Equine therapy, an intervention method that has been practiced for decades around the world, is used to treat patients susceptible to psychomotor delays.
ObjectivesWe examine development of gross motor function compared to other psychomotor skills in patients undergoing this therapy, and analyse how this improvement affects general health status and quality of life.
Material and methodsThe study includes 11 children with delayed psychomotor development (aged 8.82±3.89; 6 boys, 5 girls). The main study variables were gross motor function (GMFM-88) and perceived quality of life (Pediatric Quality of Life Inventory, PedsQL). Three measurements were performed: before and after a period of inactivity, and once again 2 months after the second measurement, following completion of a sustained period of therapy.
ResultsWe observed significant differences in overall results on the GMFM-88 between the initial and final tests and between the intermediate and final tests. Regarding the PedsQL quality of life scale, no statistically significant results were recorded.
ConclusionsNoticeable changes in motor control were recorded throughout the course of the intervention, which suggests that equine therapy may be appropriate treatment in cases of delayed psychomotor development.
Las terapias ecuestres constituyen un método de intervención para usuarios susceptibles de presentar limitaciones en el ámbito psicomotor que se lleva practicando varias décadas en todo el mundo.
ObjetivosRealizar un estudio de pacientes beneficiarios de esta terapia en los logros obtenidos en la función motora gruesa en relación con el resto de las habilidades psicomotrices y cómo esta mejora influye en el estado general y en su calidad de vida.
Material y métodosSe incluyó a 11 niños (8,82±3,89; 6 niños, 5 niñas) con retraso psicomotor. Las variables principales de estudio fueron la función motora gruesa (GMFM-88) y la percepción de calidad de vida (Pediatric Quality of Life Inventory; PedsQL). Se realizaron 3 mediciones, antes y después de un periodo de inactividad, y 2 meses después de la segunda valoración, tras un periodo continuado de tratamiento.
ResultadosSe observó una diferencia significativa entre los resultados globales de la GMFM-88 entre las pruebas inicial-final e intermedia-final. Respecto a la escala de calidad de vida PedsQL, no se han observado resultados estadísticamente significativos.
ConclusionesA lo largo de la intervención, se han observado cambios evidentes en el control motor, por lo que parece que la terapia ecuestre puede ser una terapia adecuada para la intervención del retraso psicomotor.
Psychomotor development is considered a key factor in a child's adaptation to his or her environment. The starting point for psychomotor development is constructing the body scheme, that is, organising one's bodily sensations with regard to the environment. At about 2 years of age, children start to show awareness of their setting and relate to the outside world. This stage is pivotal for their futures: stimulus deprivation, whether due to external causes or to CNS dysfunction, may have a negative impact on a child's development and consequently on his or her adaptation to the environment.1 Psychomotor development includes such areas as body scheme and image, laterality, dynamic and visuomotor coordination, balance, motor dissociation, muscle tone/posture control, and spatial-temporal orientation.2
Psychomotor retardation, or psychomotor development disorder, is a term used to describe children with a low level of development who have not acquired the skills expected for their chronological age. It may be caused by neurological diseases, chronic but non-neurological disorders, or other conditions responsible for absent or abnormal environmental stimulation.3 Normal development in children aged up to 2 years is well documented. This is a crucial stage for understanding the different areas of psychomotor development, the variants of normality, and warning signs classified by age.4 There are many disorders associated with psychomotor retardation, including autism spectrum disorders, attention deficit hyperactivity disorder, cognitive delay, learning disabilities, sensory alterations, cerebral palsy (CP), developmental delay, and other rare syndromes such as isodicentric 15 syndrome (IDIC-15) and Dandy-Walker syndrome. Some researchers have highlighted the difficulty of identifying the factors involved in psychomotor development because so many components are involved (behavioural, motor, cognitive, and affective).2,4
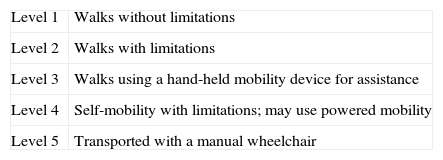
