Since the beginning of the COVID-19 pandemic, the Spanish Society of Neurology has run a registry of patients with neurological involvement for the purpose of informing clinical neurologists. Encephalopathy and encephalitis were among the most frequently reported complications. In this study, we analyse the characteristics of these complications.
Patients and methodsWe conducted a retrospective, descriptive, observational, multicentre study of patients with symptoms compatible with encephalitis or encephalopathy, entered in the Spanish Society of Neurology's COVID-19 Registry from 17 March to 6 June 2020.
ResultsA total of 232 patients with neurological symptoms were registered, including 51 cases of encephalopathy or encephalitis (21.9%). None of these patients were healthcare professionals. The most frequent syndromes were mild or moderate confusion (33%) and severe encephalopathy or coma (9.8%). The mean time between onset of infection and onset of neurological symptoms was 8.02 days. Lumbar puncture was performed in 60.8% of patients, with positive PCR results for SARS-CoV-2 in only one case. Brain MRI studies were performed in 47% of patients, with alterations detected in 7.8% of these. EEG studies were performed in 41.3% of cases, detecting alterations in 61.9%.
ConclusionsEncephalopathy and encephalitis are among the complications most frequently reported in the registry. More than one-third of patients presented mild or moderate confusional syndrome. The mean time from onset of infection to onset of neurological symptoms was 8 days (up to 24hours earlier in women than in men). EEG was the most sensitive test in these patients, with very few cases presenting alterations in neuroimaging studies. All patients treated with boluses of corticosteroids or immunoglobulins progressed favourably.
Desde el inicio de la pandemia por el virus SARS-CoV2 la Sociedad Española de Neurología (SEN) creó un registro de afectación neurológica para informar al neurólogo clínico. Las encefalopatías y encefalitis fueron una de las complicaciones más descritas. Analizamos las características de las mismas.
Pacientes y métodosEstudio descriptivo retrospectivo, observacional multicéntrico, de pacientes con sintomatología compatible con encefalitis o encefalopatía, introducidos en el Registro SEN COVID-19 desde el 17 de marzo hasta el 6 de junio de 2020.
ResultadosSe han registrado 232 casos con síntomas neurológicos, 51 casos de encefalopatía/encefalitis (21,9%). Ningún paciente era trabajador sanitario. Los síndromes más frecuentes fueron: cuadro confusional leve-moderado (33%) y encefalopatía grave o coma (9,8%). El tiempo medio entre el inicio de la infección y la clínica neurológica fue de 8,02 días. Punción lumbar en el 60,8% de pacientes; solo hubo un caso con PCR positiva. Resonancia craneal en el 47% de los pacientes (alterada en el 7,8% de ellos). Se realizó electroencefalograma en el 41,3% de los casos (alterado en el 61,9% de los mismos).
ConclusionesLas encefalopatías y encefalitis son dos de las complicaciones más frecuentes descritas en el SEN COVID-19. Más de un tercio de los pacientes presentó un cuadro de síndrome confusional leve o moderado. El tiempo medio de aparición de la sintomatología neurológica desde el inicio de la infección fue de 8 días (hasta 24h antes en mujeres que en hombres). El electroencefalograma fue la prueba más sensible en estos pacientes, encontrando muy pocos casos con alteraciones en las pruebas de neuroimagen. Todos los pacientes que recibieron tratamiento con bolos de corticoides o inmunoglobulinas tuvieron una evolución favorable.
Coronavirus disease 2019 (COVID-19), caused by the SARS-CoV-2 virus, was first described in China in December 2019, and subsequently spread to other continents. The World Health Organization considered the disease a public health emergency of international concern on 30 January 2020, and declared an international pandemic on 11 March.1 The first cases in Spain were reported on 31 January 2020,2 and by March there were over a thousand cases. At the time of writing (6 June 2020), a total of 241310 confirmed cases of COVID-19 and 27135 deaths had been reported in Spain.3
Besides the predominant respiratory symptoms, the virus can also cause a series of systemic complications, with nervous system involvement being particularly frequent (30%-60%, according to different series).4–7 Neurological manifestations include a wide range of symptoms and complications that favour higher mortality and morbidity rates.
