Headache is a frequent cause of consultation; it is important to detect patients with secondary headache, particularly high-risk secondary headache. Such systems as the Manchester Triage System (MTS) are used for this purpose. This study aims to evaluate the frequency of undertriage in patients attending the emergency department due to headache.
Material and methodsWe studied a series of consecutive patients who came to the emergency department with headache and presenting some warning sign, defined as the presence of signs leading the physician to request an emergency neuroimaging study and/or assessment by the on-call neurologist. The reference diagnosis was established by neurologists. We evaluated the MTS triage level assigned and the presence of warning signs that may imply a higher level than that assigned.
ResultsWe registered a total of 1120 emergency department visits due to headache, and 248 patients (22.8%) were eligible for study inclusion. Secondary headache was diagnosed in 126 cases (50.8% of the sample; 11.2% of the total), with 60 cases presenting high-risk secondary headache (24.2%; 5.4%). According to the MTS, 2 patients were classified as immediate (0.8%), 26 as very urgent (10.5%), 147 as urgent (59.3%), 68 as normal (27.4%), and 5 as not urgent (2%). The percentage of patients undertriaged was 85.1% in the very urgent classification level and 23.3% in the urgent level.
ConclusionDuring the study period, at least one in 10 patients attending the emergency department due to headache had secondary headache; one in 20 had high-risk secondary headache. The MTS undertriaged most patients with warning signs suggesting a potential emergency.
La cefalea es un motivo de consulta urgente frecuente, siendo la prioridad detectar a pacientes con cefalea secundaria, especialmente cefaleas secundarias de alto riesgo (CESAR). Para ello, se emplean sistemas de triaje como el Sistema de Triaje de Manchester (STM). Pretendemos evaluar la frecuencia de subtriaje en pacientes que acudieron a urgencias por cefalea.
Material y métodosEstudio de serie de casos consecutivos. Se analizaron pacientes que acudieron a urgencias refiriendo cefalea y tuvieron algún dato de alarma, definido como la presencia de datos que motivasen la solicitud de neuroimagen urgente y/o la valoración por neurología de guardia. El diagnóstico de referencia fue realizado por neurólogos. Se evaluó el nivel de triaje asignado por el STM y la presencia de datos de alarma que implicaría el triaje en un nivel superior al asignado.
ResultadosHubo 1120 visitas a urgencias por cefalea, siendo elegibles 248 pacientes (22,8%). Se diagnosticó cefalea secundaria en 126 casos (50,8% de la muestra, 11,2% del total), siendo 60 CESAR (24,2% y 5,4%). El STM clasificó 2 pacientes como críticos (0,8%), 26 emergencias (10,5%), 147 urgencias (59,3%), 68 como estándar (27,4%) y 5 como no urgente (2%).
El porcentaje de pacientes infratriados fue del 85,1% en el nivel “emergencia” y 23,3% en el de “urgencia”.
ConclusiónDurante el periodo de estudio, al menos uno de cada diez pacientes que acudió a urgencias por cefalea tenía una cefalea secundaria y uno de cada veinte una CESAR. El STM infratrió a la mayoría de pacientes con datos que implicarían una potencial emergencia.
Headache is the most frequent neurological symptom and the fourth most common reason for consultation with the emergency department.1–3 It is classified as primary or secondary, depending on the underlying cause.4 Secondary headache includes multiple entities of variable severity, ranging from relatively benign conditions to headache disorders associated with high morbidity and mortality.5–7 In some cases, prognosis depends on how early specific treatment is started; therefore, early, accurate diagnosis is essential.8
In the emergency department, detection of secondary headache is the main priority, especially with respect to entities whose treatment is time-dependent.5–8 Given the lack of specific biomarkers for secondary headache, diagnosis is based on the detection of warning signs either during history-taking or during the examination.2,4–8 The use of triage or classification systems in clinical practice helps to prioritise patients more likely to present potentially fatal conditions or with particularly disabling symptoms, such as pain.3,9
One of the most widely used triage systems is the Manchester Triage System (MTS).10 This tool evaluates patients according to the main reason for consultation and classifies them into one of 5 urgency categories according to the maximum recommended waiting time. In the case of headache, patients are classified into one category or another depending on the presence of certain signs or symptoms. The immediate category includes patients with airway compromise, inadequate breathing, seizures, or shock, or unresponsive children. The very urgent category includes patients with severe pain, abrupt onset, altered level of consciousness, sudden onset of complete vision loss, or meningeal signs. The urgent category includes patients with moderate pain, inappropriate medical history, history of loss of consciousness, focal or progressive loss of function, or recent neurological signs or symptoms. The standard category includes patients with pain, those feeling warm or hot, and those in whom headache is a recent problem.11
The usefulness of the MTS has rarely been evaluated in the context of headache. Only one study in a paediatric population has been conducted, reporting a sensitivity of 50% to 63%.11 Among the limitations of this study, the discriminators used in the case of headache differ from the classical, validated warning signs,5–8 the percentage of misclassification is as high as 50% in other conditions,12,13 and the tool’s sensitivity for some diseases is relatively low.12–16
The main purpose of this study is to analyse the frequency of undertriage in patients attending the emergency department due to headache and classified using the MTS.