Currently, the use of equine-assisted therapy is regulated and becoming increasingly common around the world. Several studies support the hypothesis that horses and horseback riding have been used throughout history to improve quality of life or people's general state of health.5,6 Whalen and Case-Smith conducted a systematic review of studies evaluating hippotherapy and therapeutic horseback riding in children with CP. Despite the low level of evidence of the studies, these authors concluded that equine-assisted therapy improved gross motor function in children with GMFCS levels I to III (Table 1).7 Other studies not included in the review article mentioned above also report a positive impact of equine-assisted therapy on postural control and quality of movement.8–13 Ionatamishvili et al.9 observed that therapeutic horseback riding improved motor skills and reduced spasticity in children with CP. In fact, this type of therapy achieved greater improvements than Bobath therapy (a dynamic, practical, multidisciplinary approach to neurological rehabilitation in people with impaired motor control). Tauffkirchen10 supports supplementing standard treatment with equine-assisted therapy for several reasons. Firstly, adapting to the horse's swaying movements, preserving straightening alignment, and maintaining symmetry and balance are intrinsic to hippotherapy and reinforce patients’ usual treatments. Secondly, hippotherapy motivates patients to fully engage in rehabilitation. And lastly, as Davis et al.13 observed in their study, a walking horse transmits three-dimensional, rhythmic impulses to the rider which are similar to the movements experienced in natural human gait. Functional improvements in children with CP were essentially due to this movement.
The results reported by studies of equine-assisted therapy for children with neurological diseases cannot be extrapolated due to their small sample sizes and heterogeneity in terms of patients’ ages and clinical manifestations. Nevertheless, we should highlight that it is extremely difficult to establish a homogeneous sample in the clinical setting, especially among children, due to the wide range of disorders they may present. Researchers should therefore find some common denominator between children with different conditions so as not to disregard those with less common illnesses.12
The purpose of our study is to analyse any changes in gross motor function and quality of life produced by equine-assisted therapy in children with psychomotor retardation. Our hypothesis was that equine-assisted therapy, when used as complementary therapy, does have a beneficial impact on gross motor function and quality of life in these children.
Material and methodsParticipantsSubjects were recruited from among members of an equestrian therapy group (Fundación Caballo Amigo) who presented some type of psychomotor development disorder. We considered all patients displaying a chronological delay of at least one year in at least 2 of the following areas on the Picq and Vayer test: hand-eye coordination, general dynamic coordination, and postural control (balance). For children younger than 4 years, only those showing a chronological delay of at least 6 months were included. The Picq and Vayer examination is a psychomotor test mainly consisting of the first 3 sections of the Ozeretski test, which were revised and adapted by Guilmain: hand-eye coordination, general dynamic coordination, and postural control.1 Each of these sections include tasks of increasing complexity, arranged by age group, that a child with normal psychomotor development is expected to perform without difficulty.
The inclusion criteria were as follows: being younger than 18; being able to walk with or without support devices, stand without support devices, and understand simple instructions; and not having started treatment intended to increase muscle tone in at least the previous 3 months. Both children and their carers had to authorise the patients’ inclusion in the study. Exclusion criteria were presence of cognitive deficits severe enough to prevent children from understanding simple instructions, and motor impairment causing inability to walk with support devices or inability to stand without support devices. Patients with comorbidities that contraindicate equine-assisted therapy were also excluded.
We initially recruited 39 children, 11 of whom were finally included in the study. Participants were aged 3 to 15 years (8.82±3.89 years; 6 boys and 5 girls).
Five patients had CP (one also had Down syndrome), 4 presented developmental delay, one had Dandy-Walker syndrome, and the last had IDIC-15 syndrome.
Study designThe present study was approved by the Ethics Committee of Fundación Caballo Amigo and complies with the principles established by the Declaration of Helsinki. We conducted a longitudinal prospective study with no control group. The main study variables were gross motor function and perceived quality of life. The variables sex, age, and other treatments received were all controlled. We used the Gross Motor Function Measure (GMFM-88) to assess the following areas: lying, sitting, crawling, kneeling, standing, and walking. Health related to quality of life was evaluated using questions about physical, emotional, social, or academic functioning using the Pediatric Quality of Life Inventory (PedsQL).14
Children were evaluated on 3 occasions: before and after a period of inactivity, coinciding with Christmas holidays, and 2 months after the second assessment (after a 2-month period of uninterrupted treatment).
