Tumours of the leptomeninges with melanin pigment are classified as melanotic meningioma, melanoma, melanotic schwannomas and meningeal melanocytoma.1 It is especially important to diagnose these cases correctly due to their different clinical evolution and the possible treatments that can be used. We describe a case of meningeal melanocytoma in the dorsal spinal cord – a case with poor biological behaviour despite the fact that these have usually been labelled as benign tumours.
A 68-year-old female presented symptoms of urinary retention, loss of strength and lower limb dysesthesias of about 20 days’ evolution. In the somatosensory-evoked potentials (SEPs), there was a decrease in amplitude and delayed latency in the lower limbs, predominantly on the right. The magnetic resonance imaging (MRI) of the cervical and dorsal spinal cord shows a spinal injury at D9 level indicative of cavernous angioma with adjacent chronic haematoma. The patient later presented an abrupt deterioration with bilateral flaccid paraplegia. An urgent surgical procedure was carried out with a complete laminectomy at the level of D9 and a partial one at D8 and D10, with solid intradural extramedullary haematoma presence, mainly at D9 level. This was not extracted as it was found to be hard and adhered to medullary tissue, and was suspected of being a vascular malformation. A spinal arteriography was carried out after the operation and this was found to be normal. A second opinion was sought. The MRI was repeated and a lesion was found with an intramedullary component and another intradural extramedullary one, which is hypointense in T2 and hyperintense in T1, with no enhancement after gadolinium administration, and was interpreted as a haematoma. We saw a disturbance in the intramedullary signal in T2 in the axial cuts, from D7 to D11, undemonstrative of cavernoma. She was operated on again and we found a very dark red lesion on the inside of the spinal cord, with a colour suggesting a chronic haematoma but that was hard and bled slightly. The lesion was removed, separating it from the medullary tissue. In the histopathological study, we saw intense medium- to large-size epithelioid cell infiltration, with large eosinophilic cytoplasm characterised by the large amount of granular melanin pigment, which was negative for iron. The immunohistochemical analysis showed immunoreactivity in approximately 2% of the cells with Ki-67 antigen, absence of immunoreactivity to P-53 and submembrane reinforcement of 20% compared to C-Kit.
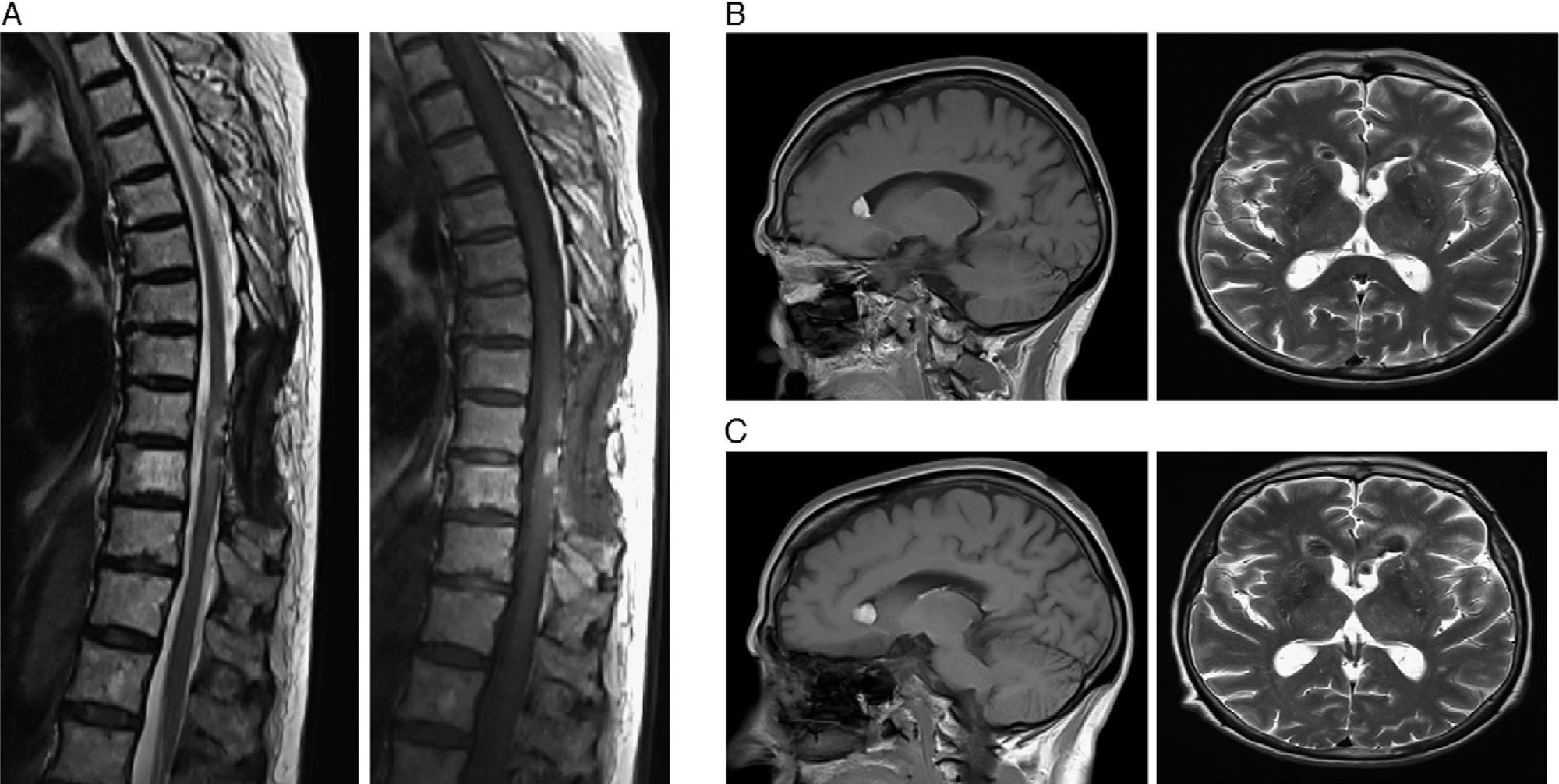
The patient was sent to our centre for rehabilitation treatment. We performed a study of motor evoked potentials of the tibialis anterior on both sides, which did not evoke a response. The SEPs of the lower limbs were also abolished, where they were delayed before. Consequently, she presented spinal cord injury syndrome D8 ASIA A on admission. The rehabilitation physician noticed a change in the patient's higher functions. We requested a neuropsychological study, where a moderate deterioration in all areas of the Barcelona test could be seen, with no specific profile of a degenerative disease. We performed a