Recent studies have reported series of patients with anosmia or dysgeusia,8 as well as cases of cerebrovascular disease associated with prothrombotic alterations (stroke, intraparenchymal haemorrhage, venous thrombosis, etc) caused by the infection.9–18 Cases have also been described of headache, encephalitis, vasculitis, myopathy, and Guillain-Barré syndrome.19–32
Encephalopathy is defined as alteration of one or more brain functions (altered level of consciousness, seizures, confusional state, acute focal deficits) caused by a systemic disease (anoxia, ischaemia, metabolic disorders, etc), and is typically reversible.33–42
Encephalitis is characterised by typically focal brain alterations, with or without meningeal involvement, with different possible causes (infectious, inflammatory, autoimmune, paraneoplastic, etc), and can be confirmed with histology studies or through the detection of inflammatory cells in the cerebrospinal fluid (CSF).43 The clinical features are fever, headache, and symptoms of brain dysfunction. While infectious aetiology is common, diagnosis of other causes, including autoimmunity, is becoming increasingly frequent.
The Spanish Society of Neurology (SEN) created a national registry of neurological complications in patients with SARS-CoV-2 infection, in order to provide information for clinical neurologists. The aim of the project was to contribute to the knowledge of these entities and to assist in their early diagnosis in order to minimise mortality, morbidity, and sequelae. Encephalopathy and encephalitis are 2 of the most frequently reported complications. In this study, we analyse the cases included in the registry.
Patients and methodsWe performed a descriptive, observational, retrospective, multicentre study of patients presenting symptoms compatible with encephalopathy or encephalitis and recorded in the SEN's COVID-19 registry between 17 March and 6 June 2020, inclusive.
During this period, the registry was available through the SEN's website and could be accessed by all members of the Society. Each participating neurologist completed a questionnaire with 42 sections.
To enable more detailed statistical analysis, the total dataset was subsequently divided according to syndrome (headache, anosmia, cerebrovascular disease, neuromuscular disease, epilepsy, and encephalopathy/encephalitis).
The data collected were: name of the informing neurologist, e-mail address, type of SEN membership, reference hospital, autonomous community, patient age and sex, general comorbidities, neurological comorbidities, past pharmacological treatments, epidemiology of infection (healthcare worker, identifiable source of transmission), time between first general symptom and first neurological symptom, symptoms of COVID-19, COVID-19 syndrome, method of diagnosis of infection, description of neurological symptoms, description of neurological examination, neurological syndrome, laboratory findings, intensive care unit (ICU) admission, intubation, lumbar puncture, CSF analysis, head computed tomography (CT) study, brain or lumbar spine magnetic resonance imaging (MRI) study, electroencephalography (EEG) study, electroneuromyography study, chest CT study, informing neurologist's judgement of the likelihood that neurological symptoms were caused by COVID-19, antiviral treatments administered, neurological treatments administered, clinical progression, and duration of neurological manifestations.
For the variable “neurological syndrome,” participating neurologists were prompted to distinguish between encephalopathy and encephalitis by selecting one of the following options from a drop-down list: encephalitis, severe encephalopathy/coma, status epilepticus, seizures, mild/moderate confusion, or a combination of several of the above. An open-ended variable (description of neurological symptoms) was also included so that respondents could specify further clinical details or symptoms they considered relevant (headache, ataxia, aphasia, etc).
All information gathered in the database, the causal role of the infection, and complementary study findings were described by the informing neurologist. Most items were open-ended, whereas others used multiple-choice drop-down lists. While nearly all items were completed by the participating neurologists, not all data were supplied for some variables, such as laboratory data (CSF protein levels, interleukins, D-dimer, etc); it is unclear whether this is because these tests were not conducted or because laboratory data were not available at the time of data input. The number of informing neurologists, the number of items included in the questionnaire, and the heterogeneity of the data complicated the analysis of the results, and result in some limitations.
Data were gathered and processed as an anonymised, grouped dataset. We conducted a statistical analysis of complete cases using SPSS version 25.0 (IBM). Categorical variables are expressed as frequencies and percentages, and continuous variables as mean (standard deviation [SD]). The chi-square test was used to establish associations between qualitative variables, and the t-test was used for quantitative variables.