Experimental protocolInterventions were conducted at the facilities owned by Fundación Caballo Amigo, in Villanueva del Pardillo, Madrid. All professionals working at this centre are specifically trained in treating patients with disorders since they are certified experts in therapeutic horseback riding. These therapists follow a pre-established plan for achieving rehabilitation or learning objectives.
The methodology applied by the group is based on the Global Rehabilitation Method with Horses (GRMH).15 GRMH is a type of movement therapy that enables construction or reconstruction of sensorimotor schemes by combining and repeating specific stimuli in the order of the stages in motor function development. For patients with CNS lesions, the movement of the horse is the biodynamic basis of this therapeutic intervention. Correct functioning of the proprioceptive and tactile afferent pathways adequately integrates the patient's body scheme, regulates muscle tone, achieves correct posture and postural control automatisms, and enables temporal, spatial, and sequential structuring. GRMH is fundamentally based on the ideal horseback riding posture: an upright sitting position with a neutral pelvis. The patient's centre of gravity and 3 body planes (sagittal, horizontal, and frontal) must be aligned with those of the horse. The difficulty to maintain balance on the horse depends on the position of the pelvis. Riding equipment is also very important. The saddle must allow pelvic retroversion to facilitate a reflex-inhibiting position (Bobath): slightly flexed hip and knees, hip abduction, and hip external rotation.16
A horse walks with a 4-beat gait. As a result, it transmits sinusoidal and rhythmic stimuli to the rider which affect the 3 planes. The rider will perceive opposite modulated movements forward and backward, upward and downward, as well as lateral swaying. These forces, with their opposite rhythms and movements, create a balance that envelops and engages the patient's body; at the same time, the CNS collects afferent data. In patients who are unable to walk independently, the stimuli involved in riding a walking horse resemble those occurring in normal human gait16 and prepare the nervous system for walking.
We conducted 2 different types of equine-assisted therapeutic activities:
- -
Hippotherapy: the patient sits on the horse's back on top of a saddle or saddle blanket that may feature specific adaptations. The horse proceeds necessarily at a walk. The patient does not actively participate in this intervention, which is led by the therapist. The main focus of this type of intervention is rehabilitation.
- -
Therapeutic horseback riding: horseback riding adapted for people with motor, psychological, or sensory disabilities. A saddle with stirrups is used in most cases, although it may be modified to suit the patient's needs. Patients are required to actively participate in guiding the horse and controlling its speed. Therapeutic horseback riding is aimed at more independent patients, and it focuses on therapeutic learning.
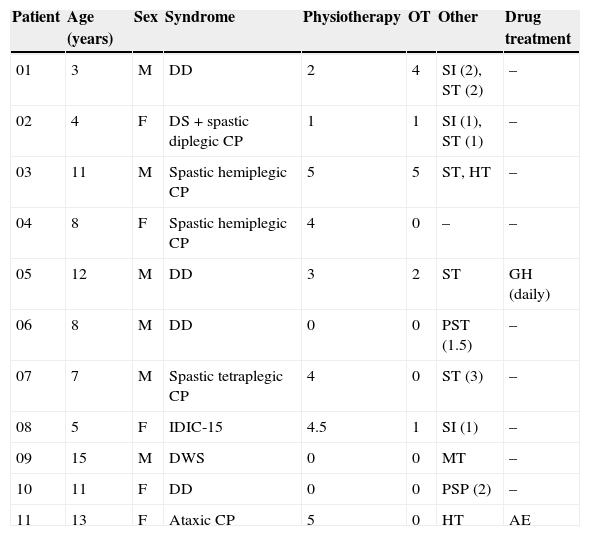
In our study, 5 patients received hippotherapy, 5 therapeutic horseback riding, and one was treated with a combination of both types of therapy. Each participant completed a 45-minute session once a week throughout a full academic year. The intervention period examined by our study was 4 months. During the study period, all participants continued with their usual rehabilitation sessions and pharmacological treatment. Patients’ characteristics are listed in Table 2.
