Early-onset dementia (EOD) is defined as dementia with onset before the age of 65 years. EOD is increasingly recognised as an important clinical and social problem with devastating consequences for patients and caregivers.
ObjectiveDetermine the annual crude incidence rate and the specific incidence rates by sex and age in patients with EOD, and the standardised rate using the last national census of the population of Argentina (NCA), from 2010.
Materials and methodsHospital Privado de Comunidad, Mar del Plata, Argentina, attends a closed population and is the sole healthcare provider for 17614 people. Using the database pertaining to the Geriatric Care Department, we identified all patients diagnosed with EOD between 1 January 2005 and 31 December 2011. EOD was defined as dementia diagnosed in patients younger than 65.
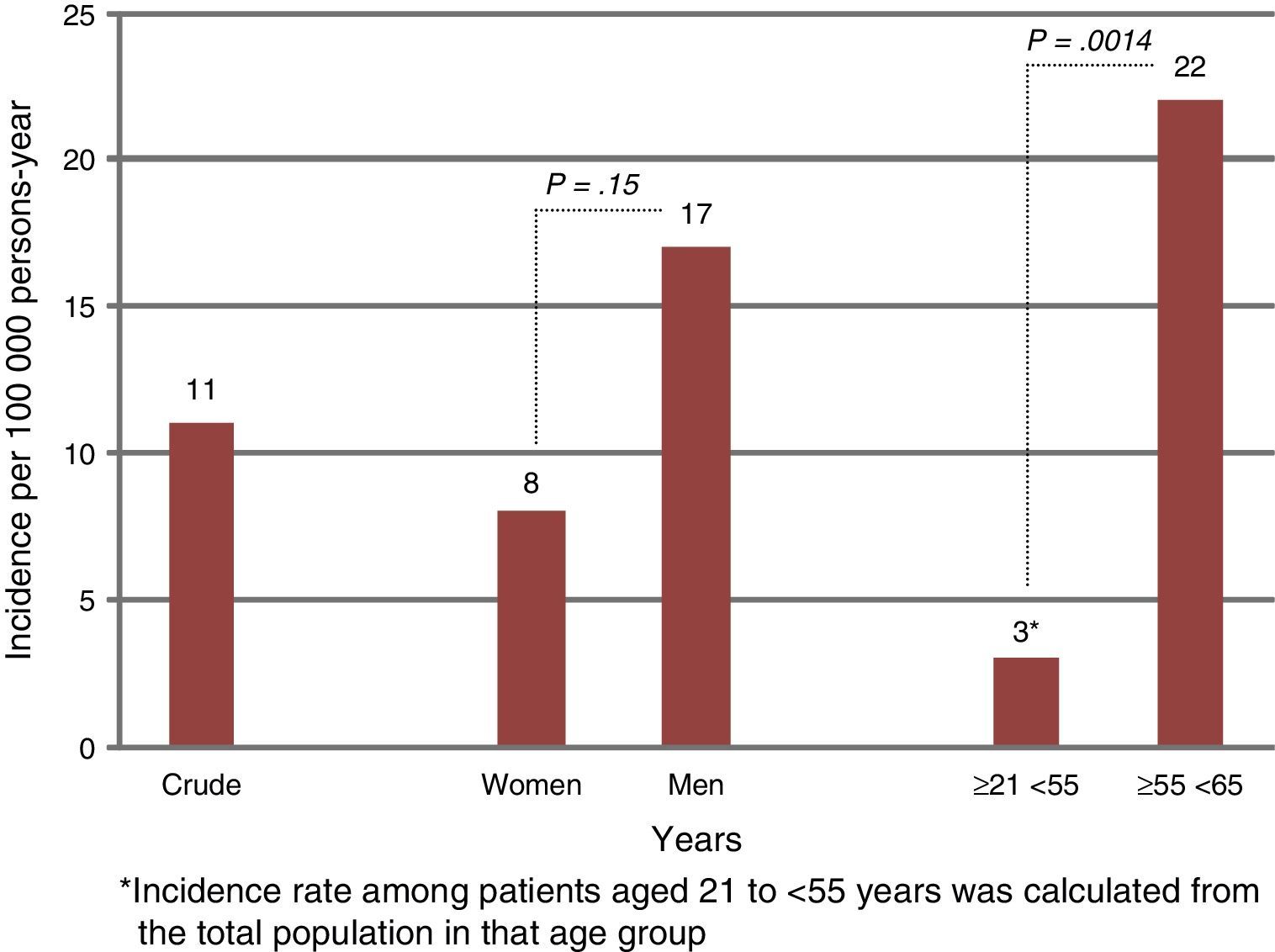
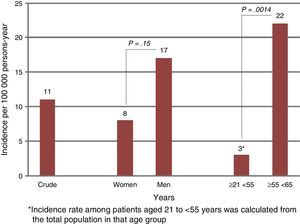
ResultsThe study period yielded 14 patients diagnosed with EOD out of a total of 287 patients evaluated for memory concerns. The crude annual incidence of EOD was 11 per 100000/year (CI 95%: 6.25-19.1): 17 per 100000 (CI 95%: 7.2-33.1) in men and 8 per 100000 (CI 95%: 3.4-17.2) in women. We observed a statistically significant increase when comparing incidence rates between patients aged 21 to <55 years and ≥55 to <65 years (3 vs 22 per 100000, P=.0014). The rate adjusted by NCPA census data was 5.8 cases of EOD inhabitants/year.