brain MRI, where we were surprised by several images indicative of ependymal implants in both anterior horns of the lateral ventricles, hyperintense in T1 sequence and hypointense in T2 (Fig. 1) without contrast enhancement, which did not correspond to blood-borne deposits in the sequence of magnetic susceptibility. In the control dorsal MRI, there were signs of myelopathy with traces of haemosiderin; at the boundary between D9 and D10 segments, we found a 1cm lesion located in the right posterolateral region of the spinal cord. Not captured by IVC, it was hyperintense in T1 and hypointense in T2, with radiological semiology characteristic of melanin (Fig. 1). The ependymal implants had doubled in size in the brain MRI after 1 month of evolution (Fig. 1), a fact that strengthened the diagnosis of rapidly progressing meningeal melanocytoma with seeding or a multifocal origin. Despite this, the patient remained clinically stable with not only her spinal cord lesion but also in her cognitive deficit during the 3 months that she stayed at our centre. In the end, she was sent to the oncology department of her reference hospital to be assessed for other treatment options.
(A) Sagittal T2 and sagittal T1 MRI: between segments D9 and D10, there is a 1-cm lesion situated in the right posterolateral area of the medulla, indicative of a melanin deposit. (B) Sagittal T1 and axial T2 MRI: images indicative of ependymal implants in both anterior horns of the lateral ventricles. (C) Sagittal T1 and axial T2 MRI: increase in the size of the ependymal implants.
Melanotic cells are derived from the neural crest during embryonic development; they are present in a healthy adult and are the origin for pigmented leptomeningeal tumours. Among these, melanocytoma originates in the spinal cord half the time.1 Although these tumours generally have a good prognosis when treated with a complete resection or incomplete surgery plus adjuvant radiotherapy, according to the series of cases with evolution at 5 years, the percentage of local relapses is not negligible; neither is the leptomeningeal progression and seeding, which are less frequent.2 In cases described on seeding, the primary location is in the posterior fossa, with implants at a spinal level.3,4 This can occur after a complete tumour resection and a period of clinically-stable years. This possibility was considered in the case presented, but it seemed improbable due to the short time of evolution between the surgery and the detection of cerebral lesions.
Despite the fact that in this case the pathological anatomy did not reveal malignancy, we saw rapid tumour progression, with a possible multifocal origin. This has been published on very few occasions; consequently, the prognosis is uncertain in this case. In references that have been found, it is attributed to a possible aggressive course and a bad prognosis.5,6 Finally, we would like to stress that we had previously considered a histological review of this tumour in order to modify the various treatment regimens and improve the outcome.
Please cite this article as: Ayuga Loro F, et al. Melanocitoma meníngeo con comportamiento maligno. Neurología. 2011;26:565–6.