ACTIVLIM is an instrument for the measurement of activity limitations in patients with neuromuscular disorders. The aim of this study is to establish a transcultural adaptation and psychometric validation of the Spanish-language version of ACTIVLIM in a sample of Spanish patients with inherited myopathies.
Patients and methodA Spanish-language version of ACTIVLIM was developed using the translation/back translation method. The questionnaire was administered to 135 patients with inherited myopathies. The psychometric properties of the questionnaire were assessed using the Rasch model. Floor and ceiling effects were estimated. Unidimensionality was evaluated with a principal component analysis of the residuals of the model, and using infit and outfit statistics. We estimated reliability with the person separation reliability index and invariance with differential item functioning. External construct validity was tested through correlation with the Brooke scale, the Vignos scale, the Functional Independence Measure scale, and floor-to-stand time. Test–retest reliability was evaluated with the intraclass correlation coefficient and differential item functioning.
ResultsThe psychometric analysis of the Spanish-language version of ACTIVLIM demonstrated that floor effect was absent, although a modest ceiling effect was identified. The instrument displayed unidimensionality, good internal consistency, external construct validity, and good test–retest reliability.
ConclusionThe Spanish-language version of ACTIVLIM is a valid and reliable measurement instrument for assessing activity limitations in patients with inherited myopathies.
ACTIVLIM es un instrumento de medición de la limitación funcional en pacientes con enfermedades neuromusculares. El objetivo de este estudio es la adaptación transcultural y la validación psicométrica de la versión en castellano del ACTIVLIM en una muestra española de pacientes con miopatías hereditarias.
Pacientes y métodoSe elaboró una versión en castellano del cuestionario ACTIVLM mediante el método de traducción-retrotraducción. El cuestionario obtenido fue cumplimentado por 135 pacientes con miopatías hereditarias. Las propiedades psicométricas del mismo fueron evaluadas mediante el modelo Rasch. Se valoró la adecuación del rango mediante la estimación de efectos techo y suelo; la unidimensionalidad mediante análisis de componentes principales de los residuales del modelo y estadísticos infit y outfit; la fiabilidad mediante el índice de fiabilidad asociado al índice de separación y la invarianza mediante la estimación del funcionamiento diferencial. Asimismo, la validez de constructo se evaluó estimando la correlación con las escalas de Brooke, de Vignos, la medida de independencia funcional y el tiempo de Gowers, y la fiabilidad test-retest mediante el índice de correlación intraclase y con el plot del funcionamiento diferencial del ítem.
ResultadosEl análisis psicométrico de la versión en castellano del ACTIVLIM demostró ausencia de efecto suelo y moderado efecto techo, unidimensionalidad, una buena consistencia interna, validez externa de constructo y buena fiabilidad test-retest.
ConclusiónLa versión en castellano del ACTIVLIM es un instrumento de medición válido y fiable para evaluar las limitaciones en la actividad en pacientes con miopatías hereditarias.
The term neuromuscular disease (NMD) refers to a broad group of diseases characterised by progressive muscle weakness; severity and distribution depend on the specific type of disease.1 Patients with NMDs have difficulties performing activities of daily living.
The World Health Organization International Classification of Functioning, Disability, and Health defines difficulties with these tasks as “activity limitations.”2 Numerous scales have been developed to measure activity limitations in patients with NMDs. These include the Motor Function Measure3; Activity Limitations for Patients with Upper and/or Lower Limb Impairments (ACTIVLIM)4; Capacity (PLAN-Q)5; the Neuromuscular Symptom Score; the gait, stairs, Gowers, chair (GSGC) score; the Walton-Gardner-Medwin Score; and the Adult Ambulatory Neuromuscular Assessment. ACTIVLIM and PLAN-Q are considered to be 2 of the 4 best instruments for measuring activity limitations in patients with NMDs.6 Both scales exclusively assess muscle function3 and include a broad range of activities for evaluating mobility, self-care, and performance of domestic tasks.
ACTIVLIM measures the capacity to perform everyday activities in patients with NMDs. The questionnaire was originally drafted in Dutch and French and validated for use in children and adults using the Rasch model.4 It has good reliability, construct validity, reproducibility, linearity, and unidimensionality, and adequate sensitivity to change.7,8 The scale is available in French, Dutch, and English,7 but no Spanish-language version currently exists. There are 2 options for extending the applicability of ACTIVLIM to Spanish-speaking countries: developing a new instrument, or adapting the existing one.9 In the latter approach, careful translation is needed to maintain the questionnaire's psychometric properties.10
We present the transcultural adaptation of a Spanish-language version of the ACTIVLIM questionnaire and its validation using the Rasch model.