ConclusionThis study, conducted in a closed population, yielded an EOD incidence rate of 11 per 100000 inhabitants/year. To the best of our knowledge, this is the first prospective epidemiological study in Argentina and in Latin America.
La demencia de inicio precoz (DIP) se define como demencia con una edad de inicio antes de los 65 años. La DIP está siendo cada vez más reconocida como un importante problema clínico y social, con consecuencias devastadoras para los pacientes y para las personas que cuidan de ellos.
ObjetivoDeterminar la tasa de incidencia bruta anual y las tasas de incidencia específicas por sexo y edad de pacientes con DIP, y la tasa estandarizada al último Censo Nacional de Población de Argentina (CNPA) del año 2010.
Materiales y métodosEn el Hospital Privado de Comunidad, Mar del Plata, Argentina, se atiende a una población cerrada con atención médica exclusiva de 17.614 personas; de estos pacientes se extrajeron todos aquellos con diagnóstico de DIP, de la base de datos del Servicio de Atención a la Tercera Edad del hospital, desde el 1 de enero del 2005 hasta el 31 de diciembre del 2011. Se definió DIP a la demencia diagnosticada antes de los 65 años.
ResultadosDurante el período de estudio, se registraron 14 pacientes con diagnóstico de DIP, de un total de 287 pacientes evaluados por queja de memoria. La tasa de incidencia anual bruta de DIP fue de 11 por 100.000 habitantes/año (IC del 95%, 6,25-19,1), 17 por 100.000 (IC del 95%, 7,2-33,1) en hombres y de 8 por 100.000 (IC del 95%, 3,4-17,2) en mujeres. Se observó un incremento estadísticamente significativo al comparar las tasas de incidencia entre pacientes de 21 a < 55 años y ≥ 55 a < 65 años (3 vs. 22 por 100.000; p = 0,0014). La tasa ajustada al CNPA fue de 5,8 casos de DATE por 100.000 habitantes/año.
ConclusiónEl presente trabajo, basado en una población cerrada, mostró que la tasa de incidencia anual de DIP fue de 11 por 100.000 habitantes/año, y a nuestro saber constituye el primer estudio prospectivo epidemiológico en Argentina y América Latina.
Dementia in patients younger than 65 at onset is known as early-onset dementia (EOD).1,2 It is increasingly being acknowledged as an important clinical and social problem and its consequences are devastating for both patients and their carers.3
The literature contains only limited epidemiological data for EOD incidence since it is less frequent than late-onset dementia (LOD). The annual incidence rate of EOD according to studies conducted in Europe and the United States ranges between 7.2 and 29.6 per 100000 persons-year.4–8 However, there are no available epidemiological data on EOD incidence in Latin America, including Argentina.
Our aim is to perform a prospective epidemiological study of EOD incidence based on a closed population.
ObjectivesThis study aims to determine the crude annual incidence rate and specific incidence rates of EOD broken down by sex and age in a closed population receiving treatment exclusively at Hospital Privado de Comunidad in Mar del Plata, in Argentina.