The study was approved by the research ethics committee of the Valladolid Este healthcare district (project no. PI 20-1722).
ResultsThe SEN's COVID-19 registry includes data for a total of 232 patients with neurological symptoms, including 51 cases (21.9%) of encephalitis or encephalopathy. The registry also included 39 cases (16.8%) of anosmia, 30 cases (12.9%) of headache, 26 cases (11.2%) of epilepsy, 61 cases (26.2%) of neuromuscular disorders, and 55 cases (23.7%) of cerebrovascular disease.
We present results for the 51 patients with encephalopathy or encephalitis.
Epidemiological dataCases of encephalopathy or encephalitis were recorded in 10 autonomous communities: 18 (35.3%) in the region of Madrid, 7 (13.72%) in Catalonia, 5 (9.8%) in the Basque Country, 4 (7.8%) in Navarre, 4 (7.8%) in the Valencian Community, 4 (7.8%) in Castile-Leon, 3 (5.9%) in Aragon, 2 (3.9%) in Castile-La Mancha, 2 (3.9%) in the Balearic Islands, one (2%) in Extremadura, and one (2%) in Asturias.
Regarding demographic data, 30 patients (58.8%) were men and 21 (41.2%) were women; mean age (SD) was 69.1 years (10.2), with an age range of 39-94 years. None of the patients were healthcare professionals.
General comorbidities were very frequent (38 patients; 74.5%), particularly history of arterial hypertension (15; 29.5%). Neurological comorbidities were recorded in 15 patients (29.4%), with the most frequent being epilepsy (4 patients; 7.8%), cognitive impairment of different degrees of severity (4; 7.8%), and history of stroke (4; 7.8%).
The source of SARS-CoV-2 transmission was unknown in most cases (35 patients; 68.6%); the most frequent known sources of transmission were family members or partners (4; 7.8%) and social or public gatherings (4; 7.8%).
Respiratory and neurological symptomsThe most frequent COVID-19 syndrome was bilateral pneumonia (21 patients; 41%), flu-like symptoms (15; 29.6%), and pneumonia with acute respiratory distress syndrome (7; 14%). Thirteen patients (25.5%) required admission to the ICU.
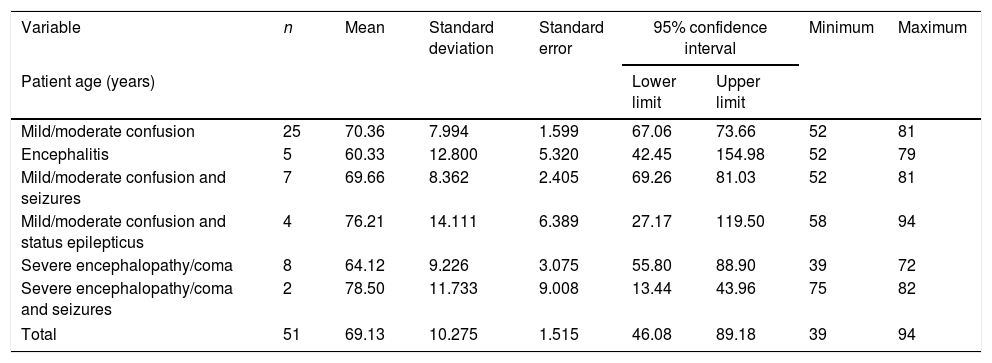
The most frequent neurological signs were mild or moderate confusion (25 patients; 49%), severe encephalopathy or coma (8; 15.7%), mild or moderate confusion and seizures (7; 14%), encephalitis (5; 10%), mild or moderate confusion and status epilepticus (4; 7.8%), and severe encephalopathy or coma and seizures (2; 3.9%) (Table 1).