Materials and methodsACTIVLIM questionnaireACTIVLIM is a self-administered questionnaire for patients with NMDs. It includes 22 items (4 are specific to children and 4 to adults) addressing activities of daily living. Patients rate the difficulty of performing a range of activities without technical or human assistance, selecting one of 3 categories (impossible: 0 points; difficult: 1 point; easy: 2 points). Activities for which the patient does not know how to respond are scored as missing data.
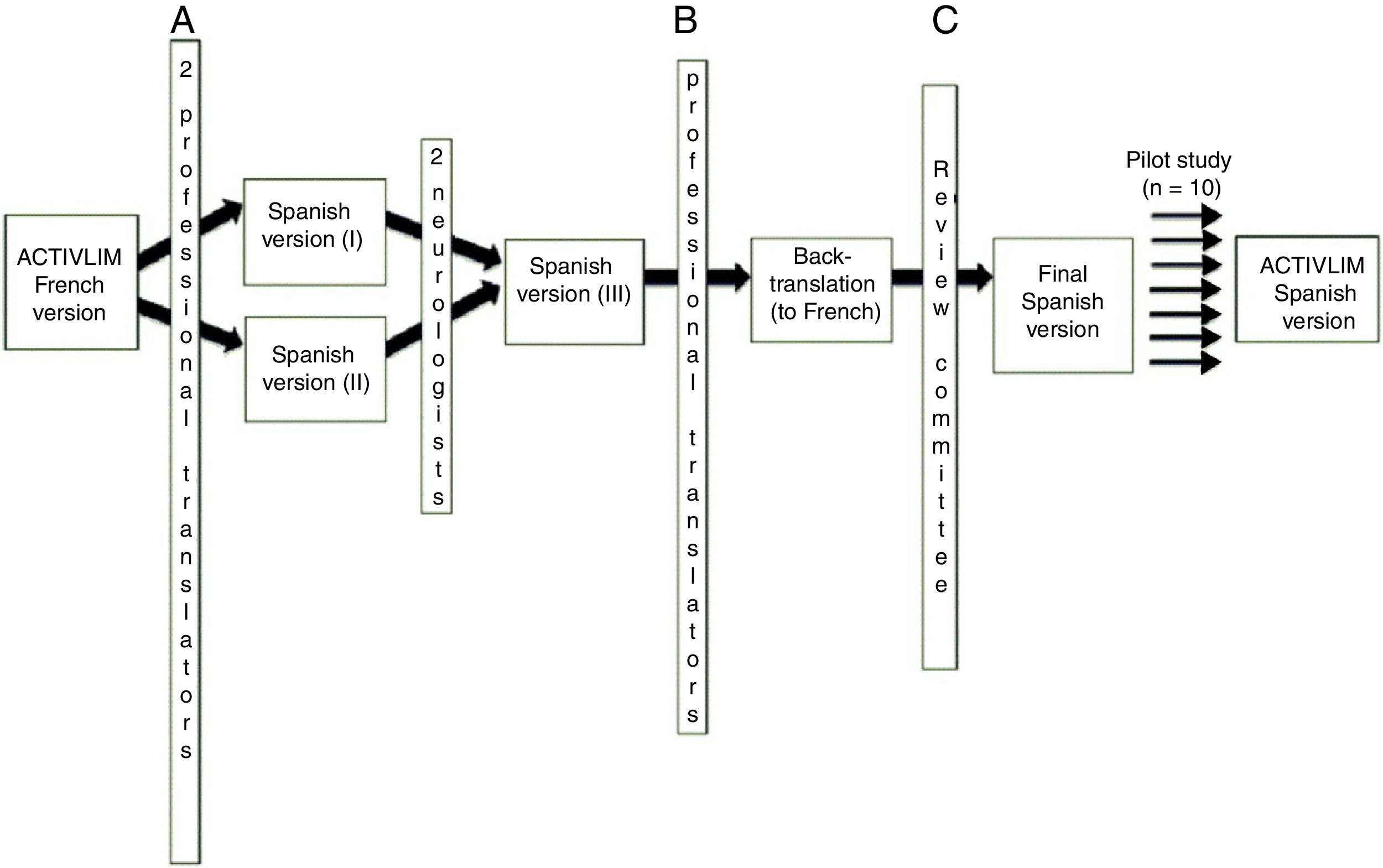
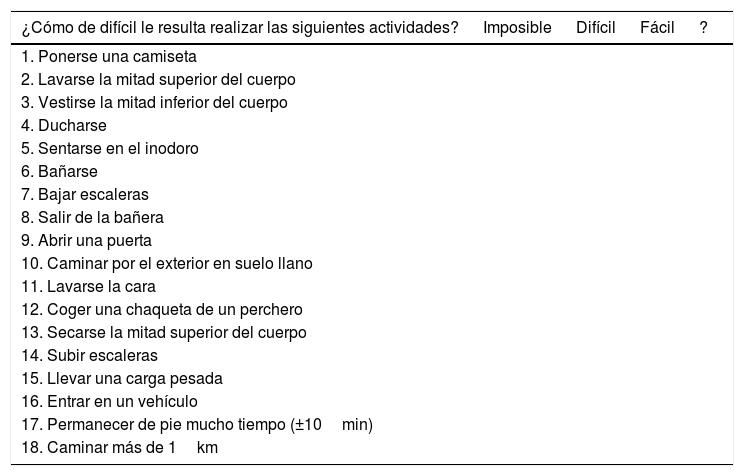
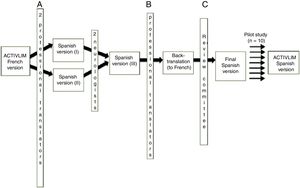
Spanish-language translation and adaptation of the questionnaireThe Spanish-language version of the questionnaire was created by a process of translation-back translation (Fig. 1), in accordance with the standardised guidelines for the transcultural adaptation of quality of life measures.11 To ensure comprehensibility and applicability, we performed a pilot study of the Spanish-language version of the questionnaire in 10 patients with NMDs. Through this process, we produced a final Spanish-language version of the questionnaire (Table 1), subsequently evaluating its psychometric properties. Before preparing the Spanish-language questionnaire, we sought the permission of the author of the original instrument, who also approved our final version.
Translation-back translation process. (A) Native Spanish speakers fluent in French; (B) native French speakers fluent in Spanish; (C) review committee comprising 2 neurologists (one specialising in NMDs) and 3 professional bilingual translators (2 native Spanish speakers and one native French speaker).
Spanish-language version of the ACTIVLIM measure of activity limitations.
| ¿Cómo de difícil le resulta realizar las siguientes actividades? | Imposible | Difícil | Fácil | ? |
|---|---|---|---|---|
| 1. Ponerse una camiseta | ||||
| 2. Lavarse la mitad superior del cuerpo | ||||
| 3. Vestirse la mitad inferior del cuerpo | ||||
| 4. Ducharse | ||||
| 5. Sentarse en el inodoro | ||||
| 6. Bañarse | ||||
| 7. Bajar escaleras | ||||
| 8. Salir de la bañera | ||||
| 9. Abrir una puerta | ||||
| 10. Caminar por el exterior en suelo llano | ||||
| 11. Lavarse la cara | ||||
| 12. Coger una chaqueta de un perchero | ||||
| 13. Secarse la mitad superior del cuerpo | ||||
| 14. Subir escaleras | ||||
| 15. Llevar una carga pesada | ||||
| 16. Entrar en un vehículo | ||||
| 17. Permanecer de pie mucho tiempo (±10min) | ||||
| 18. Caminar más de 1km |
Patients were selected from the registry of hereditary myopathies of Navarre, which contains information on 371 patients with different levels of severity. We excluded patients with other neurological diseases, chronic orthopaedic disorders, systemic diseases, or mental health disorders that may interfere in the assessment.
A total of 168 patients aged ≥16 with NMDs were invited to participate in the study; 135 (80.3%) accepted. After signing consent forms, each patient was assessed individually by the same neurologist at Complejo Hospitalario de Navarra, between November 2016 and June 2017. The assessment included the Brooke scale, the Vignos scale, the Functional Independence Measure, and Gowers time (time taken to rise from the floor). Finally, each patient completed the Spanish-language version of ACTIVLIM. The items on the questionnaire were presented in a random order (10 different orders) to prevent any bias due to systematic repetition of each item. To analyse test–retest reliability, we administered the questionnaire a second time to 64 patients, 3 weeks after the initial evaluation. This study was approved by the clinical research ethics committee of Navarre.
Data analysisSample characteristics are summarised using descriptive statistics. For each item, we evaluated the percentage of the sample for whom data were missing to assess the completeness of the information. To determine whether the range of activity limitations defined by ACTIVLIM was appropriate, we calculated the percentage of the sample scoring the lowest and the highest possible scores (floor/ceiling effect), considering < 10% to signal a small effect, 10%-20% a moderate effect, and >20% a substantial effect.12
The Spanish-language version of ACTIVLIM was validated within the item response theory framework, using the Rasch model.13,14 This model estimates the difficulty of each item and the patient's level of activity on a common linear scale, using the responses given for each item in a probabilistic framework.4,15 We evaluated response category functioning, comparing the threshold between adjacent categories (0=impossible, 1=difficult, 2=easy), which had to be located in ascending order for all items. Thresholds correspond to the level of activity required for a respondent to be more likely to select one category over another. Unidimensionality was evaluated with a principal component analysis (PCA) of the residuals obtained with the Rasch model. Results were considered to demonstrate the absence of unidimensionality if in addition to the first factor there was another factor with an eigenvalue greater than 3.16 Besides the PCA, we calculated infit and outfit mean-squares to evaluate the fit of the model, considering values between 0.5 and 1.5 (both indices) to indicate good fit17 and values <0.33 or >3 to indicate poor fit.
