Tonic pupil syndrome is a disorder secondary to lesion to the parasympathetic pathway at the ganglionic or postganglionic level.1 Manifestations include mydriasis with abolished or minimal pupillary reflex (with vermiform movements of the iris due to contraction of normally innervated segments of the iris sphincter, only visible with a slit lamp). Constriction with near effort is present (light-near dissociation) and results from subsequent aberrant reinnervation of the iris sphincter by fibres which were originally destined for the ciliary muscle. This reaction is tonic, that is, slow and sustained. Furthermore, the syndrome also manifests with cholinergic supersensitivity due to postganglionic denervation.2
The origin of the injury may be local (viral ciliary ganglionitis, open or closed trauma, or orbital tumours), or systemic-neuropathic (syphilis, alcohol abuse, diabetes, amyloidosis, or paraneoplastic alterations). However, its most frequent variant is idiopathic tonic pupil or Adie syndrome,1 which predominantly affects women (70%) in the third to the fifth decades of life. It is caused by a painless degeneration of the ciliary ganglion and posterior funiculi, sometimes associated with a slow viral infection.3
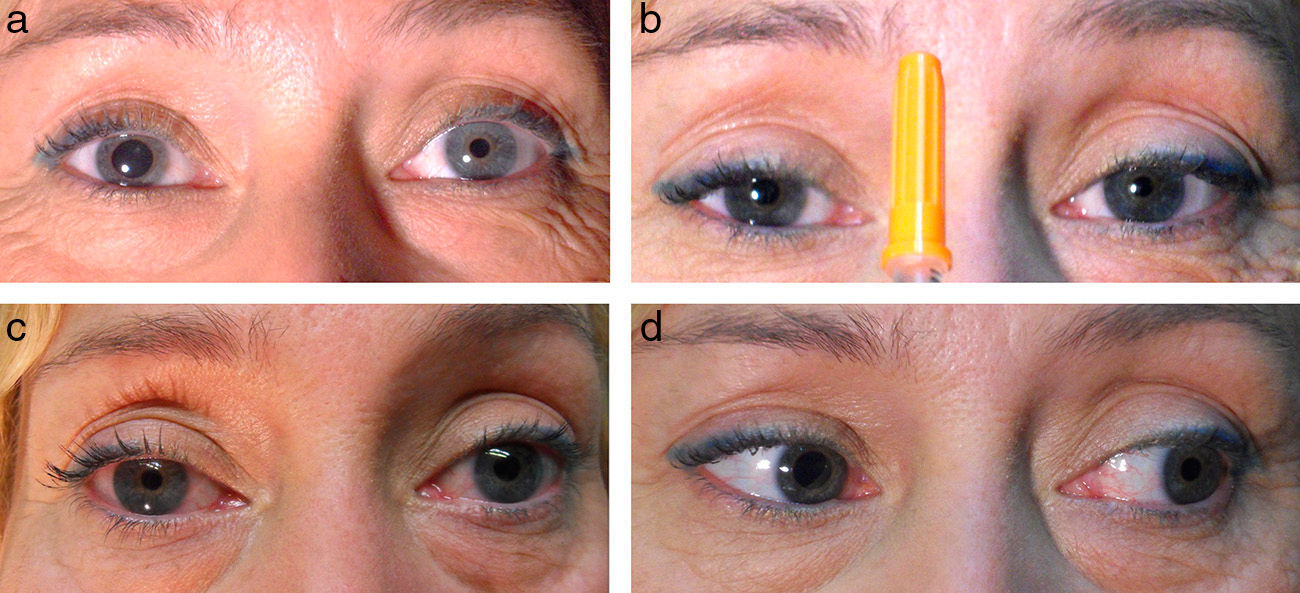
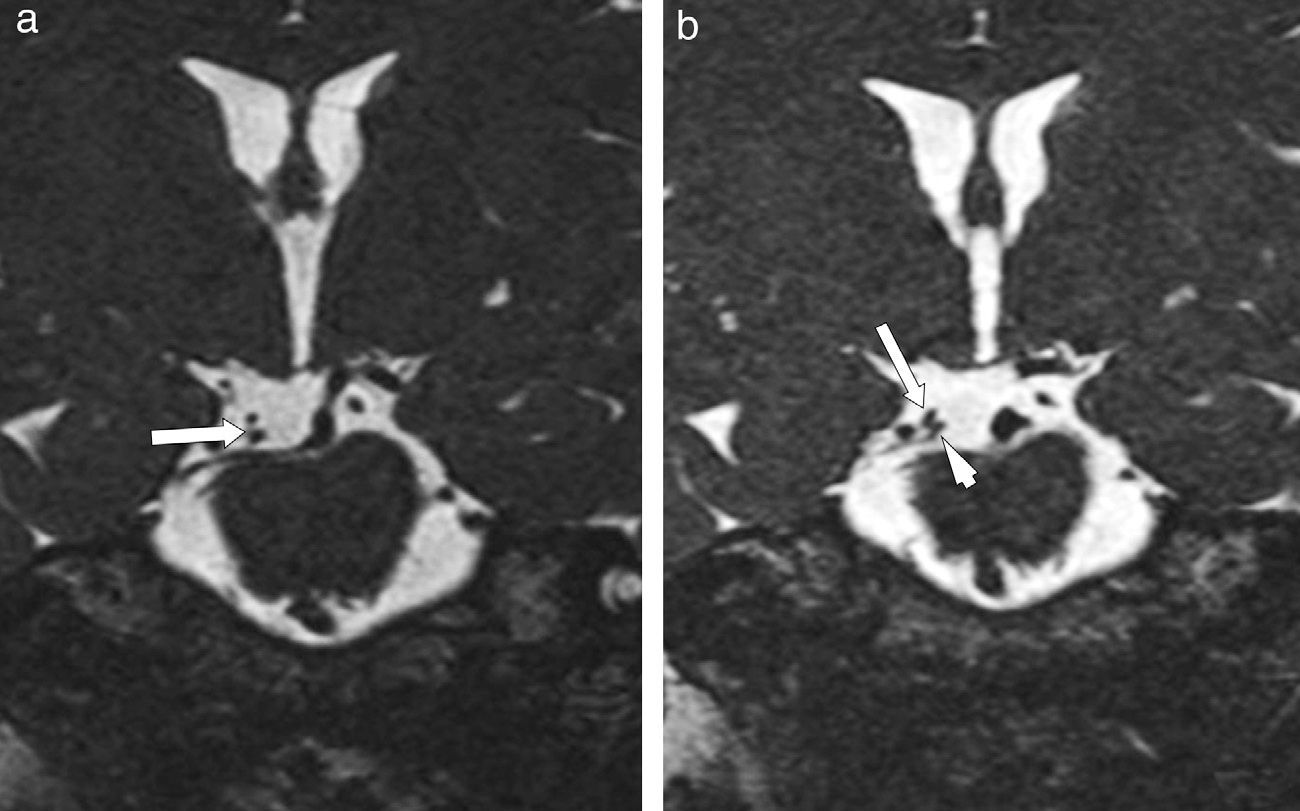
We present the case of a 44-year-old woman with flash blindness and a 7-year history of anisocoria. She reported having suffered head trauma 20 years previously and migraine-like headache that was being treated with flunarizine. The brain magnetic resonance imaging (MRI) ordered by her neurologist showed a kink at the ostium of the right posterior cerebral artery, originating from the carotid system. Since the kink was touching the superior branch of the ipsilateral oculomotor nerve (OMN), doctors suspected compression of the parasympathetic fibres and referred the patient to our department. We examined her and observed anisocoria due to right mydriasis that was more pronounced under photopic conditions. Direct photomotor reflex and consensual response were abolished in the right eye (RE) but remained intact in the left eye (LE). The near response was normal with a tonic reaction. Extrinsic eye movements were normal with no pupillary response to isolated RE adduction. Biomicroscopy results showed an irregular right pupil with minimal sectoral movements in response to light. Instillation of 0.125% pilocarpine into the conjunctival sac provoked miosis in the RE and no response in the LE (Fig. 1). Bilateral osteotendinous hyporeflexia was also observed. In view of these findings, we proposed the diagnosis of Adie syndrome. Neurologists requested a new gadolinium contrast MRI with thinner slices which revealed displacement of the right OMN without compression (Fig. 2). We therefore opted for watchful waiting.
Clinical examination: light-near dissociation. a) Anisocoria due to mydriatic right eye. b) Intact near-response (tonic response in the RE). c) Response to instillation of 0.125% pilocarpine (RE, mydriasis caused by cholinergic denervation supersensitivity; LE, intact). d) No miosis with RE adduction (aberrant reinnervation of the OMN is ruled out).