Material and methodsWe conducted a cross-sectional study of all patients attended due to headache at the emergency department of a tertiary hospital between 1 January 2011 and 30 June 2011; to evaluate changes in diagnosis, patients were followed up for 3 years. The study was approved by our centre’s research ethics committee (CP14/425-E) and complied with the STARD guidelines.17
The inclusion criteria were as follows: 1) age above 16 years, 2) reporting headache as the main symptom at the time of triage, and 3) presenting warning signs, defined as signs or symptoms motivating an emergency neuroimaging examination or assessment by the on-call neurologist. We excluded patients whose level of consciousness prevented the description of headache characteristics and for whom we lacked sufficient data about the episode motivating the consultation with the emergency department.
We retrospectively evaluated the data gathered in the patients’ electronic medical records and followed them up for 3 years to evaluate changes in diagnosis. We analysed demographic variables (age, sex), treatment priority level according to the MTS, data about the acute event (personal history, headache symptoms, other neurological signs and symptoms detected in the neurological examination, reason for requesting a neuroimaging study or assessment by a neurologist). From medical histories, we gathered data about the MTS items evaluated in patients with headache: severe pain, abrupt onset, alterations in the level of consciousness, visual alterations, meningeal signs, history of loss of consciousness, neurological signs or symptoms, and recent onset of headache.
The study variable was MTS priority level, with the classification being simplified to 3 levels: immediate/very urgent (levels 1-2 of the MTS), urgent (level 3), and standard/non-urgent (levels 4-5). The reference diagnosis was established by 2 independent neurologists who were blinded to the MTS category assigned; any discrepancies were solved with recourse to a third neurologist. Patients were subsequently followed up through their electronic medical records for 3 years, to evaluate changes in diagnosis over time. We used the International Classification of Headache Disorders, third edition (ICHD-3),4 as this was the most recent version at the time of analysis, despite the more widespread use of previous versions. High-risk secondary headache was defined as a secondary headache that: 1) is life-threatening in the short term, 2) constitutes a significant morbidity if appropriate treatment is not administered, or 3) presents with symptoms associated with another type of headache that is life-threatening or constitutes a significant morbidity in the absence of appropriate treatment. Among life-threatening headaches, we included those caused by central nervous system infections, expansive intracranial lesions, acute cerebrovascular disease, acute intracranial hypertension, or temporal arteritis.
To evaluate undertriage, we assessed the presence and frequency of warning signs pointing to an MTS category higher than that assigned. Furthermore, we describe the demographic characteristics, frequency of warning signs, and diagnostic management data by headache type (primary, secondary, or high-risk secondary), as well as the MTS category assigned to each headache group.
Statistical analysisQualitative variables are presented as absolute and relative frequencies. Quantitative variables are expressed as medians and standard deviation (SD), or medians and interquartile ranges (IQR) for non–normally distributed variables. We evaluated the association between qualitative independent variables and the outcome variable using the chi-square test or the Fisher exact test, when more than 25% of the expected values were below 5. For quantitative independent variables, we compared means using the t test for independent samples, or the non-parametric median test in the case of non–normally distributed quantitative variables.
Type I errors or alpha errors below 0.05 led to rejection of the null hypothesis. Statistical analysis was performed with the SPSS statistics package, version 26.0 (Chicago, IL, USA) for Mac®.