We tested for local dependence by calculating correlations between item residuals. Correlations of > 0.5 may indicate that the response to one item is influenced by the response to another.18 We identified all correlations >0.3 and evaluated their clinical relevance in order to decide whether any item should be removed from the questionnaire. The reliability of the scale was estimated using the person separation index, which estimates the proportion of variance between individuals that is not explained by random error. This statistic is the equivalent to Cronbach's alpha for the Rasch model. Values ≥0.7 indicate that the scale is able to differentiate at least 2 groups of patients, and is generally considered acceptable.19
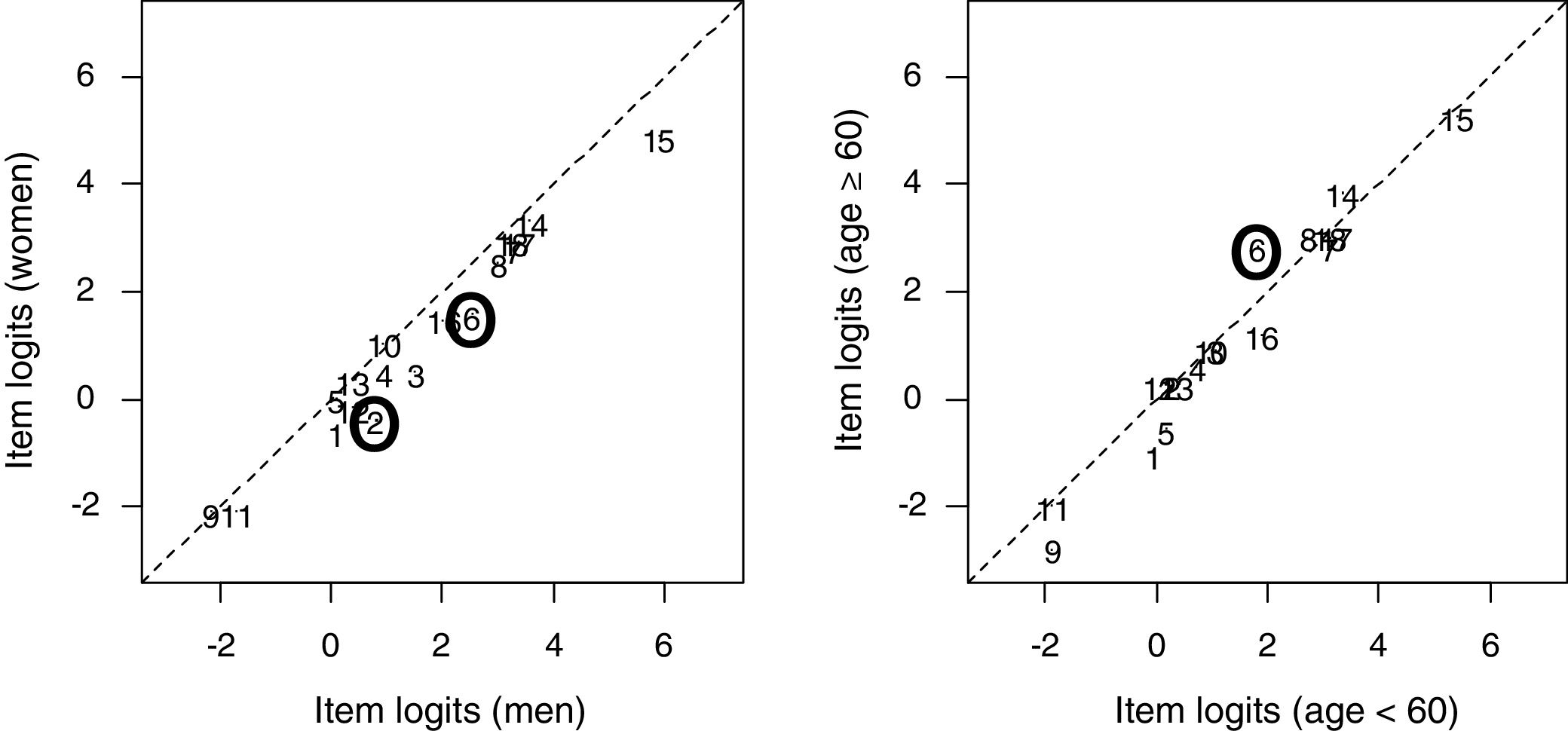
We analysed the invariance of the item difficulty hierarchy by estimating differential item functioning (DIF).20 A scale is considered to display DIF when it presents systematic differences in the likelihood of a given response to an item between groups with the same level of disability but with differences in other variables (eg, age). To analyse DIF, we performed an item-level Wald test21 considering 2 dichotomous factors (sex and age [<60 or ≥60]), displaying results as DIF plots.
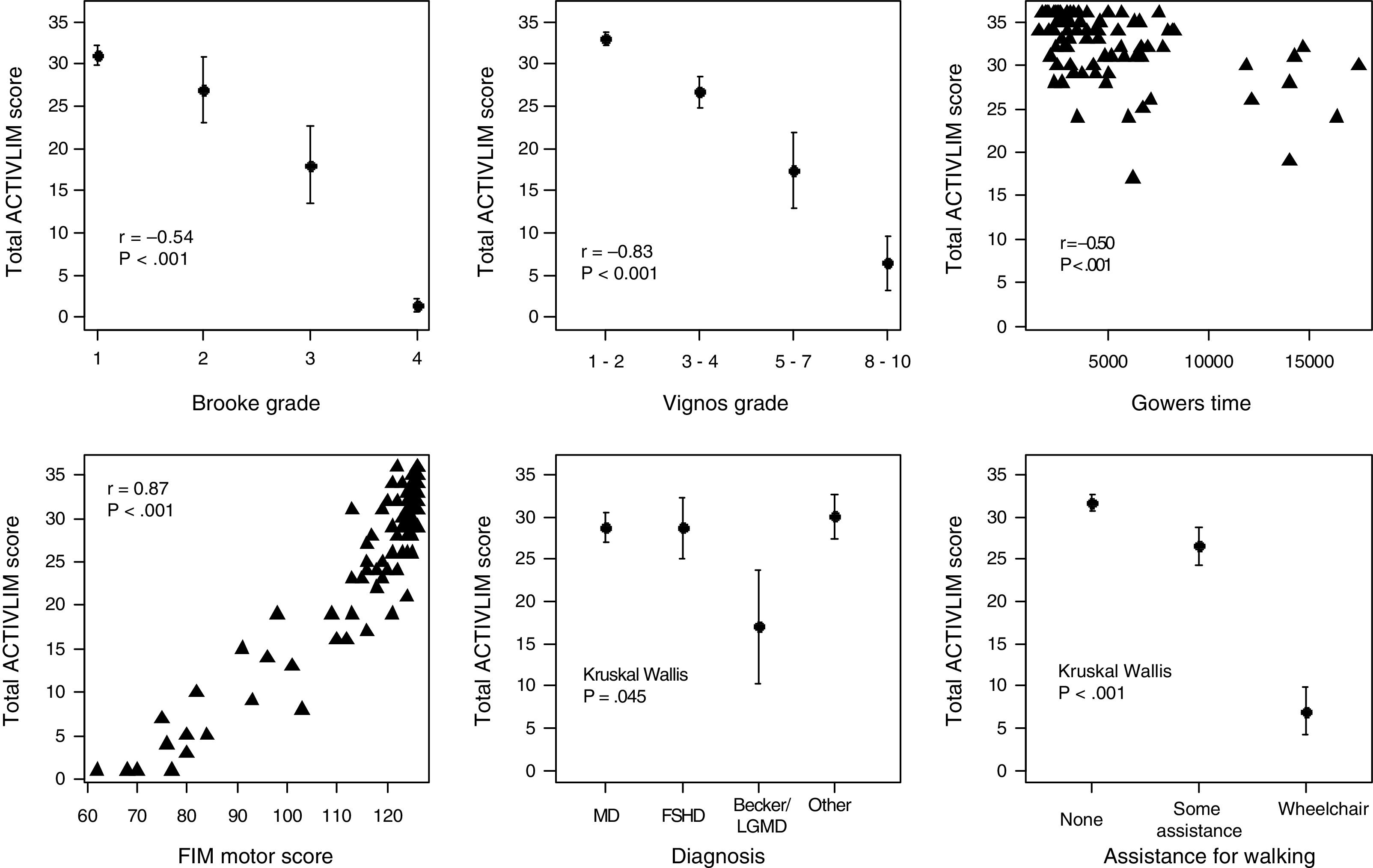
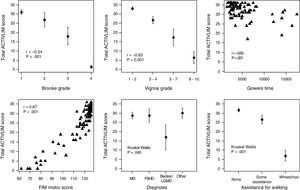
External construct validity was tested by examining the degree of association between scores for ACTIVLIM and the other instruments used: FIM,22 Gowers time,23 and the Vignos24 and Brooke scales.25 We also studied the relationship between ACTIVLIM score and demographic and clinical characteristics (age, sex, and type of NMD) to examine consistency with plausible hypotheses. We hypothesised that an adequate measure of activity limitation should correlate strongly with overall values for the FIM, Gowers time, and the Vignos and Brooke scales. We also expected scores to correlate with age, the need for devices to assist walking, and type of NMD (those with greater proximal involvement would tend to limit activity more than other types); we did not expect to observe a correlation with sex.4 We used the Mann–Whitney or the Kruskal–Wallis test to compare categorical data between groups, and the Spearman correlation coefficient to study associations with continuous variables.
