Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterised by venous and/or arterial thrombosis and recurrent miscarriage and other complications in pregnancy; these events are associated with the presence of antiphospholipid antibodies (APL).1 Neuroretinitis is an inflammation of the retina with papilloedema and star-shaped macular exudates. It is rarely associated with APS. We describe an unusual case in which APL presented as neuroretinitis and intracranial venous thrombosis.
The patient was a 16-year-old girl with no relevant medical history. She reported to the emergency department due to holocranial headache, nausea, and vomiting in the previous week, accompanied by decreased visual acuity. She reported no prior treatments and no systemic or infectious symptoms.
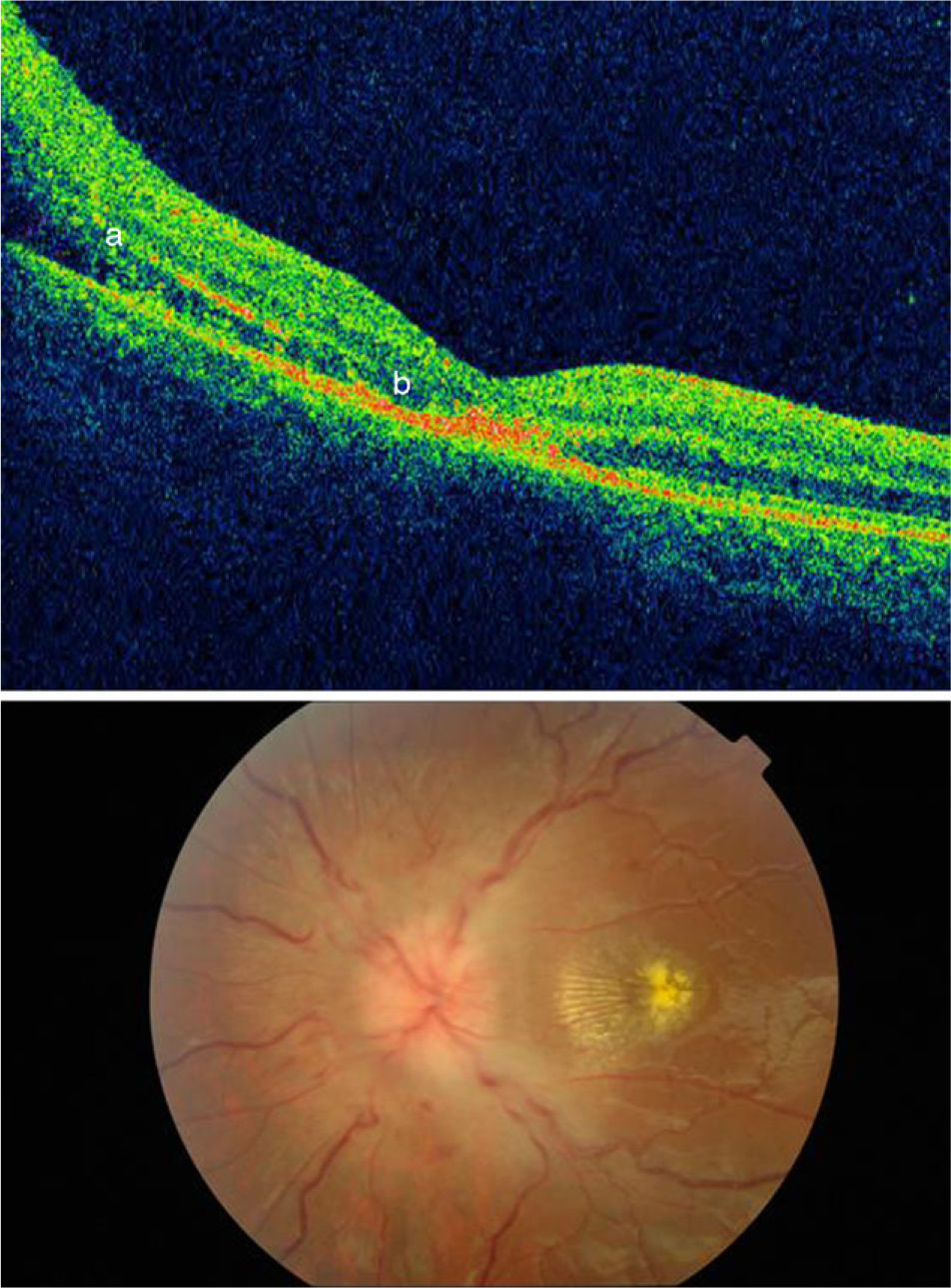
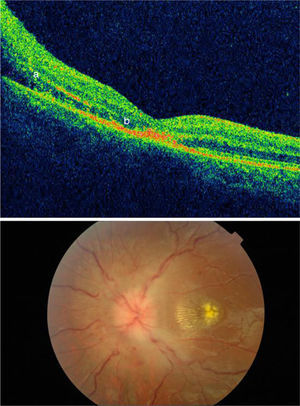
Visual acuity was 8/30 in the right eye and 8/40 in the left. Doctors detected a bilateral afferent pupillary defect. Fundus: papilloedema and star-shaped macular exudates in the retinal pigment epithelium compatible with neuroretinitis; macular star was present in both eyes (Fig. 1). Optical coherence tomography (OCT) displayed papilloedema with extravasation into the macula and photoreceptor damage (Fig. 1). Blood analysis revealed a moderately low white blood cell count. The patient tested positive for antinuclear antibodies (ANA+titre 1:640) with a homogeneous speckled pattern. Test results for rheumatoid factor, anti-Ro antibodies, anti-SM antibodies, and anti-DNA antibodies were negative. The coagulation test showed a high activated partial thromboplastin time at 78.1seconds. The patient was positive for lupus anticoagulant (LA) and had elevated levels of anticardiolipin antibodies (ACA) (titre>IgG 80) and anti-β2-GPI antibodies (anti-IgG 85).