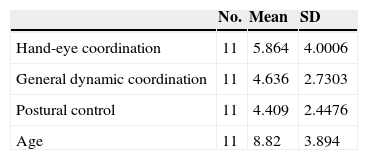
Participants’ characteristics.
| Patient | Age (years) | Sex | Syndrome | Physiotherapy | OT | Other | Drug treatment |
|---|---|---|---|---|---|---|---|
| 01 | 3 | M | DD | 2 | 4 | SI (2), ST (2) | – |
| 02 | 4 | F | DS+spastic diplegic CP | 1 | 1 | SI (1), ST (1) | – |
| 03 | 11 | M | Spastic hemiplegic CP | 5 | 5 | ST, HT | – |
| 04 | 8 | F | Spastic hemiplegic CP | 4 | 0 | – | – |
| 05 | 12 | M | DD | 3 | 2 | ST | GH (daily) |
| 06 | 8 | M | DD | 0 | 0 | PST (1.5) | – |
| 07 | 7 | M | Spastic tetraplegic CP | 4 | 0 | ST (3) | – |
| 08 | 5 | F | IDIC-15 | 4.5 | 1 | SI (1) | – |
| 09 | 15 | M | DWS | 0 | 0 | MT | – |
| 10 | 11 | F | DD | 0 | 0 | PSP (2) | – |
| 11 | 13 | F | Ataxic CP | 5 | 0 | HT | AE |
Treatments are expressed in hours per week.
AE: antiepileptics; F: female; GH: growth hormone; HT: hydrotherapy; IDIC-15: isodicentric 15 syndrome; SI: sensory integration; ST: speech therapy; M: male; MT: music therapy; CP: cerebral palsy; PST: psychomotor therapy; PSP: psychopedagogy; DD: developmental delay; DS: Down syndrome; DWS: Dandy-Walker syndrome; OT: occupational therapy.
