Tuberculous meningitis (TBM) remains the most severe form of extrapulmonary tuberculosis, despite breakthroughs in diagnostic and treatment procedures. It is one of the most frequent causes of meningitis in adults and both mortality and morbidity rates are high.1–3 Neurovascular manifestations are not uncommon in TBM and they typically appear in advanced stages of the disease, especially when early treatment is not provided.4
We present a case that differs from those generally described in that neurovascular effects presented alongside the first clinical symptoms and affected an unusual region of the brain, making diagnosis difficult.
A male patient aged 47 with a personal history of smoking and migraine without aura was admitted to our neurology department on an emergency basis. The patient experienced sudden-onset right frontoparietal headache followed by fever and progressive decrease in level of consciousness. He had displayed irritability in the 3 preceding weeks, which could be interpreted as a non-specific prodromal symptom.
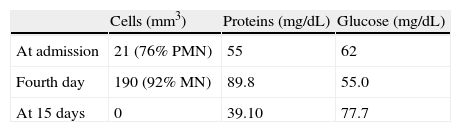
During the neurological examination at time of admission, the patient was lethargic with nuchal rigidity and mild right faciobrachial hemiplegia. Doctors performed a computed tomography (CT) study at that time, which revealed a hypodense area in the right parieto-temporal region. Lumbar puncture yielded cerebrospinal fluid (CSF) with pleocytosis (21 cells/mm3, predominantly polymorphonuclear [76%]) and mild hyperproteinaemia (55mg/dL) with no glucose uptake. Doctors began treatment with acyclovir and ceftriaxone; the patient's level of consciousness improved, but fever and headache remained.
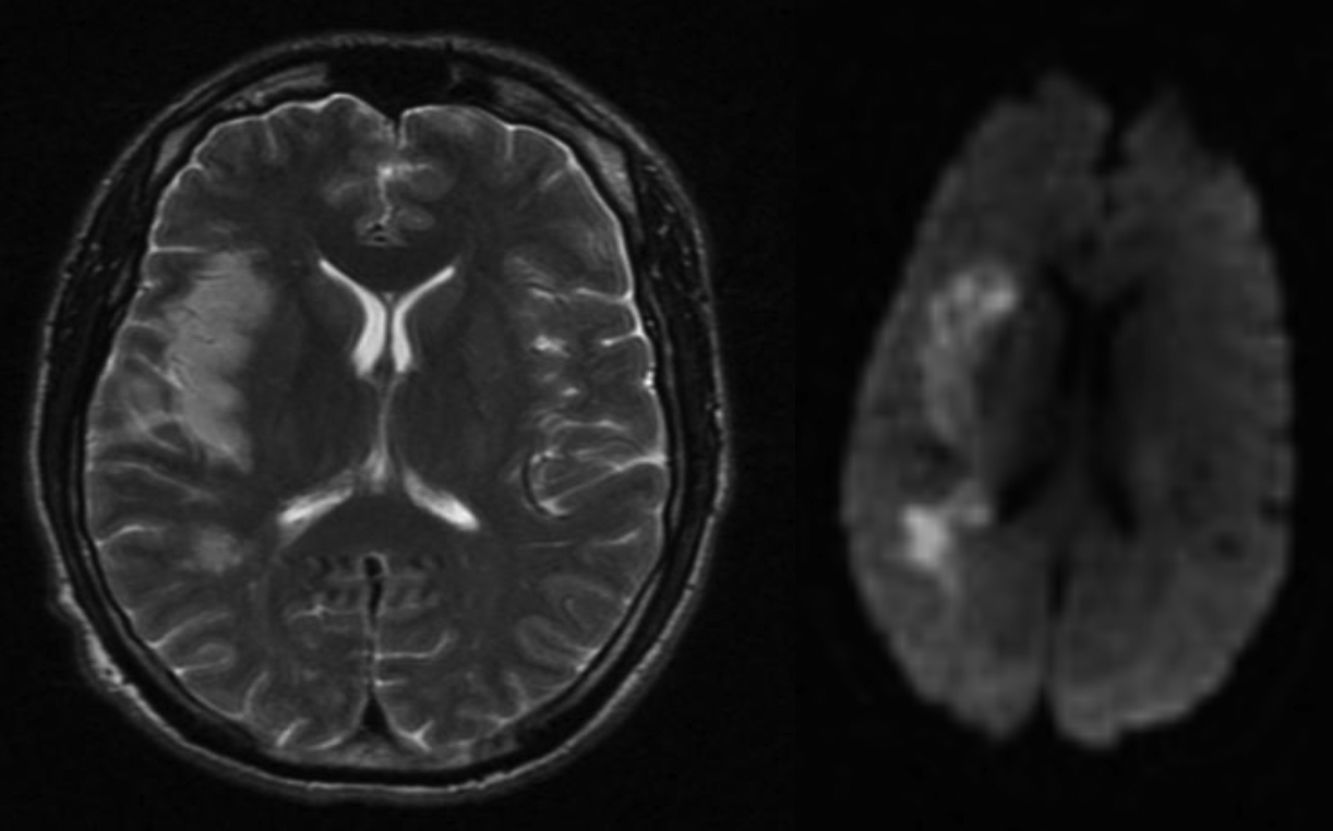
A brain MRI performed a few days later revealed an established infarct in the right parieto-temporal area (Fig. 1). MRI angiography showed amputation of distal branches of the right middle cerebral artery (MCA) and no other changes in intracranial circulation. A neurosonology study showed evidence of distal occlusion of the right MCA with signs of partial recanalisation (TIBI grade IV) of a more proximal occlusion in the M1 segment.