Relationship between age and neurological syndrome.
| Variable | n | Mean | Standard deviation | Standard error | 95% confidence interval | Minimum | Maximum | |
|---|---|---|---|---|---|---|---|---|
| Patient age (years) | Lower limit | Upper limit | ||||||
| Mild/moderate confusion | 25 | 70.36 | 7.994 | 1.599 | 67.06 | 73.66 | 52 | 81 |
| Encephalitis | 5 | 60.33 | 12.800 | 5.320 | 42.45 | 154.98 | 52 | 79 |
| Mild/moderate confusion and seizures | 7 | 69.66 | 8.362 | 2.405 | 69.26 | 81.03 | 52 | 81 |
| Mild/moderate confusion and status epilepticus | 4 | 76.21 | 14.111 | 6.389 | 27.17 | 119.50 | 58 | 94 |
| Severe encephalopathy/coma | 8 | 64.12 | 9.226 | 3.075 | 55.80 | 88.90 | 39 | 72 |
| Severe encephalopathy/coma and seizures | 2 | 78.50 | 11.733 | 9.008 | 13.44 | 43.96 | 75 | 82 |
| Total | 51 | 69.13 | 10.275 | 1.515 | 46.08 | 89.18 | 39 | 94 |
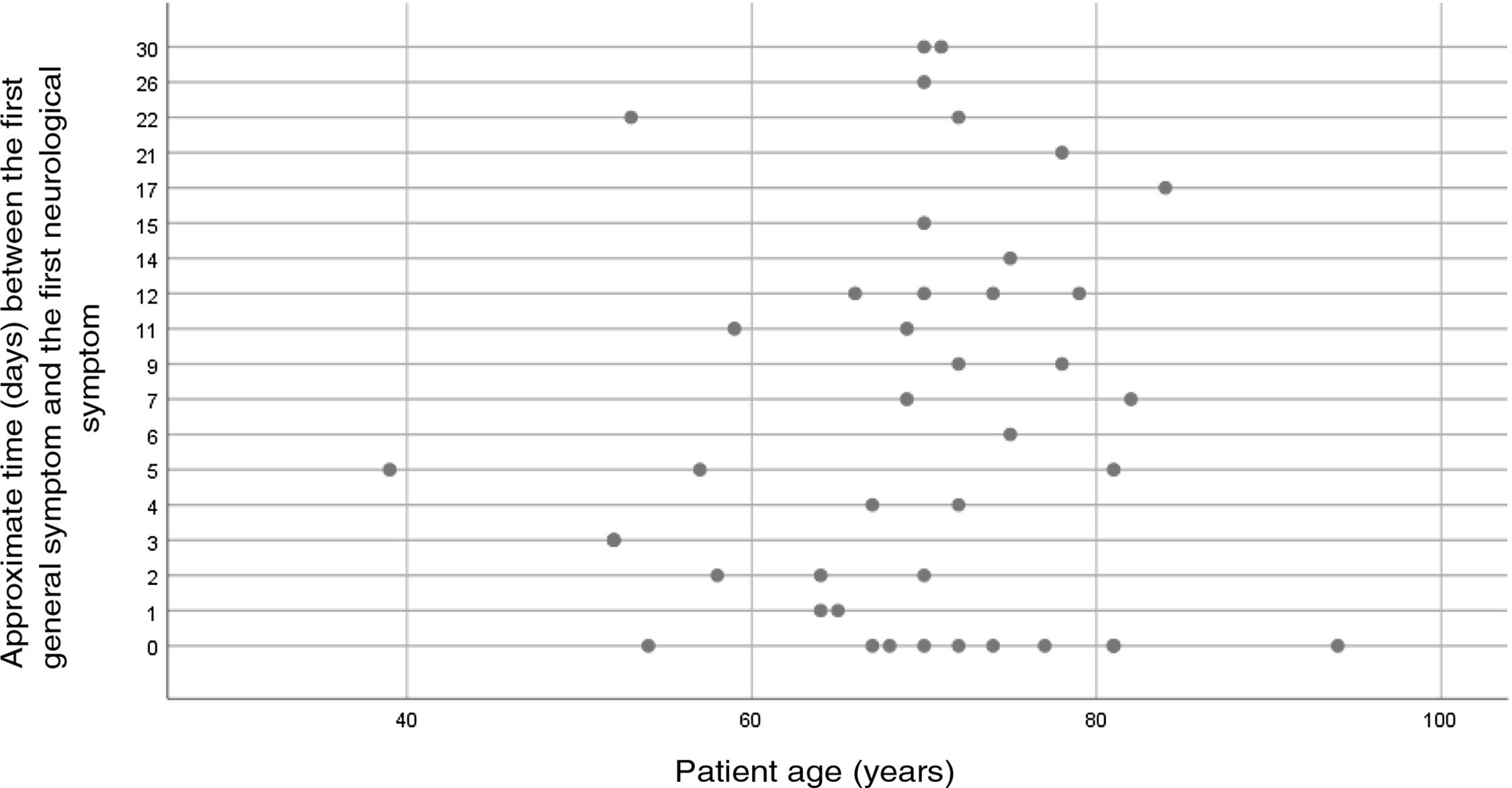
Mean time between onset of the respiratory infection and onset of neurological symptoms was 8.02 (8.57) days (range, 0-30). Neurological symptoms appeared at 7.41 (7.54) days (P=.02) in women and at 8.42 (9.31) days (P=.04) in men.