We attempt to adjust or extrapolate these rates to the population registered by the Argentinian National Census of 2010.
Materials and methodsGeneral populationHospital Privado de Comunidad in Mar del Plata provides care to a population registered with the National Institute of Social Services for Retirees and Pensioners (INSSJP). This population is treated in our hospital exclusively within the framework of a capitation system. This system is applicable to both primary care and highly specialised care. It delivers a single medical history for each patient, and diagnoses that are coded and recorded in a computer database. Capitation in Argentina is a medical service financing system by which union-run insurance organisations pay a monthly per-patient fee to a healthcare provider. In exchange, patients receive healthcare services that have been previously approved. Cápita is the term referring to the set of individuals identified by contract as the beneficiaries of those services. In our case, this amounts to 6954 patients. Additionally, another 10660 individuals receive care as beneficiaries of prepaid healthcare plans (PHP). Therefore, our hospital provides care to a total of 17614 individuals, referred to here as our ‘closed population’. We gathered data from patients with coverage provided by the INSSJP and PHPs between 1 January 2005 and 31 December 2011. We also calculated the average values for each population, and stratified data according to sex and age.
Case reportsPatients with EOD were identified in the database of the gerontology department at our hospital. This department is responsible for the assessment, diagnosis, inpatient care, and treatment of patients with memory disorders. The department is staffed with geriatric specialists, neurologists, neurology residents, speech therapists, occupational therapists, kinesiotherapists, and physical trainers. Patients are referred to this department by primary care doctors, clinicians, or neurologists. Reasons for requesting assessment include subjective memory complaints or behaviour disorders related to memory impairment. All patients underwent clinical, neurological, and neuropsychological evaluation. Neurocognitive evaluation of patients younger than 65 years follows a standard protocol and includes the following tests: Mini-Mental State Examination,9 Clock Drawing Test (Cacho scoring method),10 Alzheimer's Disease Assessment Scale,11 Frontal Assessment Battery,12 semantic and phonological word fluency test,13 Rivermead Behavioural Memory Test,14 Stroop Test,15 Trail Making Test parts A and B,16,17 Clinical Dementia Rating,18 and Global Dementia Scale.19 The Barthel Activities of Daily Living Index,20 and Lawton's Instrumental Activities of Daily Living Scale were also used.21 No other supporting techniques, whether functional neuroimaging, or biochemical markers in cerebrospinal fluid, were used in diagnosis.
The final diagnosis was achieved by consensus among evaluators (gerontologist, neurologist and neuropsychologists). In cases in which no consensus was reached, the specialist with the most experience (D.S.) assigned the final diagnosis.
DefinitionsAlzheimer disease: diagnosis followed the criteria established by the National Institute of Neurological and Communicative Disorders and the Alzheimer's Disease and Related Disorders Association (NINCDS-ADRDA).22
Vascular dementia: diagnosed according to criteria established by the NINDS-AIREN International Workshop.23
Frontotemporal dementia: Lund and Manchester criteria24 were used.
Dementia with Lewy bodies: diagnosis followed the criteria established by the International Consortium on Dementia with Lewy Bodies.25
Depression: diagnosis followed the criteria included in the DSM-IV Diagnostic and Statistical Manual of Mental Disorders, fourth edition.26
EOD: onset of dementia before the age of 65.1–3,8
LOD: onset of dementia at age 65 or older.1–3,8
Arterial hypertension: defined as at least 2 measurements of systolic pressure ≥140 and/or diastolic pressure ≥90, or a history of antihypertensive treatment.27
High cholesterol-high triglycerides: the first term refers to a fasting value >200mg/dL, or high-density lipoprotein cholesterol <35mg/dL, in the presence or absence of low-density lipoprotein cholesterol >130mg/dL. The term ‘dyslipidaemia’ refers to high triglycerides (>150mg/dL) and any other type of polygenic or familial dyslipidaemia.28
Current tobacco use: consumption in the last 6 months. This condition is met if the patient smokes even occasionally, regardless of the amount and frequency.29
Diabetes: defined as 2 measurements of fasting glycaemia of ≥126mg/dL, or ≥200mg/dL in a non-fasting sample, or history of hypoglycaemic agents.30
Statistical analysisThe statistical analysis included descriptive statistics of the closed population and EOD patients as means (standard deviation), medians, and quartiles. To calculate the crude annual incidence rate of EOD, the closed population was the denominator and the patients diagnosed with EOD during the study period constituted the numerator. To identify any sex-linked differences between EOD incidence rates, we calculated the expected frequency for each sex stratified by age group (21-34, 35-44, 45-54, and 55-64 years). The chi-square goodness of fit test was used to test the null hypothesis that the frequency distribution is independent of sex (alpha <0.05). To identify differences in EOD incidence between age groups, we calculated the expected frequency for each age group stratified by sex; chi-square goodness of fit was used to test the null hypothesis that frequency distribution was independent of age (alpha <0.05). The 95% confidence interval (95% CI) was calculated using the Poisson distribution. Age-adjusted incidence rate was calculated using the latest national census of Argentina (NCA). We used Start Direct (version 2.7.2) for statistical analysis.