ResultsDuring the study period, we recorded a total of 1120 visits to the emergency department due to headache; 248 patients (22.1%) met all the inclusion criteria and none of the exclusion criteria; of these, 158 (63.7%) were women. Mean age was 47.8 years (SD: 20; range, 16-91).
Headache typeAccording to the ICHD-3, 77 patients (31%) had primary headaches, 126 (50.9%) had secondary headaches, and 45 (18.1%) presented headaches included in the appendix of the classification or not meeting the criteria for any other headache disorder. Among primary headaches, 41 patients (53.4%) presented migraine, 24 (31.1%) had tension-type headache, 4 had trigeminal autonomic cephalalgias, and the remaining 8 had other primary headache disorders. Among secondary headaches, the most frequent was headache attributed to trauma or injury to the head and/or neck (29 cases), followed by headache attributed to infection (27); headache attributed to cranial and/or cervical vascular disorder (24); headache attributed to non-vascular intracranial disorder (23); headache attributed to disorder of homoeostasis (12); headache or facial pain attributed to disorder of the cranium, neck, eyes, ears, nose, sinuses, teeth, mouth, or other facial or cervical structure (10); and headache attributed to a substance or its withdrawal (1). Three patients had painful cranial neuropathies. Sixty patients were diagnosed with high-risk secondary headache (24.4% of the total sample and 47.6% of all secondary headaches). Over the entire study period, the proportion of secondary headaches was at least 126/1120 (11.2%; 95% CI, 9.5-13.2) and the proportion of high-risk secondary headaches was 60/1120 (5.4%; 95% CI, 4.1-6.9).
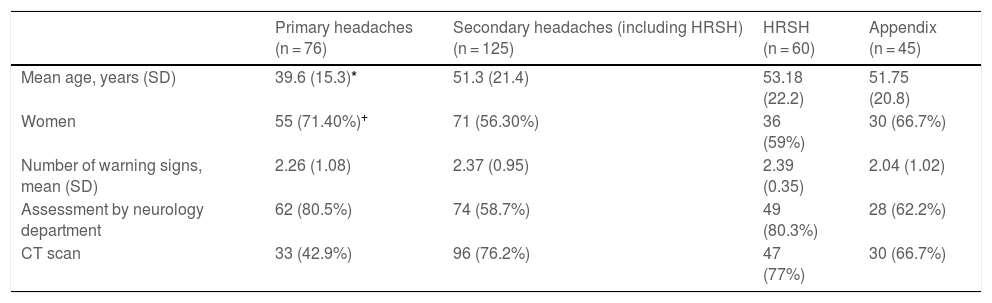
Table 1 presents the main demographic variables, number of warning signs, and management data for each diagnostic category. We found statistically significant differences in mean age (P < .001) and the proportion of women (P = .027) between the groups of patients with primary and secondary headaches.
Demographic variables, frequency of warning signs, and management data by diagnostic group.
| Primary headaches (n = 76) | Secondary headaches (including HRSH) (n = 125) | HRSH (n = 60) | Appendix (n = 45) | |
|---|---|---|---|---|
| Mean age, years (SD) | 39.6 (15.3)* | 51.3 (21.4) | 53.18 (22.2) | 51.75 (20.8) |
| Women | 55 (71.40%)+ | 71 (56.30%) | 36 (59%) | 30 (66.7%) |
| Number of warning signs, mean (SD) | 2.26 (1.08) | 2.37 (0.95) | 2.39 (0.35) | 2.04 (1.02) |
| Assessment by neurology department | 62 (80.5%) | 74 (58.7%) | 49 (80.3%) | 28 (62.2%) |
| CT scan | 33 (42.9%) | 96 (76.2%) | 47 (77%) | 30 (66.7%) |
CT: computed tomography; HRSH: high-risk secondary headaches; SD: standard deviation.
