Neurofibromatosis type 1 (NF1) is caused by a mutation of the NF1 gene, which is located in chromosome 17q11.2.1,2 Neurofibromas account for 90% of all cases, with plexiform tumours appearing less frequently. While neurofibromas are benign nerve sheath tumours, up to 10% of all plexiform neurofibromas may undergo malignant transformation.
We present the case of a girl aged 8 years and 4 months who was diagnosed with NF1 at the age of 2 years. Four days after surgical tonsillectomy and adenoidectomy, she presented inability to walk, associated with paraesthesia (cramps) in the left leg and foot. Examination revealed loss of strength in the left foot, inability to perform dorsiflexion, inadequate eversion/inversion, and positional talipes. The patient was unable to walk whether with normal or abnormal gait. Babinski sign was absent. Deep tendon reflexes were present without an increase in the reflexogenic area. Positive Lasègue's sign on the left side.
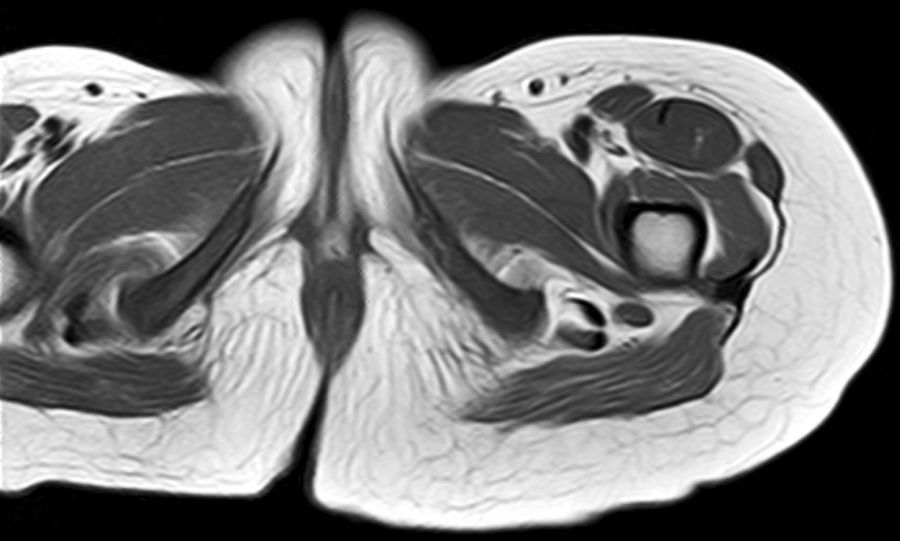
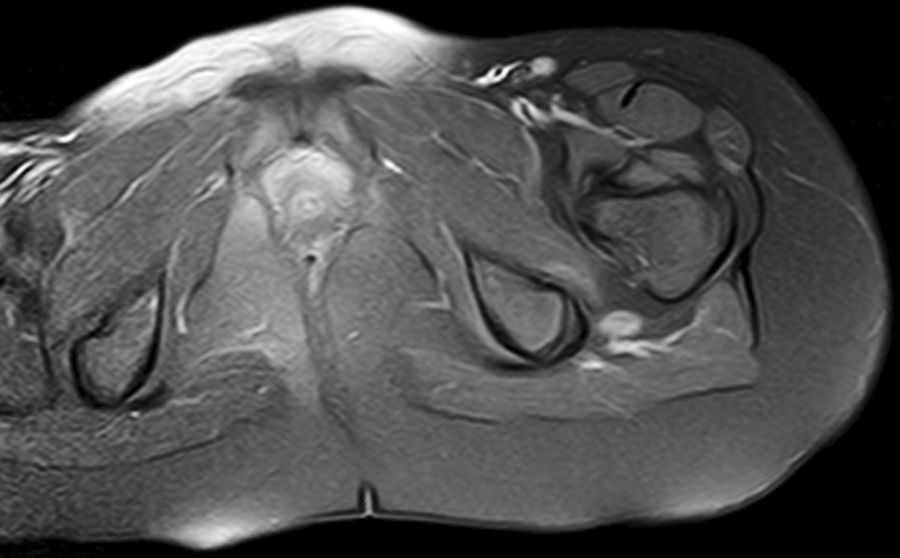
Complementary tests were as follows: radiographies of both hips, and the left foot and leg; ultrasound of the popliteal fossa and proximal third of the left leg that ruled out vein thrombosis; and a complete blood count in which coagulation, autoimmunity, and CPK readings were normal. The electroneurogram and electromyogram showed signs compatible with partial axonal mononeuropathy (axonotmesis) of the left common sciatic nerve mainly affecting the peroneal component. The patient was also studied using lumbosacral spinal, pelvic, and lower limb MRI, which showed a well-defined soft tissue lesion in the theoretical path of the left sciatic nerve, which was visible from the sciatic notch caudally to the popliteal fossa. This finding was compatible with neurofibroma (Figs. 1 and 2).
Plexiform neurofibromas are tumours that affect nerve structures (plexus, fasciculus, or nerve branches).3 The incidence of NF1 type 1 is estimated to be about 17%.2 The imaging study used to detect and characterise this disorder was MRI. We completed a general exploration of the 3 spatial planes with a T1-weighted sequence, fat-suppressed T2-weighted sequence, and fat-suppressed T1-weighted sequence after administration of intravenous gadolinium. Neurofibromas are usually hyperintense in the T2-weighted sequence. They show enhancement after administration of intravenous contrast, they are anatomically related to a nerve, and they may present a target pattern.3–6 Twelve percent of these lesions undergo malignant transformation and they generally present rapid growth or sustained pain. Positron emission tomography may be useful for studying these lesions in cases of suspected malignant transformation; some studies have calculated sensitivity and specificity levels as high as 90% and 87%, respectively.7–9 Symptomatic and/or malignant lesions are treated surgically. Chemotherapy and radiotherapy are employed in cases of malignant transformation. Angiogenesis inhibitors or cell-differentiation-inducing agents have also been used, given the vascular origin of these lesions.10
Our patient was referred to the hospital's rehabilitation department and treated with gabapentin for 2 months. We performed a neuropsychological study which revealed normal results, as well as an MRI showing no new lesions. Two years after the episode, she was pain-free and gait was normal. The neurological examination showed no deficits.
In conclusion, gabapentin may be useful for treating the neuropathic symptoms of plexiform neurofibromas. Where such neurofibromas are present, doctors should monitor any symptoms and signs that may indicate malignant transformation of the lesion.
Please cite this article as: Pérez Villena A, et al. Neurofibroma plexiforme en paciente de 8 años. Neurología. 2013;28:319–20.