To contrast variables we used a non-parametric test for 2 paired samples (Wilcoxon rank sum test for quantitative data). Data were analysed using SPSS statistical software, version 19. All values are expressed as means±SD. P values <.05 were considered statistically significant.
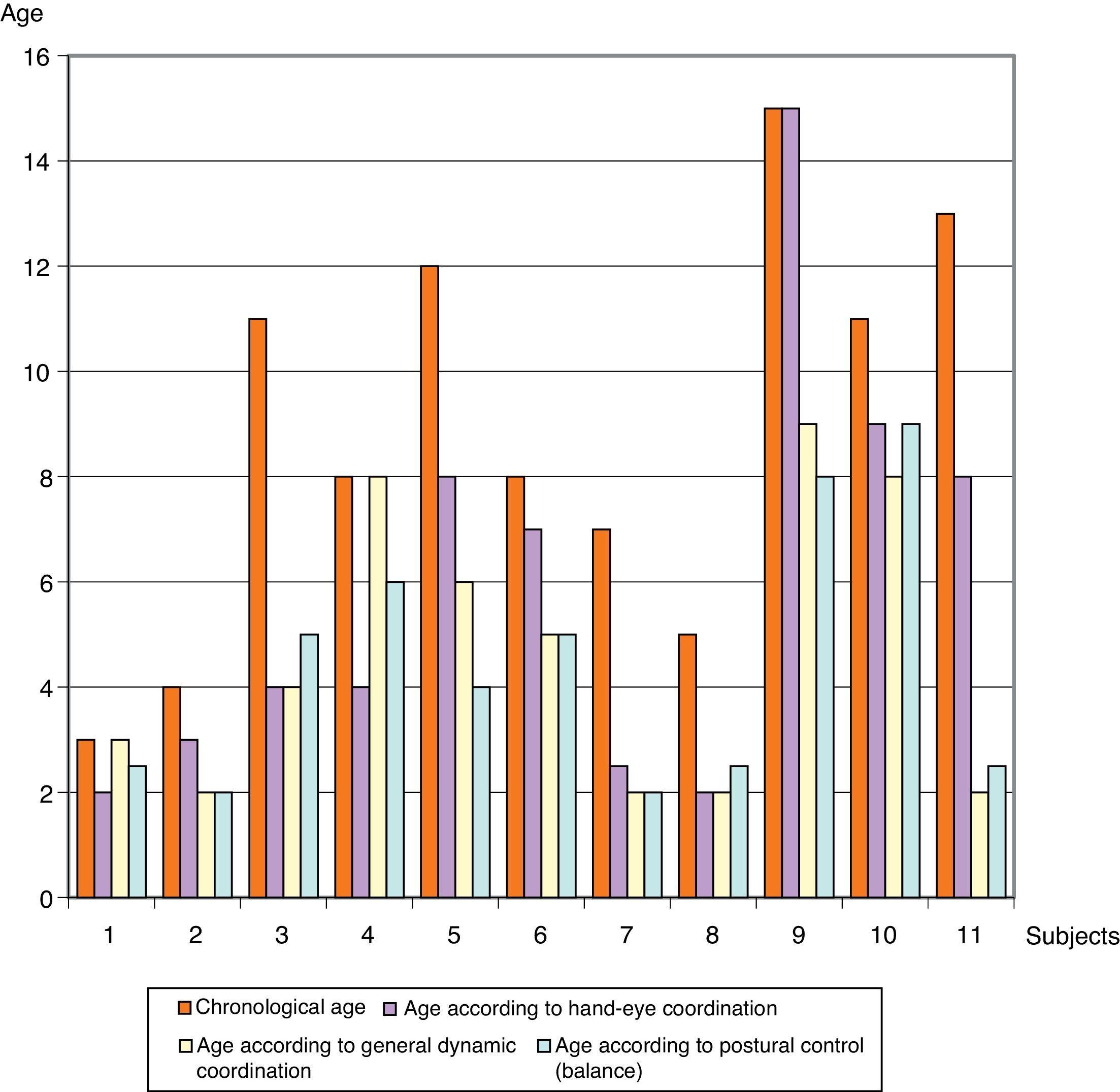
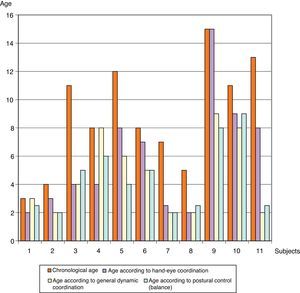
ResultsFig. 1 shows differences between the participants’ ages according to psychomotor development and their chronological ages. Patients are numbered from 1 to 11. Patient 1, aged 3, shows the least amount of difference between the age for his level of psychomotor development and his chronological age; the greatest difference is seen in patient 3, who is 6 years older than the age that corresponds to his degree of postural control. Breaking down the results by area, the highest mean corresponds to hand-eye coordination (5.86±4 years), and the most homogeneous area for the whole sample was postural control and balance (4.4±2.44 years). The mean chronological age of the group was 8.82±3.89 (Table 3).