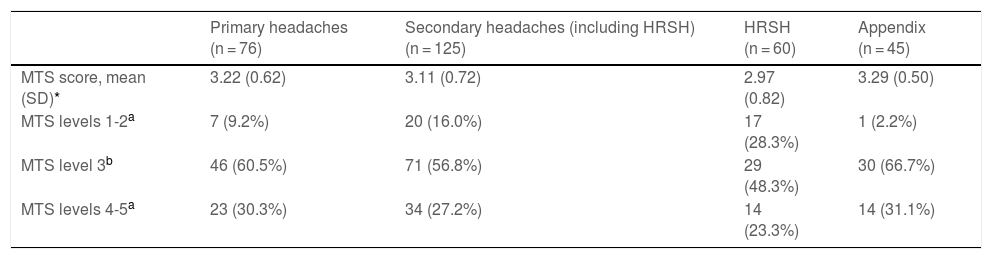
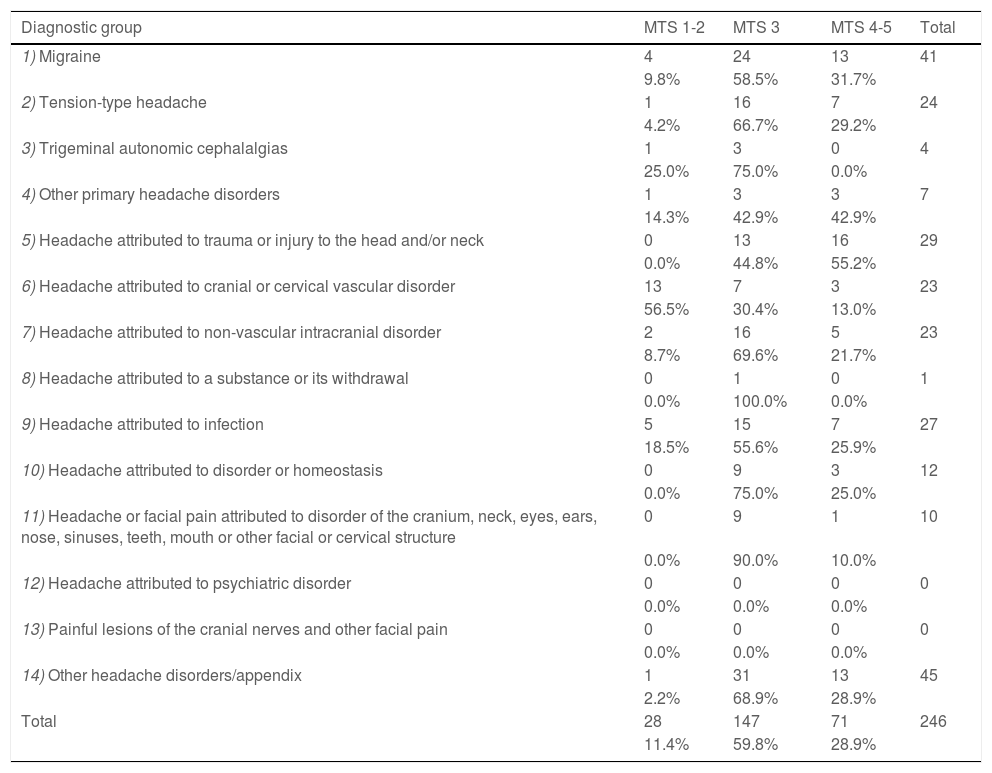
Two patients (0.8%) were assigned to the immediate MTS category, 26 (10.5%) were assigned to the very urgent category, 147 (59.3%) to the urgent category, 68 (27.4%) to the standard category, and 5 (2%) to the non-urgent category. Table 2 shows the percentage of patients assigned to each priority level by diagnostic category (primary, secondary, and high-risk secondary headache groups). Table 3 shows the numbers and percentages of patients classified within each ICHD-3 category.
Patients assigned to each Manchester Triage System category, by International Classification of Headache Disorders diagnostic group.
| Primary headaches (n = 76) | Secondary headaches (including HRSH) (n = 125) | HRSH (n = 60) | Appendix (n = 45) | |
|---|---|---|---|---|
| MTS score, mean (SD)* | 3.22 (0.62) | 3.11 (0.72) | 2.97 (0.82) | 3.29 (0.50) |
| MTS levels 1-2a | 7 (9.2%) | 20 (16.0%) | 17 (28.3%) | 1 (2.2%) |
| MTS level 3b | 46 (60.5%) | 71 (56.8%) | 29 (48.3%) | 30 (66.7%) |
| MTS levels 4-5a | 23 (30.3%) | 34 (27.2%) | 14 (23.3%) | 14 (31.1%) |
HRSH: high-risk secondary headaches; MTS: Manchester Triage System; SD: standard deviation.
