathophysiology. Treatment is classically based on weight loss, diuretics, and cerebrospinal fluid (CSF) shunting in refractory cases. Bariatric surgery has been proposed for the treatment of IIH associated with obesity, although the neurological literature includes scarce evidence on the subject. We present a case of IIH associated with obesity which was refractory to conventional treatment, and the clinical response after bariatric surgery.
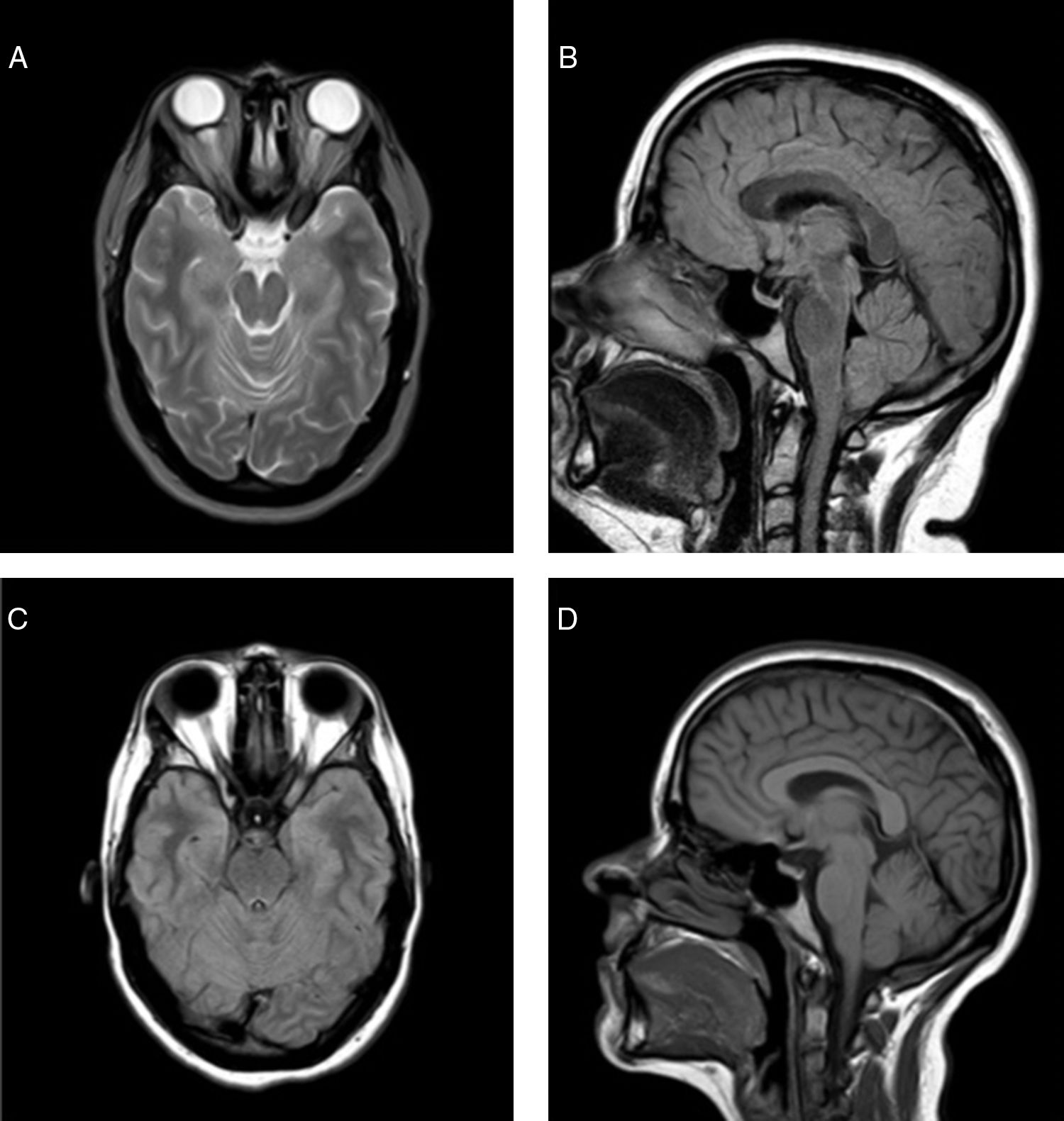
Our patient was a 23-year-old woman with a history of morbid or class III obesity, (BMI: 42.7kg/m2 [weight: 112kg; height: 162cm]), dyslipidaemia, smoking, and treatment with oral contraceptives. She presented a 3-week history of oppressive frontal headache, amaurosis fugax in the right eye, binocular diplopia with bilateral paralysis of the sixth cranial nerve, and bilateral papilloedema. We performed a brain CT scan and CT angiography, with no abnormal findings. The brain MRI scan showed a dural ectasia of the optic nerves, a partially empty sella turcica, and a mild herniation of the cerebellar tonsils which we suspected was secondary to intracranial hypertension and not a type 1 Arnold-Chiari malformation (Fig. 1). Lumbar puncture opening pressure was 39cm H2O; CSF analysis results were normal. Visual acuity, visual field assessment, and optical coherence tomography yielded normal results. The patient was diagnosed with IIH. Treatment with oral contraceptives was suspended and treatment was started with acetazolamide at 750mg/24hours, as well as dietary and lifestyle changes. The patient initially presented a favourable response: migraine episodes reduced in frequency, and papilloedema and bilateral paralysis of the sixth cranial nerve disappeared.