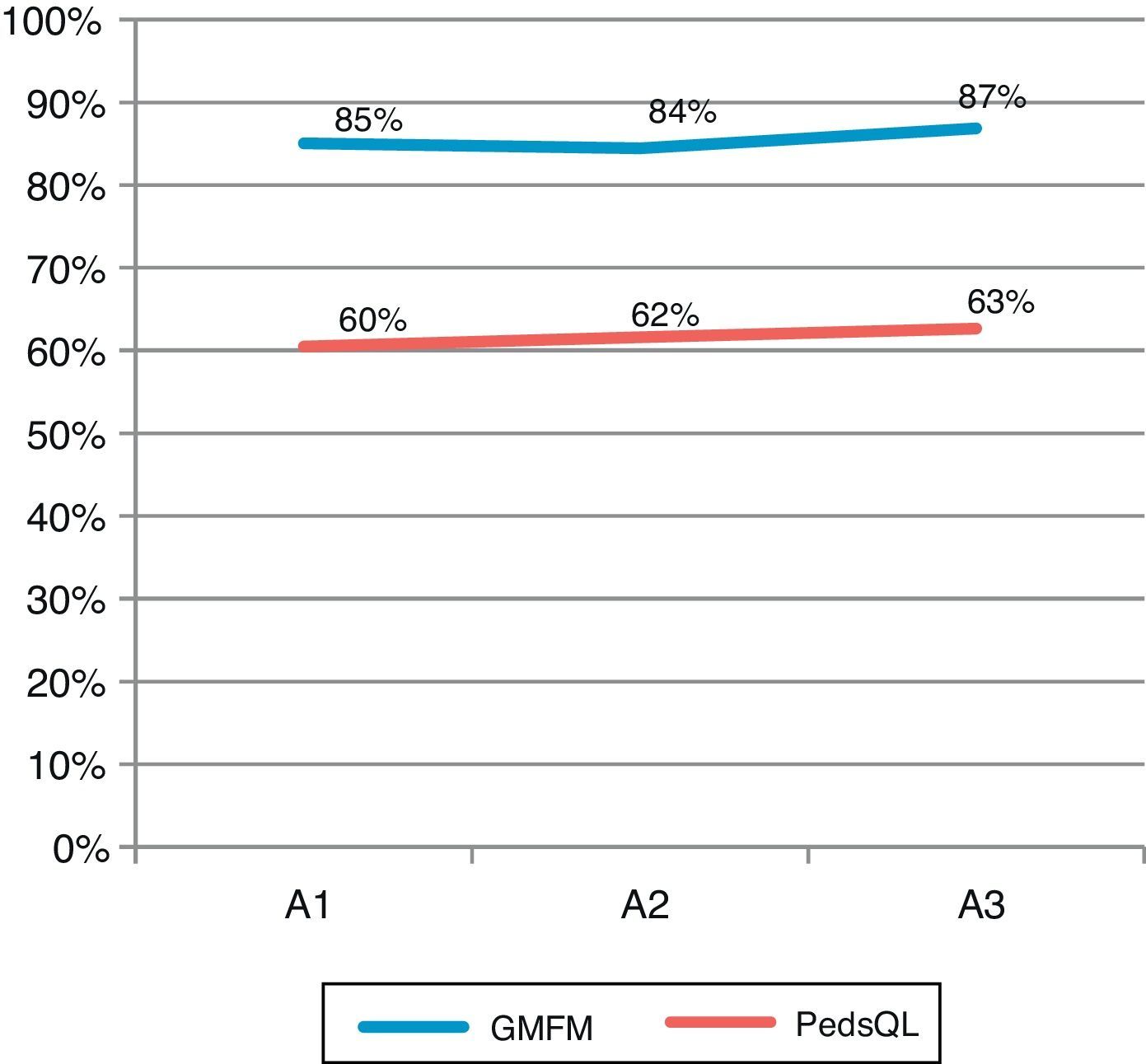
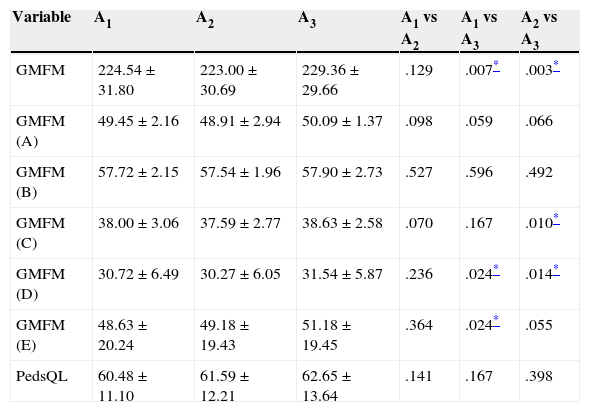
After confirming psychomotor delay in all subjects, we analysed the data obtained in the initial (A1), second (A2), and final (A3) assessments. We found significant differences in global GMFM-88 scores between the initial and final assessments (A1 vs A3) and between the second and final assessments (A2 vs A3). Scores measured after continued treatment (A2 vs A3) show an increase of 2.41% and a P value=.003. The most prominent results were found in the areas ‘crawling and kneeling’ (P=.010) and ‘standing’ (P=.014) (Table 4).