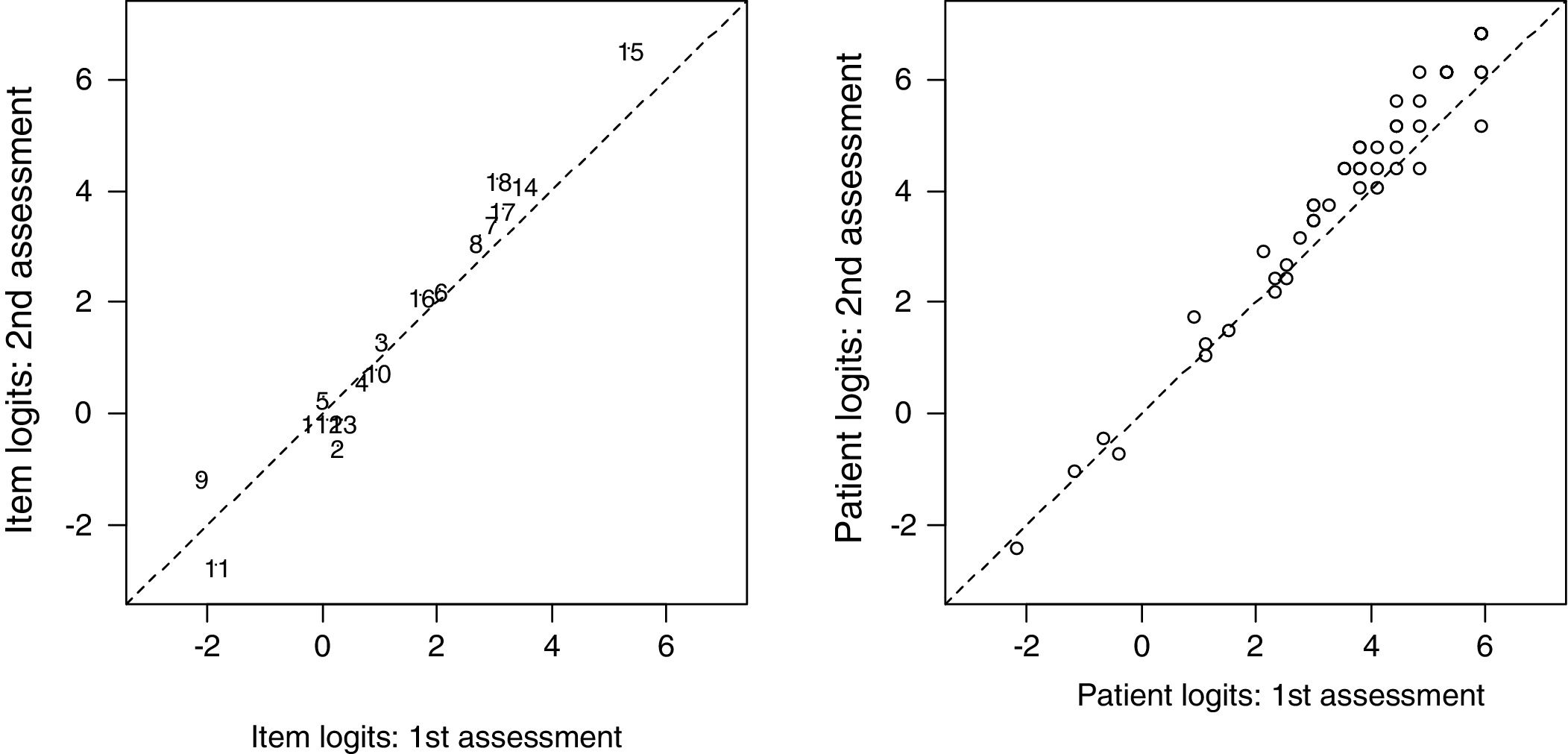
Finally, to analyse whether results were consistent over time, we calculated test–retest reliability for a subgroup of patients, who completed the questionnaire a second time 3 weeks after the initial assessment. This data was analysed with the intraclass correlation coefficient (ICC) and is displayed with DIF plots.
All analyses were performed with the eRm library in R, version 3.1.0.26 It should be noted that the results from this library are not identical to those from the WINSTEPS27 or RUMM 2020 programmes,28 but are a linear transformation of these.