Pupil abnormalities are examined relatively frequently in neuro-ophthalmology clinics. Finding the lesion location and cause is necessary to assign an accurate diagnosis and subsequently, an appropriate treatment approach. Non-reactive mydriasis may be caused by lesion to the parasympathetic pathway, which can be located at one of several levels: nuclear, preganglionic, ganglionic, and postganglionic.1
In this case, differential diagnosis includes lesion to the OMN (preganglionic) and Adie's tonic pupil (ganglionic/postganglionic). Furthermore, differential diagnosis was complicated in this case by results of an imaging scan showing an anatomical variant of the origin of the posterior cerebral artery which might compress parasympathetic fibres of the right OMN. A compression injury to this nerve at the point where it leaves the midbrain may affect parasympathetic fibres, causing mydriasis on the affected side due to a preganglionic defect.3
However, clinical signs do not indicate compression injury to the OMN at that level. Light-near dissociation, tonic near-response, and vermiform movements of the iris may indicate tonic pupil. Although the supersensitivity test with pilocarpine has traditionally been used to diagnose tonic pupil, positive results are not exclusive to postganglionic parasympathetic lesions but may also be seen with preganglionic lesions.4,5
Aberrant reinnervation of the pupil by parasympathetic fibres originally destined for the ciliary muscle depends on the axonal distribution of the ciliary muscle and pupillary sphincter (typically a 30:1 ratio). An abnormal distribution causes light-near dissociation. A similar phenomenon occurs with compressive lesions to the OMN with aberrant reinnervation of the pupillary sphincter by fibres originally destined for the medial rectus muscle. This produces a false light-near dissociation because the pupil responds not only to near objects but also to any eye adduction movement.1
Clinical findings associated with bilateral osteotendinous hyporeflexia suggest Holmes-Adie syndrome as a diagnosis for our young female patient, after reconsidering the initial diagnosis suggested by MRI findings. Adopting a multidisciplinary approach to these patients helps determine the diagnosis and an appropriate treatment strategy.
Conflicts of interestThe authors have no commercial interests nor have they received any financial support.
The authors declare that this article has not been published or submitted to another journal for publication. They also confirm transfer of the copyright of this article to the Spanish Society of Neurology.
Please cite this article as: Arciniegas-Perasso CA, Díaz-Cespedes RA, Manfreda-Domínguez L, Toro-Giraldo D. Defecto pupilar eferente, ¿preganglionar o posganglionar? Diagnóstico clínico vs neuroimagen. Neurología. 2016;31:66–68.