Mean±SD scores on the GMFM-88 (A–E) and PedsQL scales and P values for changes in scores over time.
| Variable | A1 | A2 | A3 | A1 vs A2 | A1 vs A3 | A2 vs A3 |
|---|---|---|---|---|---|---|
| GMFM | 224.54±31.80 | 223.00±30.69 | 229.36±29.66 | .129 | .007* | .003* |
| GMFM (A) | 49.45±2.16 | 48.91±2.94 | 50.09±1.37 | .098 | .059 | .066 |
| GMFM (B) | 57.72±2.15 | 57.54±1.96 | 57.90±2.73 | .527 | .596 | .492 |
| GMFM (C) | 38.00±3.06 | 37.59±2.77 | 38.63±2.58 | .070 | .167 | .010* |
| GMFM (D) | 30.72±6.49 | 30.27±6.05 | 31.54±5.87 | .236 | .024* | .014* |
| GMFM (E) | 48.63±20.24 | 49.18±19.43 | 51.18±19.45 | .364 | .024* | .055 |
| PedsQL | 60.48±11.10 | 61.59±12.21 | 62.65±13.64 | .141 | .167 | .398 |
A: lying; B: sitting; C: crawling; D: standing; E: walking. GMFM: Gross Motor Function Measure; PedsQL: Pediatric of Quality of Life Inventory; A1: initial assessment; A2: second assessment; A3: final assessment.
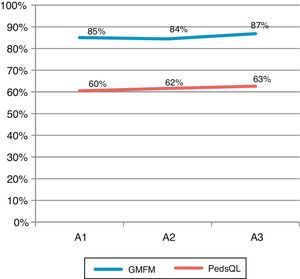
There were no statistically significant changes in the PedsQL scores. Scores (given as percentages) increased with each assessment. However, we cannot state that equine-assisted therapy is directly responsible for this increase, since the P value associated with the Wilcoxon test is higher than .05 in the 3 assessments. Three participants achieved lower PedsQL scores in the final assessment than in the initial one, while others showed a marked positive deviation from the mean; this may be the reason why the standard deviation increased progressively with each assessment.
Fig. 2 shows global changes in the GMFM-88 and PedsQL scores for the full group. The line representing GMFM-88 scores displays a slight decrease at A2 and therefore exhibits a concave curvature, whereas PedsQL scores increase progressively although discretely.
DiscussionThe purpose of our study is to analyse the changes in gross motor function and quality of life in children with psychomotor retardation who undertake equine-assisted therapy in addition to their normal rehabilitation treatments. Equine-assisted therapy, when used as an adjuvant to other types of therapy, is considered to have a positive impact on gross motor function and quality of life. Our results partially support the initial hypothesis.
We obtained a sample of children whose common denominator was psychomotor delay rather than a specific disease. Scales and tools that adequately classify psychomotor retardation were used to gather as homogeneous a sample as possible. For all participants, levels of psychomotor development in the 3 areas assessed were at least 2 years below their actual chronological ages. Psychomotor delay was secondary to neurological diseases or non-neurological chronic diseases such as genetic alterations. Our sample, although homogeneous in terms of presence of psychomotor delay, included children with different disorders and a wide range of clinical manifestations.
GMFM-88 scores displayed statistically significant changes. We observed no change or improvement in scores between the initial and second assessments. This period also included a 3-week period of inactivity corresponding to the Christmas holidays. However, we did find a statistically significant improvement in scores after periods of uninterrupted therapy (A1 vs A3, A2 vs A3). This fact supports the hypothesis that equine-assisted therapy can have a positive impact on psychomotor development.
Results show improved gross motor function, especially in the areas ‘crawling and kneeling’ and ‘standing’. Improvements are more pronounced after the uninterrupted period of treatment (from A2 to A3). Therefore, the statistically significant difference in the measurement for gross motor functions supports the initial hypothesis.
Self-perceived quality of life increased for most of the participants, but increases were not so pronounced as to be statistically significant.