Numbers and percentages of patients assigned to each Manchester Triage System category, by diagnostic group.
| Diagnostic group | MTS 1-2 | MTS 3 | MTS 4-5 | Total |
|---|---|---|---|---|
| 1) Migraine | 4 | 24 | 13 | 41 |
| 9.8% | 58.5% | 31.7% | ||
| 2) Tension-type headache | 1 | 16 | 7 | 24 |
| 4.2% | 66.7% | 29.2% | ||
| 3) Trigeminal autonomic cephalalgias | 1 | 3 | 0 | 4 |
| 25.0% | 75.0% | 0.0% | ||
| 4) Other primary headache disorders | 1 | 3 | 3 | 7 |
| 14.3% | 42.9% | 42.9% | ||
| 5) Headache attributed to trauma or injury to the head and/or neck | 0 | 13 | 16 | 29 |
| 0.0% | 44.8% | 55.2% | ||
| 6) Headache attributed to cranial or cervical vascular disorder | 13 | 7 | 3 | 23 |
| 56.5% | 30.4% | 13.0% | ||
| 7) Headache attributed to non-vascular intracranial disorder | 2 | 16 | 5 | 23 |
| 8.7% | 69.6% | 21.7% | ||
| 8) Headache attributed to a substance or its withdrawal | 0 | 1 | 0 | 1 |
| 0.0% | 100.0% | 0.0% | ||
| 9) Headache attributed to infection | 5 | 15 | 7 | 27 |
| 18.5% | 55.6% | 25.9% | ||
| 10) Headache attributed to disorder or homeostasis | 0 | 9 | 3 | 12 |
| 0.0% | 75.0% | 25.0% | ||
| 11) Headache or facial pain attributed to disorder of the cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cervical structure | 0 | 9 | 1 | 10 |
| 0.0% | 90.0% | 10.0% | ||
| 12) Headache attributed to psychiatric disorder | 0 | 0 | 0 | 0 |
| 0.0% | 0.0% | 0.0% | ||
| 13) Painful lesions of the cranial nerves and other facial pain | 0 | 0 | 0 | 0 |
| 0.0% | 0.0% | 0.0% | ||
| 14) Other headache disorders/appendix | 1 | 31 | 13 | 45 |
| 2.2% | 68.9% | 28.9% | ||
| Total | 28 | 147 | 71 | 246 |
| 11.4% | 59.8% | 28.9% |
MTS: Manchester Triage System.
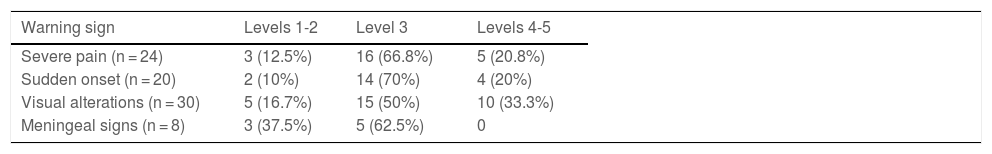
Table 4 shows the criteria used to assign a patient to the very urgent MTS category, as well as the percentage of patients who were finally assigned to each MTS category. A total of 69/82 patients (84.1%) were undertriaged (ie, assigned a score ≥ 3). The frequency of undertriage was 21/24 (87.5%) for severe pain (P < .001), 18/20 (90%) for abrupt onset (P = .006), 25/30 (83.3%) for visual alterations (P < .001), and 5/8 (62.5%) for meningeal signs (P < .001).