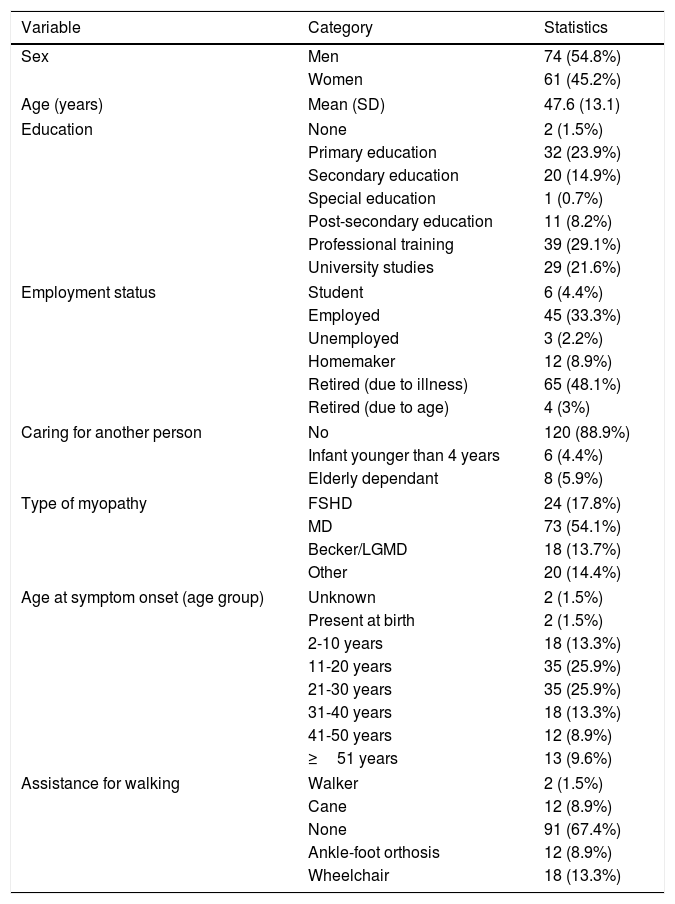
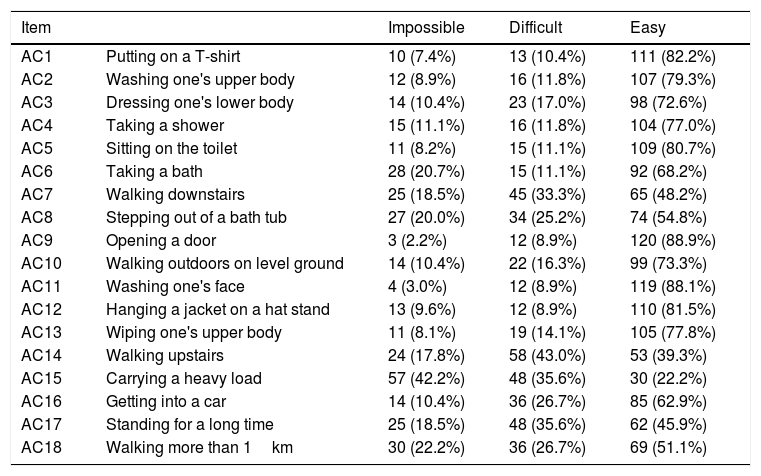
ResultsOur sample's demographic and clinical characteristics are shown in Table 2. Table 3 presents results from the disability assessment (Brooke and Vignos scales, FIM, Gowers time, and ACTIVLIM score). The percentage of missing data for ACTIVLIM items was equal to 0%. No floor effect was observed, whereas 22 patients (16%) scored the maximum of 36 points, suggesting a moderate ceiling effect. Table 4 shows the frequency of the different responses to each item. Five items were considered easy by over 80% of patients, and 2 items (AC9 and AC11) were rated as impossible by fewer than 10% of patients.
Patients’ demographic and clinical characteristics.
| Variable | Category | Statistics |
|---|---|---|
| Sex | Men | 74 (54.8%) |
| Women | 61 (45.2%) | |
| Age (years) | Mean (SD) | 47.6 (13.1) |
| Education | None | 2 (1.5%) |
| Primary education | 32 (23.9%) | |
| Secondary education | 20 (14.9%) | |
| Special education | 1 (0.7%) | |
| Post-secondary education | 11 (8.2%) | |
| Professional training | 39 (29.1%) | |
| University studies | 29 (21.6%) | |
| Employment status | Student | 6 (4.4%) |
| Employed | 45 (33.3%) | |
| Unemployed | 3 (2.2%) | |
| Homemaker | 12 (8.9%) | |
| Retired (due to illness) | 65 (48.1%) | |
| Retired (due to age) | 4 (3%) | |
| Caring for another person | No | 120 (88.9%) |
| Infant younger than 4 years | 6 (4.4%) | |
| Elderly dependant | 8 (5.9%) | |
| Type of myopathy | FSHD | 24 (17.8%) |
| MD | 73 (54.1%) | |
| Becker/LGMD | 18 (13.7%) | |
| Other | 20 (14.4%) | |
| Age at symptom onset (age group) | Unknown | 2 (1.5%) |
| Present at birth | 2 (1.5%) | |
| 2-10 years | 18 (13.3%) | |
| 11-20 years | 35 (25.9%) | |
| 21-30 years | 35 (25.9%) | |
| 31-40 years | 18 (13.3%) | |
| 41-50 years | 12 (8.9%) | |
| ≥51 years | 13 (9.6%) | |
| Assistance for walking | Walker | 2 (1.5%) |
| Cane | 12 (8.9%) | |
| None | 91 (67.4%) | |
| Ankle-foot orthosis | 12 (8.9%) | |
| Wheelchair | 18 (13.3%) | |
FSHD: facioscapulohumeral muscular dystrophy; LGMD: limb-girdle muscular dystrophy; MD: myotonic dystrophy.
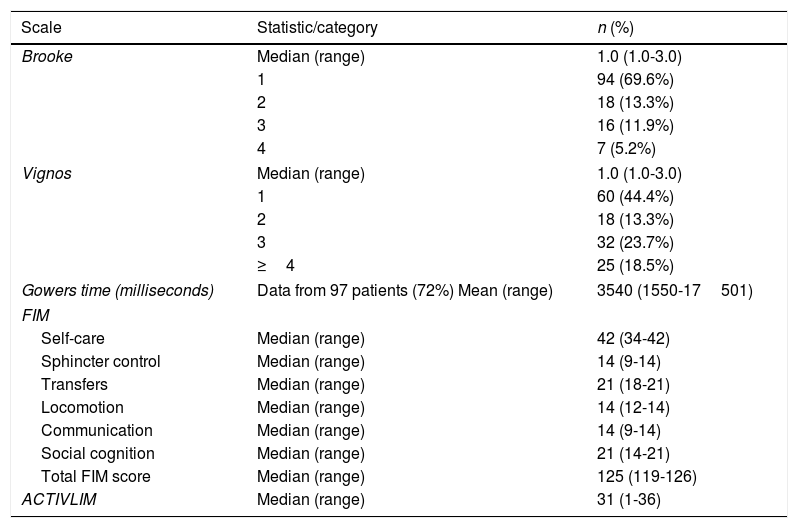
Results from the Brooke scale (upper limbs), Vignos scale (lower limbs), Gowers time, Functional Independence Measure (FIM), and ACTIVLIM.
| Scale | Statistic/category | n (%) |
|---|---|---|
| Brooke | Median (range) | 1.0 (1.0-3.0) |
| 1 | 94 (69.6%) | |
| 2 | 18 (13.3%) | |
| 3 | 16 (11.9%) | |
| 4 | 7 (5.2%) | |
| Vignos | Median (range) | 1.0 (1.0-3.0) |
| 1 | 60 (44.4%) | |
| 2 | 18 (13.3%) | |
| 3 | 32 (23.7%) | |
| ≥4 | 25 (18.5%) | |
| Gowers time (milliseconds) | Data from 97 patients (72%) Mean (range) | 3540 (1550-17501) |
| FIM | ||
| Self-care | Median (range) | 42 (34-42) |
| Sphincter control | Median (range) | 14 (9-14) |
| Transfers | Median (range) | 21 (18-21) |
| Locomotion | Median (range) | 14 (12-14) |
| Communication | Median (range) | 14 (9-14) |
| Social cognition | Median (range) | 21 (14-21) |
| Total FIM score | Median (range) | 125 (119-126) |
| ACTIVLIM | Median (range) | 31 (1-36) |
Number of patients in each category for ACTIVLIM items.