Baseline brain MRI: (A) Axial T2-weighted sequence, showing ectasia of the optical nerve sheath, with prominence of both optic discs with signs of IIH. (B) Sagittal FLAIR sequence, showing the partially empty sella turcica. The cerebellar tonsils are mildly herniated, reaching the level of the foramen magnum. Brain MR image obtained 6 months after bariatric surgery. (C) Axial FLAIR sequence, showing resolution of the orbital findings. (D) Sagittal T1-weighted sequence, showing slight retraction of cerebellar tonsils in comparison with the previous study.
However, her condition progressively worsened, and she had to be hospitalised twice and visit the emergency department numerous times due to refractory headache, with onset of a new bilateral papilloedema with preserved visual acuity, requiring 2 lumbar taps; the second tap revealed an opening pressure of 47cm H2O and resulted in no clinical improvement. She was then referred to neurosurgery for assessment of eligibility for CSF shunting. At 10 months after diagnosis, she had lost 12kg and presented a BMI of 38.1kg/m2, and was therefore assessed by the endocrinology and nutrition department's high risk obesity unit; bariatric surgery was indicated and the neurosurgical treatment was postponed. She underwent a laparoscopic sleeve gastrectomy without complications. At 3 months after bariatric surgery, the patient had lost an additional 16kg, with a BMI of 32kg/m2, showing clear signs of headache improvement, normal eye fundus, normal visual acuity, and improvement of the signs of intracranial hypertension in the follow-up MRI scan (Fig. 1). We therefore ruled out neurosurgical treatment. IIH resolution persisted after 12 months of follow-up.
Since 1986, several case reports and case series of IIH with obesity treated with bariatric surgery have been published, mainly in surgery journals.1–9 A review article by Fridley et al.10 reported a total of 62 cases (class IV evidence) in which signs and symptoms of IIH resolved in 92% of cases, with no significant complications associated with bariatric surgery. Furthermore, 11 cases have been reported in which neurosurgical shunting was unsuccessful and improvement was observed after bariatric surgery.10,11 We did find it striking that these data have had so little impact in the field of neurology, with only 2 articles published.8,12
Weight loss continues to be the most effective treatment for obese patients with IIH. Its pathophysiological mechanism remains unknown. It has been hypothesised that obesity may cause an increase in intra-abdominal pressure, and secondarily intrathoracic pressure, consequently increasing central venous pressure, which would delay venous return and consequently CSF reabsorption.9 Therefore, secretion of pro-inflammatory adipokines and such hormones as leptin by the adipose tissue is believed to play an important role.13
Regarding neurosurgical treatment options, we would like to point out that in cases where IIH is associated with type 1 Arnold-Chiari malformation, CSF lumboperitoneal shunt is not recommended, since it may even aggravate the condition; ventriculoperitoneal shunt is an alternative option.14
Despite the need for prospective and controlled trials with higher levels of evidence, those published to date suggest that bariatric surgery should be considered in patients with IIH and obesity,15 especially before associated visual loss manifests. Furthermore, researchers suggest including IIH as a criterion for prioritising patients with obesity on bariatric surgery waiting lists, which are long in our setting. In practical terms, multidisciplinary management is recommended, with early referral of these patients to a specialised obesity unit.
Please cite this article as: Pérez-Sánchez JR, Arnoriaga Rodríguez M, Díaz-Otero F, Bretón Lesmes I. Tratamiento de la hipertensión intracraneal idiopática con cirugía bariátrica. Neurología. 2019;34:493–495.
This study was previously presented at the 12th National Congress of the Spanish Society for the Study of Obesity (SEEDO) in 2015, under the title “Bariatric surgery in idiopathic intracranial hypertension: a case report”.