ResultsDemographical data- –
General population. Mean population was 17614 (61% women) for the period between 1 January 2005 and 31 December 2011 (Table 1).
- –
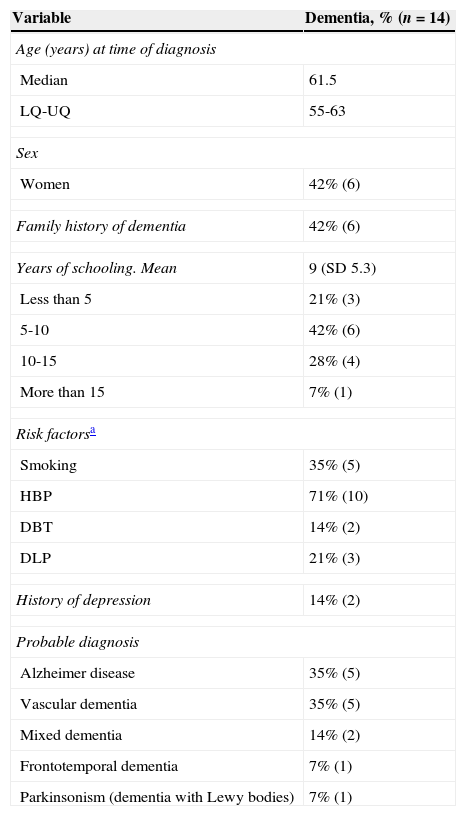
Study population. Fourteen patients diagnosed with EOD were identified out of the 287 patients aged 21-65 evaluated by the gerontology department during the study period. Mean age at diagnosis of EOD was 61.5 years; 42% were women. A total of 6 patients (42%) had a first-degree relative with probable dementia. Alzheimer disease was observed in 35% of the patients, as well as vascular dementia. Mixed dementia (vascular and degenerative dementia) was observed in 14%, whereas Lewy body dementia and frontotemporal dementia affected 17% of the EOD patients. Table 2 lists the remaining clinical, demographic, and aetiological characteristics.
Table 2.Population characteristics
Variable Dementia, % (n=14) Age (years) at time of diagnosis Median 61.5 LQ-UQ 55-63 Sex Women 42% (6) Family history of dementia 42% (6) Years of schooling. Mean 9 (SD 5.3) Less than 5 21% (3) 5-10 42% (6) 10-15 28% (4) More than 15 7% (1) Risk factorsa Smoking 35% (5) HBP 71% (10) DBT 14% (2) DLP 21% (3) History of depression 14% (2) Probable diagnosis Alzheimer disease 35% (5) Vascular dementia 35% (5) Mixed dementia 14% (2) Frontotemporal dementia 7% (1) Parkinsonism (dementia with Lewy bodies) 7% (1) LQ: lower quartile; UQ: upper quartile; SD: standard deviation.
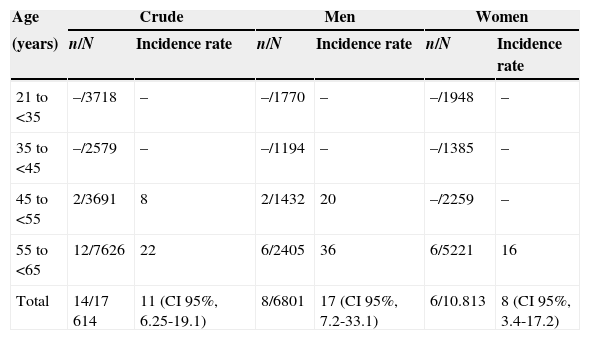
Crude annual incidence rate of EOD was 11 per 100000 persons-year (95% CI, 6.25-19.1), 17 per 100000 (CI 95%, 7.2-33.1) in men and 8 per 100000 (95% CI, 3.4-17.2) in women. This difference observed between sexes was not statistically significant. Table 3 lists relative incidence rates for age group and sex.