| Item | Impossible | Difficult | Easy | |
|---|---|---|---|---|
| AC1 | Putting on a T-shirt | 10 (7.4%) | 13 (10.4%) | 111 (82.2%) |
| AC2 | Washing one's upper body | 12 (8.9%) | 16 (11.8%) | 107 (79.3%) |
| AC3 | Dressing one's lower body | 14 (10.4%) | 23 (17.0%) | 98 (72.6%) |
| AC4 | Taking a shower | 15 (11.1%) | 16 (11.8%) | 104 (77.0%) |
| AC5 | Sitting on the toilet | 11 (8.2%) | 15 (11.1%) | 109 (80.7%) |
| AC6 | Taking a bath | 28 (20.7%) | 15 (11.1%) | 92 (68.2%) |
| AC7 | Walking downstairs | 25 (18.5%) | 45 (33.3%) | 65 (48.2%) |
| AC8 | Stepping out of a bath tub | 27 (20.0%) | 34 (25.2%) | 74 (54.8%) |
| AC9 | Opening a door | 3 (2.2%) | 12 (8.9%) | 120 (88.9%) |
| AC10 | Walking outdoors on level ground | 14 (10.4%) | 22 (16.3%) | 99 (73.3%) |
| AC11 | Washing one's face | 4 (3.0%) | 12 (8.9%) | 119 (88.1%) |
| AC12 | Hanging a jacket on a hat stand | 13 (9.6%) | 12 (8.9%) | 110 (81.5%) |
| AC13 | Wiping one's upper body | 11 (8.1%) | 19 (14.1%) | 105 (77.8%) |
| AC14 | Walking upstairs | 24 (17.8%) | 58 (43.0%) | 53 (39.3%) |
| AC15 | Carrying a heavy load | 57 (42.2%) | 48 (35.6%) | 30 (22.2%) |
| AC16 | Getting into a car | 14 (10.4%) | 36 (26.7%) | 85 (62.9%) |
| AC17 | Standing for a long time | 25 (18.5%) | 48 (35.6%) | 62 (45.9%) |
| AC18 | Walking more than 1km | 30 (22.2%) | 36 (26.7%) | 69 (51.1%) |
The Rasch analysis of responses to all 18 items showed that no item presented reversed thresholds, indicating proper functioning of the categories for all items. In the PCA, no factor except the first (factor loading of 8.8) had a factor loading >3, indicating unidimensionality.
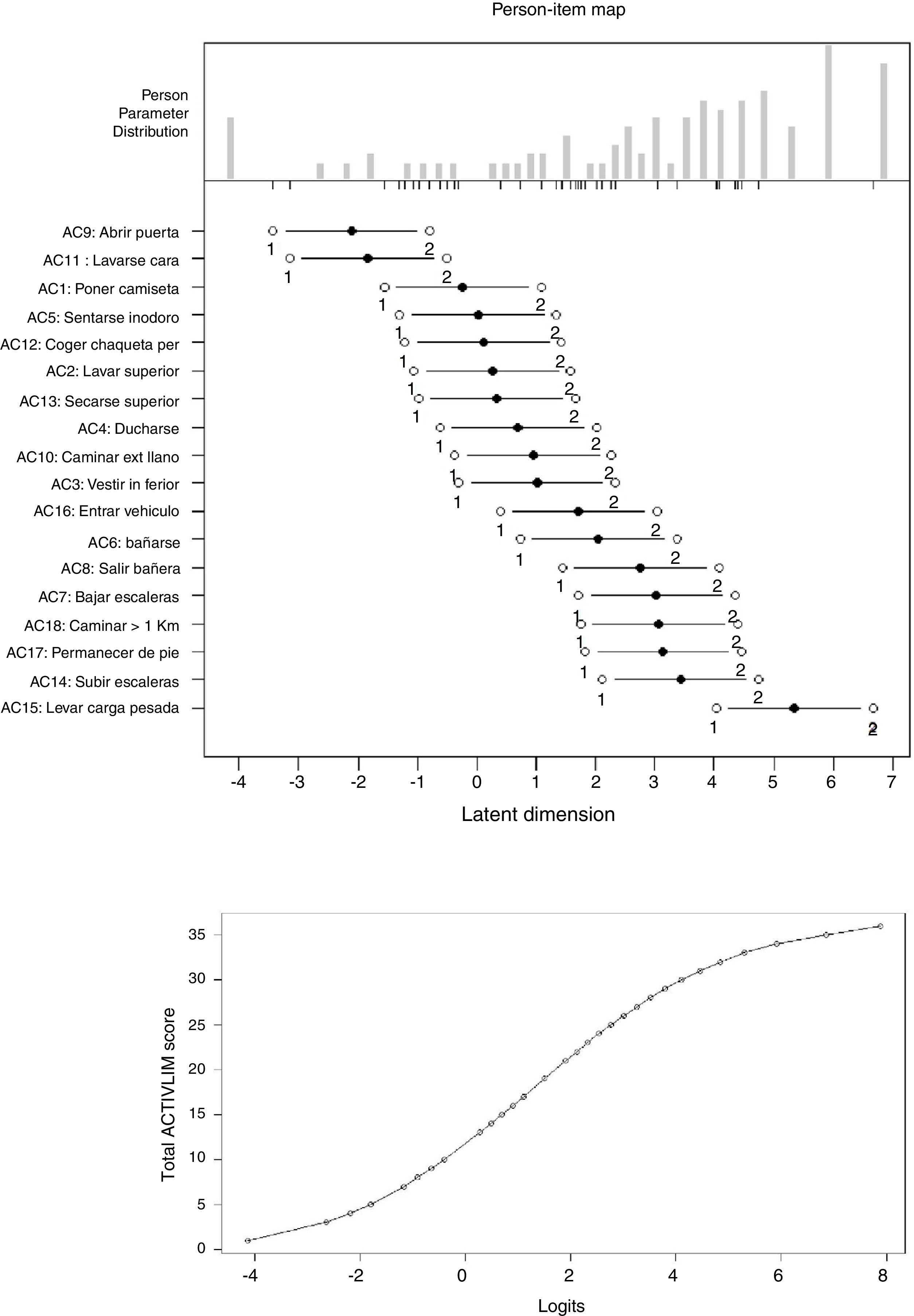
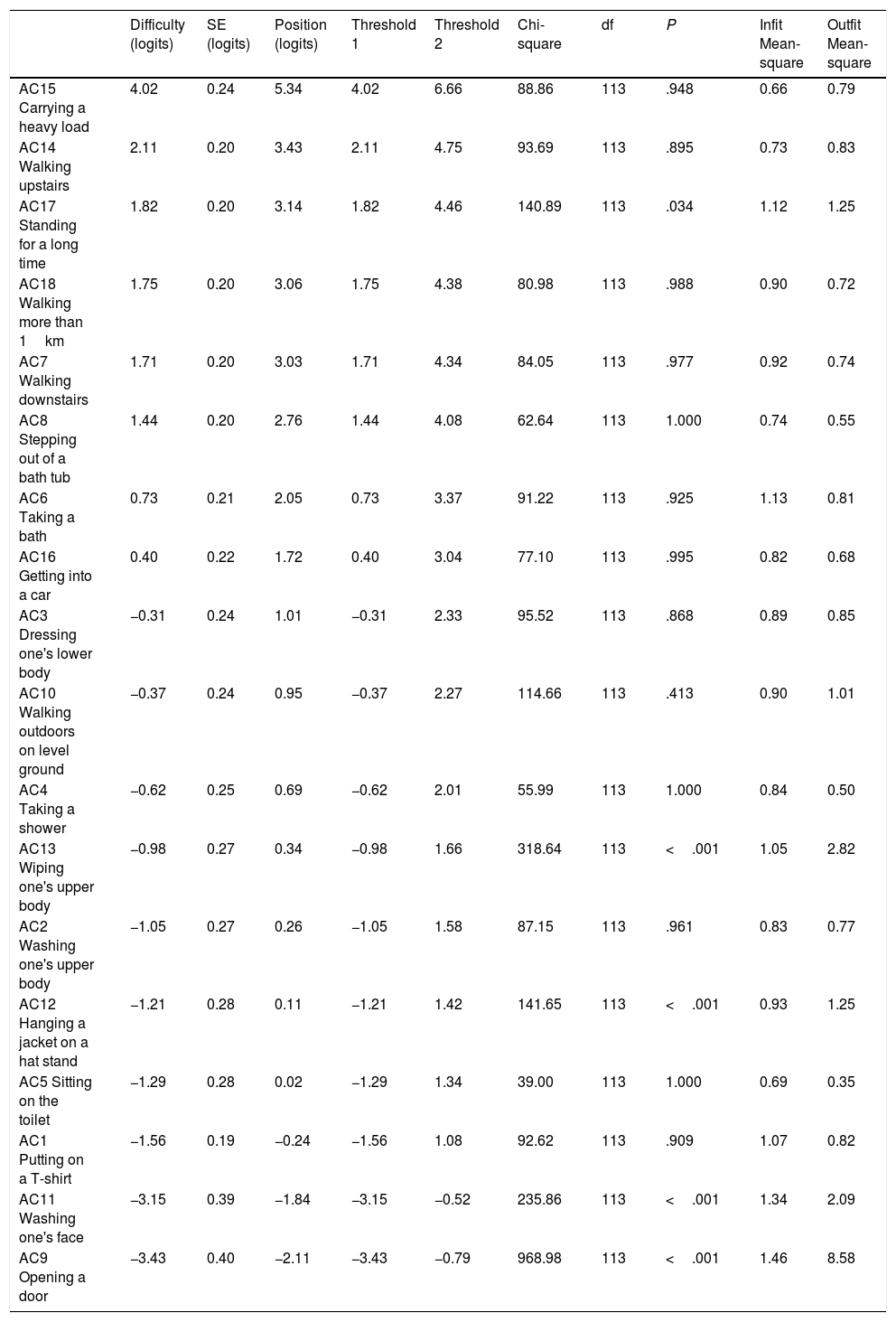
The calibration of the 18 ACTIVLIM items is shown in Table 5. Items are listed (top to bottom) in decreasing order of difficulty (mean difficulty: 0.0 logits; range, −3.4 to 4.0), with higher logit values indicating greater difficulty. The table also shows the standard error (mean: 0.25 logits; range, 0.19-0.40) and infit and outfit values. Item AC9 (opening a door) is the only item with outfit mean-square greater than 3, indicating poor fit. Taking into account the results of the PCA and the infit and outfit statistics, which were acceptable for all items except AC9 (for which the instability may be explained by the fact that only 3 patients rated the item impossible), we may conclude that the items define a unidimensional scale and that the fit of the model is good. Fig. 2 shows the person-item map for the difficulty of ACTIVLIM items; this may be used to compare the range and position of the distribution of items and patients (centre and top part of the panel, respectively). For example, rating item AC1 (putting on a T-shirt) as easy would require 1.08 logits, whereas any patient with a measure less than −1.56 logits could not complete this task. While the most difficult item (AC15 [carrying a heavy load]) was rated as easy by 25% of respondents, only 4% of patients had less capacity than that required to perform the easiest item (AC9 [opening a door]). The lower panel shows the functional relationship used to convert the ordinal total score into a linear activity measure. While a quasi-linear relationship is apparent in the central part of the graph, a single point increase in the total score represents a great difference at both extremes.