Most of the studies and review articles we consulted analyse the effect of equine-assisted therapy on children with CP17 and various degrees of impairment18 and report positive results for total gross motor function scores and dimension-specific scores. Casady and Nichols-Larsen19 report improvements not only for gross motor function but also for functional outcomes. Haehl et al.20 observed an increase in postural control when they performed a kinematic analysis of seated riders’ trunks to record articulation angles. Likewise, Winchester et al.21 described significant increases in gross motor function, although not in gait speed.
Regarding personal well-being and quality of life, several reviews and studies22 support our findings and demonstrate that equine-assisted therapy is a non-invasive treatment option with an emotional component linked to the presence and control of the horse. Patients’ self-perception may improve in parallel to their motor function,23 as seen in our study, which may in turn facilitate these children's integration in society. In a study analysing the connection between hippotherapy and mental well-being in patients with spinal cord injury, Lechner et al.24 concluded that motor improvements produced by this type of intervention were more marked than emotional improvements. However, these beneficial effects were only seen in the short term. On the other hand, a study by Davis et al.13 did not find therapeutic horseback riding to have a clinically significant impact on the quality of life of children with CP. However, these results may be due to low sensitivity of the assessment tools, and this may also be the case in the present study. In other studies, quality of life was assessed according to researchers’ subjective observations and without using standardised tools; its connection with equine-assisted therapy is therefore difficult to evaluate.25–27
Study limitationsOur study presents several limitations that should be corrected in future studies. On the one hand, the wide variety of participants’ disorders may have had an impact on other study variables. It may be argued that the selected criterion for homogeneity (level of psychomotor development) may yield robust results since these levels do not reflect changes present in specific disorders. However, our findings are drawn from a small sample of 11 children (with CP, Down syndrome, developmental delay, Dandy-Walker syndrome, and IDIC-15 syndrome) and as such they cannot be extrapolated to the many possible aetiologies of psychomotor retardation. Multi-centre studies including larger series will be necessary to generalise, confirm, or refute our findings. Furthermore, our results should be interpreted with caution due to the wide age range among the included patients. Age is a parameter that should be controlled in further studies that feature larger samples.
All of the patients continued with their original treatment sessions while also receiving equine-assisted therapy at Fundación Caballo Amigo. They were therefore treated with several types of therapies in addition to equine-assisted therapy during the study period. Although this combination of different therapies seems to yield improvements in the study variables, a direct connection cannot be established between these improvements and equine-assisted therapy as a complementary treatment, since results may be due to greater treatment intensity. Therefore, new lines of research should aim to dissociate equine-assisted therapy from other types of therapy and the variable of treatment intensity. Likewise, follow-up after the intervention should be intensified so as to analyse medium- and long-term effects of this type of therapy.
Clinical relevance and future researchOur findings are clinically relevant on many levels and pave the way for further lines of research. The present study provides a better understanding of equine-assisted therapy in children with psychomotor retardation. We aimed to demonstrate our clinical experience with this therapy while following the scientific method. We recognise the deviations from the scientific method that are inherent to clinical studies. Furthermore, our criterion for homogeneous sample selection may be the starting point for groundbreaking future studies including children with a wide range of disorders. This approach would therefore deepen but also refine our knowledge of the benefits of equine-assisted therapy, and benefit patients with rare and lesser-known conditions.
Despite the limitations listed above, we feel that our study provides useful information for patients, families, and researchers, and opens new horizons in a highly heterogeneous and complex yet promising field.
ConclusionsWhile the study has its limitations, the interventions have been shown to improve gross motor function in children with psychomotor delay. We observed marked changes in motor control throughout the study period, which suggests that equine-assisted therapy is a suitable treatment option for psychomotor development disorders. Regarding quality of life, however, improvements were modest and not statistically significant. Studies with a higher methodological quality will be needed in order to support the use of equine-assisted therapy with a stronger level of clinical evidence.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: del Rosario-Montejo O, Molina-Rueda F, Muñoz-Lasa S, Alguacil-Diego IM. Efectividad de la terapia ecuestre en niños con retraso psicomotor. Neurología. 2015;30:425–432.