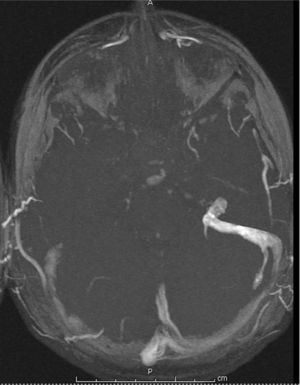
Lumbar puncture opening pressure was 46cm H2O, and cytochemical examination of cerebrospinal fluid yielded normal results. Intracranial magnetic resonance angiography showed right transverse and sigmoid sinus thrombosis (Fig. 2) with no lesions in the cerebral parenchyma. Axial brain MRI showed retinal oedema in the left eye (Fig. 3). Results of serological tests were negative for syphilis, borreliosis, neurotropic virus, and Bartonella henselae. Tests at 12 weeks found elevated levels of ACA and LA (IgG 154) and anti-β2-GPI antibodies (anti IgG: 37, IgM: 39). Results for ANA were negative.
The patient experienced intracranial hypertension secondary to intracranial venous thrombosis of the sinuses. She met the diagnostic criteria for APL based on prothrombotic phenomena and positive tests for ACA and LA antibodies. She began treatment with prednisone dosed at 1mg/kg, acetazolamide, and acenocoumarol as anticoagulant. At present, after 3 years of follow-up, the patient has not experienced any further thrombotic events or vision loss associated with the optic disc.
The diagnostic criteria for APL include the presence of at least one clinically significant thrombotic event and LA, ACA, anti-β2-GPI, or other antibodies. Our patient first experienced intracranial sinus thrombosis that caused intracranial hypertension, which manifested as headache of organic origin, vision loss, and papilloedema.
Neuroretinitis with disc oedema and macular star is an optical neuropathy characterised by oedema of the optic nerve, peripapillary oedema, macular hard exudates, and often by the presence of cells in the vitreous humour.2 The macular star is formed by lipid deposition in the plexiform layer, which results in serous retinal detachment. The reabsorption of serous fluid around the macula leaves behind star-shaped lipid precipitates. This process occurs at the onset of vision loss or 1 to 2 weeks later. The presence of macular star may be associated with neuroretinitis, hypertensive retinopathy, and papilloedema.3 Most patients with neuroretinitis experience different degrees of vision loss with dyschromatopsia. The condition is not painful and it is frequently associated with afferent pupillary defect and centrocecal scotoma. Papilloedema is an early sign of neuroretinitis and it may develop into peripapillary oedema and splinter haemorrhages. Most cases of neuroretinitis are idiopathic, but some infrequent causes that should be considered include certain non-specific viral infections or immune-mediated processes. The most commonly involved viruses are herpes simplex, herpes zoster, the hepatitis B virus, and the mumps virus. The most common bacterial causes are toxoplasmosis, syphilis, cat scratch disease, and Lyme disease. Non-infectious causes of neuroretinitis, for example, as the initial manifestation of systemic lupus erythematosus or APL, have rarely been described in the literature.4 Ophthalmological manifestations in antiphospholipid syndrome vary considerably and their incidence rates range from 8% to 88%. The structures most likely to be affected are the retina, the choroidal vessels, oculomotor nerves, and the visual pathway.5 The presence of papilloedema in these cases has been linked to diffuse retinal ischaemia or anterior ischaemic optic neuropathy.6 The pathophysiological process behind neuroretinitis in our case was clearly related to intracranial hypertension caused by intracranial venous thrombosis with increased pressure. Intracranial hypertension acts on the optic nerve, which leads to papilloedema. In addition, cases of ischaemia and thrombotic phenomena in both the retinal vessels and the optic disc have been described in the pathophysiology of neuroretinitis due to antiphospholipid syndrome, according to the existing literature.7
We present the case of an adolescent girl with neuroretinitis of non-infectious origin due to transverse sinus thrombosis in the context of primary APL. Numerous references point to a link between APL and optical neuropathy, occlusive retinal disease, and scleritis/episcleritis. Neuroretinitis is a rare presentation of APL.
Please cite this article as: Pelegrina Molina J, Barrero Hernández FJ, Callejas Rubio JL, Anaya Alaminos R, Ortego Centeno N. Neurorretinitis y trombosis venosa intracraneal en el síndrome antifosfolípido. Neurología. 2014;29:318–320.