Calibration of the ACTIVLIM item difficulty hierarchy, and goodness of fit parameters.
| Difficulty (logits) | SE (logits) | Position (logits) | Threshold 1 | Threshold 2 | Chi-square | df | P | Infit Mean-square | Outfit Mean-square | |
|---|---|---|---|---|---|---|---|---|---|---|
| AC15 Carrying a heavy load | 4.02 | 0.24 | 5.34 | 4.02 | 6.66 | 88.86 | 113 | .948 | 0.66 | 0.79 |
| AC14 Walking upstairs | 2.11 | 0.20 | 3.43 | 2.11 | 4.75 | 93.69 | 113 | .895 | 0.73 | 0.83 |
| AC17 Standing for a long time | 1.82 | 0.20 | 3.14 | 1.82 | 4.46 | 140.89 | 113 | .034 | 1.12 | 1.25 |
| AC18 Walking more than 1km | 1.75 | 0.20 | 3.06 | 1.75 | 4.38 | 80.98 | 113 | .988 | 0.90 | 0.72 |
| AC7 Walking downstairs | 1.71 | 0.20 | 3.03 | 1.71 | 4.34 | 84.05 | 113 | .977 | 0.92 | 0.74 |
| AC8 Stepping out of a bath tub | 1.44 | 0.20 | 2.76 | 1.44 | 4.08 | 62.64 | 113 | 1.000 | 0.74 | 0.55 |
| AC6 Taking a bath | 0.73 | 0.21 | 2.05 | 0.73 | 3.37 | 91.22 | 113 | .925 | 1.13 | 0.81 |
| AC16 Getting into a car | 0.40 | 0.22 | 1.72 | 0.40 | 3.04 | 77.10 | 113 | .995 | 0.82 | 0.68 |
| AC3 Dressing one's lower body | −0.31 | 0.24 | 1.01 | −0.31 | 2.33 | 95.52 | 113 | .868 | 0.89 | 0.85 |
| AC10 Walking outdoors on level ground | −0.37 | 0.24 | 0.95 | −0.37 | 2.27 | 114.66 | 113 | .413 | 0.90 | 1.01 |
| AC4 Taking a shower | −0.62 | 0.25 | 0.69 | −0.62 | 2.01 | 55.99 | 113 | 1.000 | 0.84 | 0.50 |
| AC13 Wiping one's upper body | −0.98 | 0.27 | 0.34 | −0.98 | 1.66 | 318.64 | 113 | <.001 | 1.05 | 2.82 |
| AC2 Washing one's upper body | −1.05 | 0.27 | 0.26 | −1.05 | 1.58 | 87.15 | 113 | .961 | 0.83 | 0.77 |
| AC12 Hanging a jacket on a hat stand | −1.21 | 0.28 | 0.11 | −1.21 | 1.42 | 141.65 | 113 | <.001 | 0.93 | 1.25 |
| AC5 Sitting on the toilet | −1.29 | 0.28 | 0.02 | −1.29 | 1.34 | 39.00 | 113 | 1.000 | 0.69 | 0.35 |
| AC1 Putting on a T-shirt | −1.56 | 0.19 | −0.24 | −1.56 | 1.08 | 92.62 | 113 | .909 | 1.07 | 0.82 |
| AC11 Washing one's face | −3.15 | 0.39 | −1.84 | −3.15 | −0.52 | 235.86 | 113 | <.001 | 1.34 | 2.09 |
| AC9 Opening a door | −3.43 | 0.40 | −2.11 | −3.43 | −0.79 | 968.98 | 113 | <.001 | 1.46 | 8.58 |
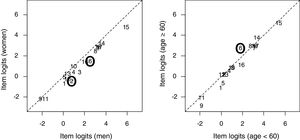
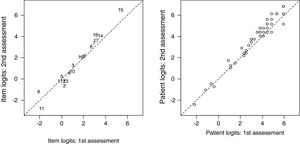
The person separation index was estimated at 0.095, showing good reliability. Intercorrelations between item residuals were below 0.5 (range, −0.34 to 0.31); the only pair of items showing a correlation greater than 0.3 was AC2 (washing one's upper body) and AC13 (wiping one's upper body), which showed a moderate effect (r=0.31). We may therefore assume that no local dependence is present. Fig. 3 shows the DIF plots for sex and age (<60 or ≥60). The results suggest that the item difficulty hierarchy differs slightly according to age for items AC2 and AC6 (P=.043 and P=.049, respectively) and for age for AC6 (P=.021), with no relevant differences.