On the fourth day after hospitalisation, given the patient's clinical progression, we repeated the CSF study and found that pleocytosis had increased (190 cells/mm3) and was now predominantly mononuclear. Hyperproteinaemia had also increased to 89.9mg/dL, with no glucose uptake (Table 1). In light of a suspected case of tuberculous meningitis, doctors began treatment with isoniazid, rifampicin, pyrazinamide, ethambutol, and dexamethasone. Both headache and fever resolved rapidly. The polymerase chain reaction (PCR) test for Mycobacterium tuberculosis (M. tuberculosis) was positive.
The patient's neurological examination at time of discharge was normal. Over the following weeks, neuroimaging and neurovascular studies showed persistence of the infarct and the distal occlusion in the right MCA with complete recanalisation of the stenotic area in the proximal part of the M1 segment. CSF parameters normalised completely (Table 1).
Symptoms such as fever, headache, or nuchal rigidity do not distinguish meningeal tuberculosis from other forms of bacterial meningitis.2 CSF studies may yield very distinct results, with leukocyte counts or protein levels that may not be very high, and varying percentages of neutrophils and glucose uptake rates. In any case, detecting M. tuberculosis in CSF, cultured fluid, or by PCR yields a definitive diagnosis of TBM.2
The most dangerous complication of TBM is secondary cerebrovascular affectation, which is also the leading cause of established neurological deficit. This syndrome is relatively common, and its frequency varies according to whether we define it by the presence of neurological symptoms (in 20%), CT findings (13–35%) or MRI findings (up to 57%).4 Although cases of TBM have been described in which focal symptoms appear as the first manifestation or present in the first days of illness,4–6 these symptoms normally appear in long-term illness and may persist despite treatment with tuberculostatic drugs and corticosteroids.6–8 Focal symptoms predict increased TBM-related mortality.9 It has been shown that advanced age, visual changes or changes in cranial nerves, meningeal uptake in initial imaging studies, and elevated levels of polymorphonuclear leukocytes in CSF (as in our case) predict a presentation of TBM with neurovascular impairment.5,8
Meningovascular tuberculosis affects anterior circulation more frequently than posterior circulation, and in most cases it affects the territory corresponding to the MCA.8,10 The most common localisations for infarcts are the internal capsule and basal ganglia, which correspond to the territory depending on lenticulostriate and thalamic perforating vessels. Bilateral and often symmetrical infarcts in basal ganglia are especially characteristic of TBM.4,6 Cortical or subcortical lesions, like those in our patient, are less common, and they have most often been described in cases with prolonged progression.4
The test of choice for detecting these infarcts is MRI, which may also show leptomeningeal or pachymeningeal enhancement, hydrocephalus, or tuberculomas.6 MRI angiography is a very sensitive test for detecting vascular impairment, although images in TBM are no different from those in other systemic or infectious forms of vasculitis. The study may show stenotic areas, irregularities or, as in our patient, obstructions; vasculitis is sometimes detected without there being an infarct in the corresponding territory.6 Similar findings can be identified in CT angiography studies.11
The pathogenesis of meningovascular tuberculosis has not been fully defined, although researchers believe it arises from vasculitis and associated intimal proliferation, which has been described in 30% to 70% of all cases.6
Treatment for TBM with neurovascular impairment consists of corticosteroids associated with tuberculostatic drugs such as those used to treat our patient. This approach decreases risk of death and neurological sequelae.6 Nevertheless, doctors must be aware of the possibility of a hypersensitivity reaction that would lead to a worsened clinical state and require other immunosuppressants.12
In conclusion, TBM is a relatively frequent entity whose clinical signs are non-specific; in addition, neuroimaging and CSF findings resemble those in other infections of the central nervous system. Appearance of a focal neurological deficit in a case of TBM should suggest secondary neurovascular impairment, even in patients who are receiving appropriate treatment. Nevertheless, as this case description shows, a cerebral infarct with an atypical location may be a form of presentation of TBM, which should be considered when vascular symptoms appear in association with meningeal syndrome and CSF changes. Rapid discovery of a positive PCR test for M. tuberculosis will permit use of a specific and early treatment. In some cases, such as the one described here, this may prevent the appearance of other complications and residual symptoms.
Please cite this article as: Mulero Carrillo P, Pedraza Hueso MI, Rojo Martínez E, Guerrero Peral ÁL. Tuberculosis meningovascular: descripción de un caso con presentación atípica. Neurología. 2014;29:187–189.
Partially presented in poster format at the 15th Congress of the European Federation of Neurological Societies, Budapest, September 2011.