Complementary testsIn the cases for which laboratory data were available, the most frequent findings were increased C reactive protein level (29 patients; 52.9%), increased D-dimer level (27; 52.9%), lymphocytopaenia (24; 47%), and increased erythrocyte sedimentation rate (27; 52.9%).
Lumbar puncture was performed in 31 cases (60.8%), detecting alterations in 10 (19.6%): 6 with high CSF protein levels and 4 with high protein levels plus pleocytosis; pleocytosis in isolation was not detected in any patient. PCR returned positive results for SARS-CoV-2 in the CSF of a single patient. PCR testing of CSF was not performed in 10 patients (19.6%) due to lack of resources. No data are available on CSF interleukin levels or other microbiological cultures.
Neuroimaging studies were performed in 48 patients (94.1%).
Forty-six patients (90.2%) underwent head CT studies, with alterations detected in 12 (23.5%): 5 with acute lesions (3 patients with intraparenchymal haemorrhages, one with subacute infarct, and one with post-ictal diffuse oedema) and 8 with chronic lesions (7 with lacunar infarcts and one with hygromas).
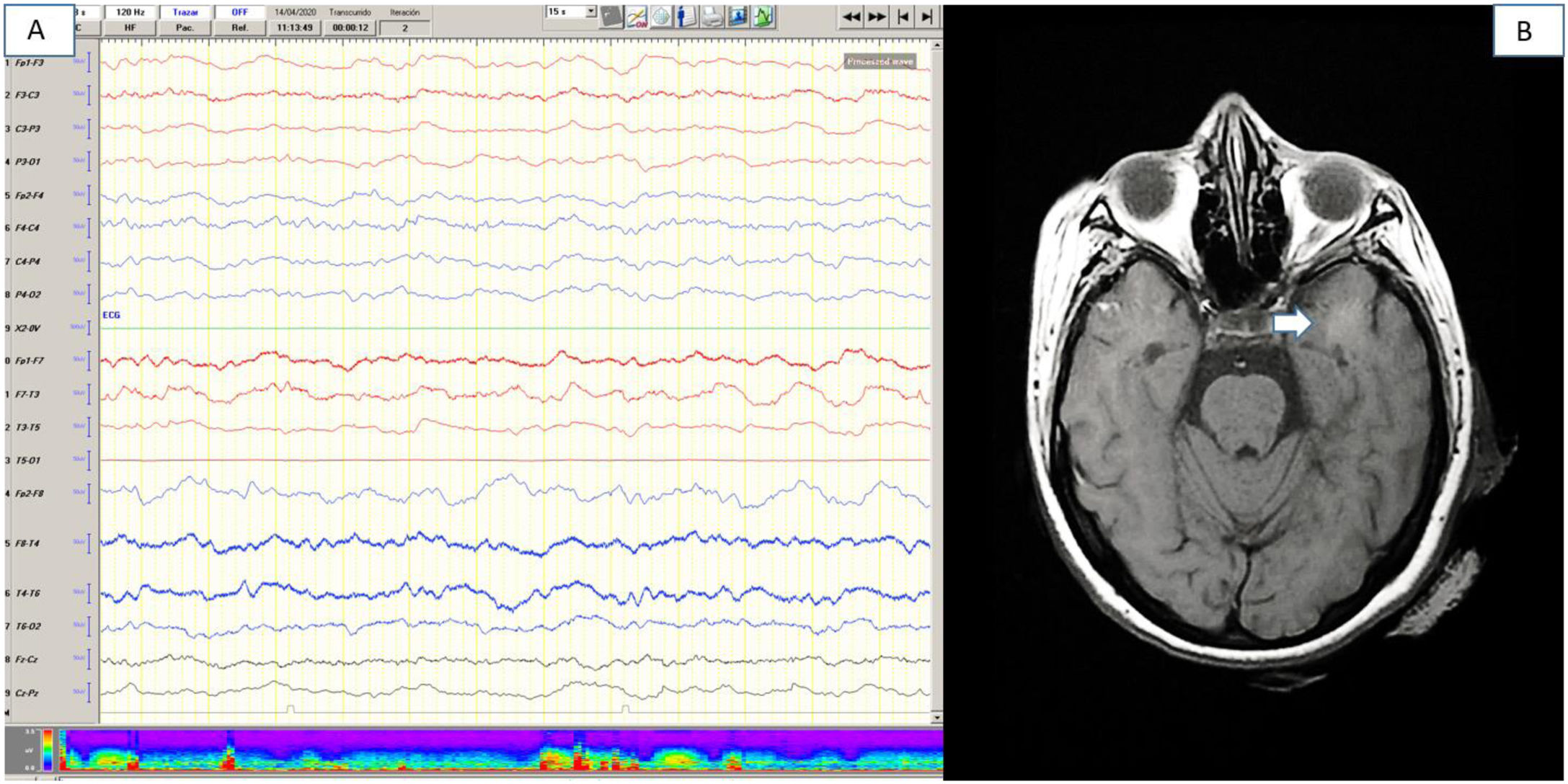
Brain MRI studies were performed in 18 patients (35.3%), detecting alterations in 8 cases (15.7%). Four patients (7.3%) presented acute vascular alterations (2 with acute lacunar infarcts, one with subacute frontal haemorrhage, and one with diffuse microbleeds in the white matter). In a further 4 patients (7.81%), MRI revealed white matter hyperintensities, mainly in temporal and mesencephalic regions (Fig. 1). Three of these 4 patients presented mild or moderate confusional symptoms. The number of patients in whom MRI diffusion sequences were performed is unclear.