Annual crude and relative incidence rates of EOD per 100000 persons-year, distributed by sex and age
| Age | Crude | Men | Women | |||
|---|---|---|---|---|---|---|
| (years) | n/N | Incidence rate | n/N | Incidence rate | n/N | Incidence rate |
| 21 to <35 | –/3718 | – | –/1770 | – | –/1948 | – |
| 35 to <45 | –/2579 | – | –/1194 | – | –/1385 | – |
| 45 to <55 | 2/3691 | 8 | 2/1432 | 20 | –/2259 | – |
| 55 to <65 | 12/7626 | 22 | 6/2405 | 36 | 6/5221 | 16 |
| Total | 14/17614 | 11 (CI 95%, 6.25-19.1) | 8/6801 | 17 (CI 95%, 7.2-33.1) | 6/10.813 | 8 (CI 95%, 3.4-17.2) |
CI: confidence interval.
A comparison of incidence rates among patients aged 21 to <55 years and patients aged ≥55 to <65 years (3 vs 22 per 100000), revealed a statistically significant increase (P=.0014) (Fig. 1).
The rate adjusted to the latest NCA, corresponding to 2010, was 5.8 EOD cases per 100000 persons-year.
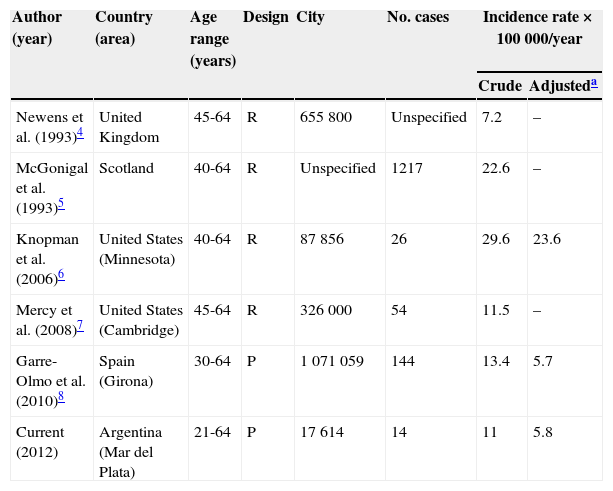
DiscussionWe identified only 5 articles on the incidence of early onset dementia in Europe and the United States.4–8 To our knowledge, ours is the first prospective epidemiological study for both Argentina and Latin America to have been published.
Our study is based on a closed population and it yielded an annual incidence rate of EOD of 11 per 100000 persons-year. Furthermore, we observed a statistically significant increase in this incidence rate with age.