ACTIVLIM scores showed a significant correlation with scores for the Brooke scale (r=−0.54, P<.001), the Vignos scale (r=−0.83, P<.001), Gowers time (r=−0.50, P<.001), and the FIM (r=0.87, P<.001), indicating good construct validity (Fig. 4). Scores were also associated with type of NMD (P=.045, with the Becker/limb-girdle muscular dystrophies group scoring 10-12 points lower than the remaining patients), orthosis or wheelchair use (P<.001, with patients using orthoses scoring 5 points lower and wheelchair users scoring 25 points lower than the remaining patients), and age (r=−0.32, P<.001), indicating discriminatory ability (Fig. 4). No sex-related differences were observed (P=.659).
Fig. 5 (right panel) shows the test–retest reliability of the patient measures. The ICC for patient measures is equal to 0.96. Fig. 5 also shows the DIF plot for the item difficulty hierarchy between assessments. Estimated item ICC is also equal to 0.96, indicating good reproducibility of the item difficulty hierarchy.
DiscussionOur results demonstrate that the 18 items constitute a single, ordered scalar structure; fit a unidimensional scale; present good internal consistency, construct validity, and test–retest reliability; and do not present local dependence or relevant DIF for such demographic characteristics as sex and age. No ACTIVLIM item showed reversed thresholds, indicating that participants were well discriminated in the 3 response categories.29 The lack of missing data, an indicator of the quality of a questionnaire,30 demonstrates the absence of any biases induced by lack of responses to any item. While no patient rated all items as impossible, the fact that 16% of patients regarded all the activities as easy indicates a moderate ceiling effect,12 which is probably due to the questionnaire format, with 3 possible responses per item. The high percentage of patients who were able to perform all activities may be related to the high proportion of patients with myotonic dystrophy in our sample (54.1%). This condition is characterised by distal muscle weakness that progresses slowly over a period of several years; proximal weakness typically develops late in the course of the disease. The tasks included on the ACTIVLIM are more related to proximal than to distal muscle function, which may explain this observation.4,31
The findings from the Rasch analysis support the unidimensionality of the scale and indicate that item scores may be added together, resulting in a single global score. Item AC9 (opening a door), which patients found to be the easiest action, is the only one showing poor fit. In the development of the original ACTIVLIM scale,4 this item was also identified as one of those presenting DIF in the test–retest reliability assessment. Although the evidence is insufficient to remove this item from the global score, future studies should review whether it should be removed. The standard errors associated with the estimated difficulty of each item (mean, 0.25 logits) are sufficiently small to indicate high precision,32 although standard errors for the 2 lowest-ranked items (AC9 [opening a door] and AC11 [washing one's face]) are marginal (0.39-0.40). This may be related to the fact that these activities are so common that patients develop different means of performing them.
The scale shows good reliability (R=0.95), as the 44 thresholds represent a broad range of functional status. Despite the modest ceiling effect and the fact that some items were easy to perform for many patients, the wide range of gradations for the 22 items is sufficient for measuring activity limitation in all patients. The absence of local dependence suggests that there is no redundancy or multidimensionality in the items. The item difficulty hierarchy shows nearly no age- or sex-related variability, suggesting that the ACTIVLIM may be used for any patient with a hereditary myopathy. The high ICC value (ICC=0.96) for the second assessment at 3 weeks and the invariance of the item difficulty hierarchy between assessments signal that questionnaire results are reproducible over time.
Comparison against disability measurement by other scales (the Brooke and Vignos scales, the FIM, and Gowers time) showed good construct validity, with correlation coefficients greater than 0.5 for the Brooke scale and Gowers time and greater than 0.8 for the Vignos scale and the FIM; these values are very similar to those obtained during the development of the original scale.4 Each category for the Brooke and Vignos scales represents a broad range of ACTIVLIM logit measures; this suggests that the ACTIVLIM enables differentiation between patients who fall within a single category on the other 2 scales. Compared to the FIM, the ACTIVLIM appears to discriminate more precisely between groups of patients with higher motor scores. A larger ceiling effect was observed for the FIM than for the ACTIVLIM in our sample, with 35% of patients receiving the maximum score (126 points), vs 16% for the latter scale. Gowers time does not present a floor effect, although 28% of patients were unable to complete the task, constituting missing data for that test; no missing data were recorded for the ACTIVLIM. The scale is also able to discriminate according to the need for assistance with walking, not only between wheelchair users and non-users. ACTIVLIM score is also associated with the type of NMD, with patients in the Becker/limb-girdle muscular dystrophies group scoring lower. This may be explained by differences in the distribution of muscle involvement depending on the type of myopathy, given that weakness of proximal and flexor muscles is associated with greater activity limitation.
Although the response rate was high, the small size of the sample and the relatively high number of patients scoring high on the ACTIVLIM mean that our results should be interpreted with caution. Future studies should address the sensitivity to change of the Spanish-language version of the scale; previous research has addressed this aspect of the original scale.7 It should also be noted that we focused on adult patients; it would be beneficial to perform further studies with paediatric patients, including the 4 items specific to children from the original ACTIVLIM scale. To conclude, the Spanish-language version of the ACTIVLIM is a valid, reliable instrument for measuring activity limitations in patients with hereditary myopathy. This simple self-administered questionnaire may be used to complement clinical assessment methods for measuring disability in these patients.
Conflicts of interestThe authors have no conflicts of interest to declare.
We are grateful to Dr Laure Vandervelde, the author of the original ACTIVLIM, for reviewing our results.
We would also like to thank the nurses Celia Lusarreta and Ana Peletero of the neuromuscular diseases unit at Complejo Hospitalario de Navarra for their assistance in patient selection.
Please cite this article as: Pagola I, Torné L, Jericó I, Ibáñez B. ACTIVLIM: adaptación transcultural al castellano y validación en adultos con miopatías hereditarias utilizando el modelo Rasch. Neurologia. 2021;36:514–524.