EEG was performed in 16 patients (31.3%), with findings suggestive of mild or moderate diffuse encephalopathy in 10 cases (Fig. 1); 3 of these patients also displayed epileptiform EEG abnormalities.
Treatment and progressionThe specific treatments administered for SARS-CoV-2 were chloroquine or hydroxychloroquine plus lopinavir/ritonavir in 31 cases (60.7%), interferon beta 1b in 9 (17.6%), tocilizumab in 8 (15.6%), methylprednisolone boluses in 4 (7.8%), remdesivir in one (2%), and tenofovir in one (2%). Two patients (3.9%) received no treatment.
The specific neurological treatments administered were as follows:
- 1.
Antiepileptic drugs: levetiracetam (13 patients; 25.4%), clonazepam (2; 3.9%), lamotrigine (1; 2%), lacosamide (1; 2%), and eslicarbazepine acetate (1; 2%).
- 2.
Corticosteroids: methylprednisolone boluses for neurological symptoms (4 patients; 7.8%).
- 3.
Antivirals: aciclovir (3 patients; 5.8%).
- 4.
Immunoglobulins (2 patients; 3.9%).
Progression was favourable or stable in 27 cases (53.1%); 10 patients (19.6%) remained completely asymptomatic, 8 patients (15.6%) presented complications or progressive worsening, and 6 patients (11.7%) died.
According to the informing neurologist's judgement, the causal role of COVID-19 in neurological symptoms was coincidental in 15.8% of cases, probable in 74.5%, and definite in 9.8%.