Frequencies and percentages of patients presenting warning signs requiring very urgent care assigned to each Manchester Triage System category. Patients assigned to categories 3, 4, and 5 are undertriaged.
| Warning sign | Levels 1-2 | Level 3 | Levels 4-5 |
|---|---|---|---|
| Severe pain (n = 24) | 3 (12.5%) | 16 (66.8%) | 5 (20.8%) |
| Sudden onset (n = 20) | 2 (10%) | 14 (70%) | 4 (20%) |
| Visual alterations (n = 30) | 5 (16.7%) | 15 (50%) | 10 (33.3%) |
| Meningeal signs (n = 8) | 3 (37.5%) | 5 (62.5%) | 0 |
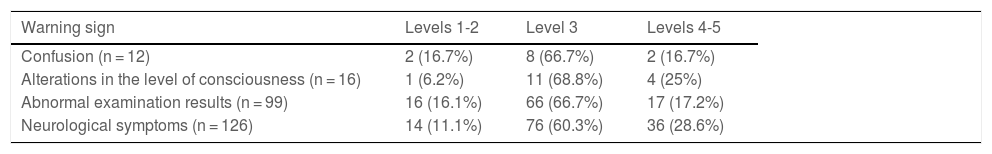
Table 5 shows the MTS classification of patients presenting at least one warning sign corresponding to the urgent care category. A total of 59 of 253 patients (23.3%) were undertriaged. The number of undertriaged patients by warning sign was as follows: 2/12 patients (16.7%) for confusion (P < .001) and 4/16 patients (25%) for history of loss of consciousness (P = .07). Undertriage was also observed in 17/99 patients (17.2%) displaying abnormal examination findings (P = .005) and in 36/126 patients (28.6%) reporting other neurological signs or symptoms (this difference was not significant).
Frequencies and percentages of patients presenting warning signs requiring urgent care assigned to each Manchester Triage System category. Patients assigned to categories 4 and 5 are undertriaged.
| Warning sign | Levels 1-2 | Level 3 | Levels 4-5 |
|---|---|---|---|
| Confusion (n = 12) | 2 (16.7%) | 8 (66.7%) | 2 (16.7%) |
| Alterations in the level of consciousness (n = 16) | 1 (6.2%) | 11 (68.8%) | 4 (25%) |
| Abnormal examination results (n = 99) | 16 (16.1%) | 66 (66.7%) | 17 (17.2%) |
| Neurological symptoms (n = 126) | 14 (11.1%) | 76 (60.3%) | 36 (28.6%) |
This study evaluates the frequency of undertriage in patients visiting the emergency department due to headache and classified using the MTS. To this end, we selected patients presenting warning signs that motivated either a neuroimaging study or a consultation with the neurology department. We did not include other patients, given that the probability of a diagnosis of secondary headache in our hospital was negligible.
The percentage of patients with secondary headaches and high-risk secondary headaches was high (11.2% and 5.4%, respectively). One of the strengths of our study is the fact that diagnoses were established by expert neurologists according to the ICHD-3.4,18 The percentage of patients with secondary headaches reported in other studies ranges from 5% to 18%,18–22 and up to 28 different causes for secondary headache have been reported. The concept of high-risk secondary headache is of particular importance considering the highly variable prognosis of these patients.8
Although primary headaches are not life-threatening, they are highly prevalent, with rates as high as 60% for tension-type headache and 20% to 30% in the case of migraine.1,18 Prevalence peaks in middle age, a period when this type of headache represents the leading cause of years lived with disability.23 In fact, the most frequent reason for consultation in patients visiting the emergency department due to headache was the exceptional severity of the episodes, in over half of the cases.9 Compared to secondary headaches, patients with primary headaches are characterised by a younger mean age and a higher proportion of women.18
Of a total of 248 patients, only 7 were assigned to the immediate or the non-urgent MTS categories; this reflects the fact that, despite the existence of 5 categories, most patients are assigned to one of the middle 3 categories. According to a European multicentre study including over 280 000 patients, the percentage of patients assigned to the immediate MTS category ranged from 0.6% to 1.7%, with 0.3% to 2.1% assigned to the non-urgent category.17 According to a meta-analysis, over 50% of patients are assigned to the incorrect triage category.13
Median MTS scores differed between the primary headache, secondary headache, and high-risk secondary headache groups; however, the magnitude of the mean difference was small (0.11 over 5 points). These differences were due to the higher number of patients assigned to the very urgent category in the high-risk secondary headache (28.3%) and secondary headache groups (16.0%) than in the primary headache group (9.2%). No significant differences were found in the percentages of patients assigned to the urgent category; this percentage is similar to those reported in paediatric populations (9.4%-15.2%)11 and in prospective cohort studies (21.8%), although these do not focus on headache.12 This is particularly relevant considering that the sample was selected based on the presence of warning signs.