Our results are similar to those published in other studies.4–8 The first of these studies, conducted in the United Kingdom, showed an incidence of early onset dementia of 7.2 per 100000 persons-year4; the second, limited to Scotland, yielded an incidence of 22.6 EOD cases per 100000 persons-year.5 The third study was carried out in Minnesota and showed an incidence rate of 29.6 cases per 100000 persons-year, demonstrating a clear increase in incidence with age.6 The fourth study, from Cambridge (USA), estimated an EOD incidence of 11.5 cases per 100000 persons-year.7 The last study, reporting an incidence of 13.4 cases per 100000 persons-year, was performed in Girona, Spain (ReDeGi Study Group) (Table 4).8
Adjustment and standardisation of measured rates using the latest Argentinian national census, corresponding to 2010
| Author (year) | Country (area) | Age range (years) | Design | City | No. cases | Incidence rate×100000/year | |
|---|---|---|---|---|---|---|---|
| Crude | Adjusteda | ||||||
| Newens et al. (1993)4 | United Kingdom | 45-64 | R | 655800 | Unspecified | 7.2 | – |
| McGonigal et al. (1993)5 | Scotland | 40-64 | R | Unspecified | 1217 | 22.6 | – |
| Knopman et al. (2006)6 | United States (Minnesota) | 40-64 | R | 87856 | 26 | 29.6 | 23.6 |
| Mercy et al. (2008)7 | United States (Cambridge) | 45-64 | R | 326000 | 54 | 11.5 | – |
| Garre-Olmo et al. (2010)8 | Spain (Girona) | 30-64 | P | 1071059 | 144 | 13.4 | 5.7 |
| Current (2012) | Argentina (Mar del Plata) | 21-64 | P | 17614 | 14 | 11 | 5.8 |
EOD incidence was age-dependent in our population, which displayed a statistically significant increase in patients aged ≥55 and <65 years, a pattern similar to that observed in the articles listed above.5–8 In the Girona study, incidence rates for the 40 to 49, 50 to 59, and 60 to 64 age groups, were 3.9, 22.9, and 67.7 cases per 100000 persons-year, respectively.8 In the Cambridge study, the incidence rate for subjects aged 45 to 64 was 11.5 cases per 100000 inhabitants;7 in the Minnesota study, incidence rates were 8.8, 22.9, and 125.9 cases per 100000 persons-year for subjects aged 40 to 49, 50 to 59, and 60 to 64, respectively.6
Incidence rate in our population adjusted to the last NCA was 5.8 EOD cases per 100000 persons-year (Table 4). Adjusting the EOD incidence rate to the NCA yields a far lower incidence rate (from 11 to 5.8 per 100000 persons-year) due to the high number of older patients (>55 years). This shows how important it is to consider the population's demographic characteristics when comparing incidence rates for an entity whose distribution is biased towards certain age groups. Therefore, when adjusting the rate from the Girona study8 to the NCA, we observe an incidence rate similar to our own at 5.7 cases per 100000 persons-year. For the Minnesota study,6 the rate adjusted to the NCA was 23.6 cases per 100000 persons-year; this high rate might be explained by the study's older age groups (all older than 40 years, unlike our population and that used in the Girona study), or because there may be a higher risk of EOD dementia in that population.
Our study presents several limitations. Firstly, it includes patients who attended consultations due to memory complaints, behavioural disorders, or language disorders. Since these patients had been referred by clinicians, neurologists, or geriatric specialists to be evaluated by our gerontology department, they may not be representative of the total number of patients with the disease. Such referrals are probably less common for EOD patients than for patients with LOD, since the late-onset variant has devastating consequences for patients and their families. Therefore, LOD is very unlikely to go unnoticed and patients will very probably receive medical attention. Secondly, during the study period, the evaluations performed by the gerontology department had fees attached, which might have decreased the number of consultations, and subsequently the incidence rate. For this reason, we compared the number of young patients who attended the hospital during the period in which evaluations were free of charge and concluded that consultation frequency was similar during both periods. Thirdly, the diagnostic criteria used in our study, and in earlier ones, had been validated for an elderly population, so their applicability to a younger population might be limited. Fourthly, the probable aetiologies given for EOD cases should be considered with caution, since they were not confirmed by a pathology study. Furthermore, several overlapping diseases may be associated.
However, our study also presents several strong points: the included patients belonged to a geographically well-defined population and they were all evaluated using a standard procedure in a single hospital. Cases were collected prospectively, which minimises the number of possible missing cases. Indirect markers of appropriate monitoring consisted of the increasing incidence rate of EOD with age and the annual crude rate, as shown by prior studies.
Dementia is a source of great hardship for patients, their families, and society, and gathering epidemiological information is therefore essential to developing healthcare policies applicable to this situation.
Epidemiological studies of EOD incidence should be based on large at-risk populations because of the rareness of the disease. For this reason, most of the studies of dementia in younger patients published to date have been prevalence studies.
Our aim was to calculate EOD incidence rate in a closed population from the town of Mar del Plata in order to obtain consistent epidemiological results and compare them with results from prior studies performed in other towns around the world. To our knowledge, this is the first prospective epidemiological study to be performed in Argentina and in Latin America.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sanchez Abraham M, Scharovsky D, Romano LM, Ayala M, Aleman A, Sottano E, et al. Incidencia de demencia de inicio precoz en Mar de Plata. Neurología. 2015;30:77–82.