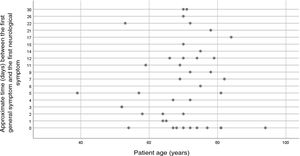
The comparative analysis identified no statistically significant association between mean age and ICU admission (mean [SD]: 68.8 [10.3]; 95% confidence interval [CI], 65.7-71.9; P=4.503), neurological syndrome and ICU admission (mean: 1.02 [1.55]; 95% CI, 0.582-1.457; P=4.681), or age and symptom progression time (mean: 60.9 [13]; 95% CI, 56.976-64.978; P=3.756) (Fig. 2).
Patients with encephalitis were younger than patients with other neurological syndromes (mean: 60.3 [12.8] years; P=1.82), whereas patients with severe encephalopathy and seizures were older (mean: 78.5 [11.7] years; P=2.29) (Table 1).
DiscussionSince the beginning of the COVID-19 pandemic, it has become clear that the characteristic respiratory symptoms are often accompanied by neurological symptoms, both in mild and in more severe cases.5–15
Since that early juncture, the SEN has made it possible, through its website, to enter data on patients with neurological manifestations, in order to create a multicentre registry to improve understanding of complications of the infection. The registry collects data on a broad range of variables, mostly using open-ended questions; this complicated the statistical analysis but provided additional value, enabling collection of a large amount of data and consideration of different hypotheses.
Encephalopathy and encephalitis were 2 of the most frequently reported syndromes in the registry and in ongoing national and international series of patients with neurological complications.33–42 We categorised the information recorded by the informing neurologists with a view to homogenising the data.
From an epidemiological viewpoint, the series showed a predominance of men (58.8%), as is the case in the majority of series published, and the age range of patients was very broad. Curiously, none of the patients was a healthcare worker, despite up to 21%-30% of hospital and health centre staff having been affected by the disease.44–48 Data were recorded in 10 autonomous communities. While this is a multicentre study, it presents a clear risk of selection bias: many hospitals (especially tertiary-level hospitals) created their own registries, with few participating in the SEN registry; therefore, our sample size is smaller than desired.
Most patients presented comorbidities, with a quarter presenting history of neurological disorders; other series report somewhat lower rates.8–18 In most cases the source of transmission of SARS-CoV-2 could not be determined.
Regarding clinical symptoms, of the 51 patients presenting encephalopathy or encephalitis, 46 presented encephalopathy of differing degrees of severity and 5 presented encephalitis, according to the informing neurologist. The most frequent symptoms were confusion (mild, moderate, or severe), seizures or status epilepticus, and coma. While these symptoms are frequently associated with both entities, these data may also be influenced by the fact that some patients had history of cognitive impairment or epilepsy.
The mean time from onset of respiratory symptoms to onset of neurological symptoms was 7-8 days, coinciding with the critical period of the respiratory infection (days 7-10). This suggests that confusional symptoms may be related to the progression of the respiratory disease (hypercapnic encephalopathy), the appearance of complications affecting other organs (uraemic/hepatic encephalopathy, etc), or progression of the systemic inflammatory reaction (“cytokine storm”). Neurological symptoms appeared up to 24 hours earlier in women than in men.
Of the 28 patients who underwent lumbar puncture, PCR only detected SARS-CoV-2 in the CSF of one patient. These data, which are consistent with those reported in recent publications,34 suggest that CSF involvement may be secondary to the inflammatory phase of the infection (cytokine release), with encephalopathy resulting from diffuse effects of inflammation on the nervous system, rather than direct infection of the brain parenchyma. Due to an initial lack of resources, access to CSF PCR testing was limited, hence the small amount of data on this parameter. We also lack sufficient information on inflammatory markers in the CSF of patients who underwent lumbar puncture to evaluate the influence of the systemic inflammatory reaction.
Regarding imaging studies, nearly all patients underwent CT or MRI, depending on their respiratory status. Most of the MRI alterations detected were small vascular lesions, with radiological signs of encephalopathy only being observed in 4 cases, 2 of whom required ICU admission due to severe respiratory symptoms. Three of these patients presented good progression, remaining asymptomatic; clinical signs did not correlate with the grade of the radiological lesion.
While radiological studies presented poor sensitivity and specificity for detecting these entities, we did observe better performance for EEG, with results suggestive of mild or moderate encephalopathy in nearly half of patients.