Few data are available on the sensitivity of the MTS, which has only been analysed in the paediatric population.11 Studies evaluating the accuracy of the MTS are scarce; studies have reported sensitivity values of 70.4% in patients with sepsis24 and 44.6% in those with acute coronary syndrome.25 In the general population, studies show sensitivity values ranging from 47% to 87%12,15; according to a meta-analysis,13 the sensitivity of the MTS for detecting patients requiring very urgent or urgent care is 53%. However, the sensitivity of this tool for patients assigned to the standard or non-urgent categories is over 97%.13 Given the implications of the failure to diagnose patients with high-risk secondary headache, the detection of severe conditions should always be prioritised.
In our study, we also analysed whether the criteria for the very urgent or urgent categories were adequately detected during the application of the MTS. In the very urgent category, 62.5% to 90% of the variables were not correctly detected; and in the urgent category, 16.7% to 28.6% of items were not detected. Previous studies underscore the influence of the triage nurse’s experience and the number of patients classified.26 In the case of the MTS, some authors have shown that the selection and detection of an appropriate discriminator is essential to assigning patients to the correct triage level.27
No objective biomarkers are currently available for headache.3 Unlike in the case of chest or abdominal pain, no analytical markers can guide physicians in clinical decision-making.5 Contrary to popular belief, neuroimaging biomarkers have low sensitivity in the absence of strong diagnostic suspicion.8 It should be noted that such entities as venous sinus thrombosis, certain space-occupying lesions, and central nervous system infections may go undetected in conventional neuroimaging studies performed at the emergency department.5,6 In the United States, the percentage of patients with headache undergoing neuroimaging studies nearly tripled between 1998 and 2008, without a proportionate increase in the frequency of diagnosis of intracranial alterations.28 Some authors have proposed and validated the use of clinical decision-making tools to guide the indication of neuroimaging studies, achieving a 37.6% decrease in the number of scans requested.29
Today, the diagnosis of headache is still based on data from the medical history and physical examination.2,3 A series of signs and symptoms, known as red flags or warning signs, are frequently associated with secondary headaches. Expert groups have published lists of the main red flags,30,31 although very few validation studies have been conducted.6,9 The most recent list is that published by the International Headache Society’s Secondary Headache Special Interest Group, which includes 15 warning signs and is based on the mnemonic SNNOOP10.31 Interestingly, the MTS does not include 9 of the 15 warning signs listed in the SNNOOP10 list: systemic symptoms, history of neoplasm, age of onset older than 50 years, positional headache, triggered by coughing or Valsalva manoeuvres, onset during pregnancy or puerperium, eye pain, immunosuppression, and association with medication overuse. However, the MTS does include items suggested in prospective studies6,9 or in clinical decision tools designed to assist in the indication of neuroimaging studies.29
In contrast, some items of the MTS may be considered relatively nonspecific, and are not included in the traditional lists of red flags. Among these, we may include severe pain or inappropriate history3; others are relatively ambiguous, such as visual alterations, sudden onset, or feeling hot. Finally, some red flags, such as neurological or meningeal signs, require thorough examination, which is not always feasible during triage.
Our study presents several limitations, including its single-centre design, retrospective data analysis, and the fact that data were not systematically gathered. In our study, the number of secondary headaches and patients assigned to the immediate MTS category may have been underestimated, given that these patients are usually transferred directly to the shock room by the prehospital emergency services without previous triage by the nursing staff. Among the strengths of this study, diagnoses were confirmed by neurologists and classified according to the ICHD-3, and patients were followed up to confirm the initial diagnosis. This is the first study evaluating the MTS in adults with headache. Future studies should seek to replicate our methods, gathering data systematically and assessing the sensitivity and specificity of each variable in a larger sample.
ConclusionIn our sample, one in every 10 patients visiting the emergency department due to headache was diagnosed with secondary headache, and one in every 20 was diagnosed with high-risk secondary headache.
The MTS assigns most patients with headache to the 3 intermediate categories, with similar rates among patients with primary and secondary headaches.
Four in every 5 patients meeting criteria for the very urgent category and one in every 4 patients meeting criteria for the urgent category were undertriaged.
FundingThis study has received no specific funding from any public, commercial, or non-profit organisation.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank the emergency department for their work and their participation in the study.