The patients reported in the series received the main drugs used in Spain at the beginning of the pandemic (initially hydroxychloriquine and subsequently lopinavir/ritonavir, tocilizumab, corticosteroids, etc), in line with the developing knowledge of the disease. The main specific neurological treatments administered were antiepileptic drugs and corticosteroids. Only 2 patients received immunoglobulins, with both showing good progression.
Most patients progressed favourably. All patients who received methylprednisolone boluses or immunoglobulins (n=6) progressed favourably, which suggests that these drugs were able to improve the systemic inflammatory reaction, and that this was causing the neurological symptoms. However, this patient group represents a small proportion of the complete series, and we were unable to analyse other factors that may have influenced prognosis (drugs tried previously, lumbar puncture findings, etc). Co-presence of COVID-19 and neurological symptoms was only described as “coincidental” (in the view of the informing neurologist) in 15.8% of cases.
In the great majority of cases, the informing neurologist considered SARS-CoV-2 infection to be directly related to the appearance of neurological symptoms, either due to direct viral infection or due to the systemic inflammatory reaction and resulting metabolic alterations. The fact that PCR only detected the virus in the CSF of one patient also supports this hypothesis, and is consistent with the findings of recent studies.37
The patient with positive PCR results for SARS-CoV-2 in the CSF had history of dementia and was living in a nursing home; the head CT study only identified 2 old ischaemic lesions (right parietal and left occipital regions). The EEG study showed diffuse slowing, with epileptiform abnormalities in the right hemisphere, which may have been related to the sequelae of the previous stroke.
The limitations of this study include the risk of selection bias, mentioned above, as well as the fact that diagnosis and the assessment of causality were based on the subjective view of the participating neurologists, the lack of data on certain variables (particularly laboratory data) in such a comprehensive database, and the high number of patients who did not undergo brain MRI due to their respiratory status. Complete CSF studies are also available in few cases, as several patients did not undergo lumbar puncture, or because PCR testing for SARS-CoV-2 was not performed due to a lack of resources.
The strengths of the study include its multicentre approach and the large number of variables analysed, which provided a large dataset. While the data are very heterogeneous, we were able to perform a detailed descriptive study and assess several hypotheses based on the information provided.
ConclusionsEncephalopathy and encephalitis are 2 of the most frequently reported complications in the SEN's COVID-19 registry. The most frequent symptom was mild or moderate confusion, observed in more than one-third of patients. Mean time from infection to onset of neurological symptoms was 8 days, with neurological symptoms developing up to 24 hours earlier in women than in men. EEG was the most sensitive diagnostic test, with very few patients showing specific alterations in neuroimaging studies. All patients receiving treatment with corticosteroid boluses or immunoglobulins presented favourable progression. Encephalopathy and encephalitis were probably associated with SARS-CoV-2 infection, with the systemic inflammatory reaction to the infection causing these symptoms.
Conflicts of interestThe authors have no conflicts of interest to declare.
Dr Hortensia Alonso Navarro, Dr Teresa Mateos Salas, Dr María Fuensanta Valero García, Dr Fernando Morejón Burguillos, Dr Alejandra Collía Fernández, Dr Juan Carlos García Moncó, Dr Ana del Villar Igea, Dr Sergio Borja Andrés, Dr Eva Fernández Díaz, Dr Jéssica Fernández Domínguez, Dr Beatríz Martínez Menéndez, Dr Cristina Guijarro Castro, Dr Elsa Puiggros Rubiol, Dr Iago Payo Froiz, Dr María Rabasa Pérez, Dr Noelia González Nafría, Dr Jesús Porta Etessam, Dr Esteban Peña Llamas, Dr Jose Carlos Roche Bueno, Dr Misericòrdia Floriach Robert, Dr Victoriano Romero Cantero, Dr Guillermo Hernández Pérez.
Please cite this article as: Abenza Abildúa MJ, Atienza S, Carvalho Monteiro G, Erro Aguirre ME, Imaz Aguayo L, Freire Álvarez E, et al. Encefalopatías y encefalitis durante la infección aguda por SARS-CoV2. Registro de la Sociedad Española de Neurología SEN COVID-19. Neurología. 2021;36:127–134.