Epilepsy is a group of long-term neurological disorders characterised by seizures that may respond to pharmacological treatment.
ObjectiveDetermine the prescribing patterns of anticonvulsants for patients covered by the healthcare system in Colombia.
MethodsCross-sectional study using a database containing 6.5 million people. From among residents in 88 Colombian cities, we selected patients of both sexes and all ages who were treated continuously with anticonvulsants between June and August 2012. We designed a drug consumption database and performed multivariate analysis for combination treatment and co-medication using SPSS 20.0.
ResultsA total of 13793 patients with mean age of 48.9±22.0 years were studied; 52.9% of the participants were women. Of the patient total, 74.4% were treated in monotherapy and 25.6% received two or more anticonvulsants. Globally, 72.9% of the patients were initially treated with classic anticonvulsants and 27.1% with new drugs. The most frequently used drugs were valproic acid (33.3%), carbamazepine (30.2%), clonazepam (15.7%), pregabalin (10.3%), phenytoin (10.0%) and levetiracetam (7.9%). Most agents were used in higher doses than recommended. The most common combinations were valproic acid+clonazepam (10.9%), valproic acid+carbamazepine (10.0%), carbamazepine+clonazepam (5.6%), valproic acid+phenytoin (4.4%). The most frequently prescribed co-medications were antihypertensives (61.0%), lipid-lowering drugs (45.8%), antidepressants (36.7%), antipsychotics (20.1%), anxiolytics (7.9%), and lithium (1.8%).
DiscussionDoctors predominantly prescribe drugs with a high therapeutic value and favour anticonvulsant monotherapy. Most agents were used in higher doses than recommended. This underlines the need to design educational strategies addressing these prescribing habits, and to undertake research on the effectiveness of treatment.
La epilepsia constituye un problema neurológico común caracterizado por convulsiones.
ObjetivoSe pretendió determinar los patrones de prescripción de medicamentos antiepilépticos en pacientes afiliados al Sistema de Salud de Colombia.
MétodosEstudio de corte transversal sobre una base de datos de 6,5 millones de personas. Se seleccionó a pacientes de cualquier sexo y edad, residentes en 88 ciudades, tratados con antiepilépticos desde junio a agosto del 2012. Se diseñó una base de datos de consumo de medicamentos, se hicieron análisis multivariados sobre utilización en terapia combinada y comedicación mediante SPSS 20.0.
ResultadosSe estudió a 13.793 pacientes, con edad promedio de 48,9±22,0 años; el 52,9% eran mujeres; el 74,4% recibía monoterapia antiepiléptica y el 25,6%, 2 o más anticonvulsivos. El orden de prescripción fue: clásicos (72,9%) y nuevos antiepilépticos (27,1%). Los más frecuentemente empleados fueron: ácido valproico (33,3%), carbamazepina (30,2%), clonazepam (15,7%), pregabalina (10,3%), fenitoína (10,0%) y levetiracetam (7,9%). La mayoría, a dosis superiores a las recomendadas. Las combinaciones más comunes fueron: ácido valproico+clonazepam (10,9%), ácido valproico+carbamazepina (10,0%), carbamazepina+clonazepam (5,6%) y ácido valproico+fenitoína (4,4%). Las comedicaciones más frecuentes fueron: antihipertensivos (61,0%), hipolipidemiantes (45,8%), antidepresivos (36,7%), antipsicóticos (20,1%), ansiolíticos (7,9%) y litio (1,8%).
DiscusiónPredominan los hábitos de prescripción de medicamentos de alto valor terapéutico, principalmente en la monoterapia antiepiléptica. La mayoría se emplea en dosis mayores a las recomendadas. Se plantea la necesidad de diseñar estrategias educativas para corregir algunos hábitos de prescripción e investigaciones que evalúen la efectividad del tratamiento.
Epilepsy is one of the most frequent neurological diseases overall, affecting approximately 1% to 3% of the population. Nearly 10% of the population will experience at least one seizure episode at some point in their lives.1 Around 50 million people in the world have epilepsy.2,3 The incidence of this disorder in developing countries is much higher due to poor sanitation, deficient healthcare systems, and an increased risk of cerebral infections.2–5
The risk of mortality is 2 to 3 times higher in epileptic patients than in the general population.6,7 In these patients, deaths are not directly associated with seizures but rather with a variety of comorbidities including tumours, cerebrovascular diseases, ischaemic heart diseases, pneumonia, suicide, and accidents.6–17
One of the challenges faced by the Colombian health and social security system (SGSSS) and other health organisations is to improve epilepsy detection, access to treatment, and follow-up for epileptic patients. Colombia's National Institute for Drug and Food Surveillance was created in 1995 with a view to promoting responsible drug use. This entity established the Compulsory Health Plan, a list of essential medications including 8 antiepileptic agents that clinicians working for the SGSSS can prescribe: carbamazepine, phenytoin, phenobarbital, lamotrigine, valproic acid, ethosuximide, primidone, and clonazepam.18 To prescribe other antiepileptic agents, doctors must send a special request to the health service institutions (the ‘technical-scientific committees’, or TSC) via a standard procedure explaining the need for prescribing a drug other than those listed by the Compulsory Health Plan.18 Likewise, patients also have a legal means or procedure (tutela, or guardianship) to request access to drugs not included in the list.
The purpose of this study is to analyse antiepileptic prescription patterns in Colombia with a view to providing a deeper knowledge of antiepileptic drug use in our country. These data can help in developing programmes to achieve more appropriate use of these drugs and better patient management.
Materials and methodsWe conducted a cross-sectional study to analyse antiepileptic prescription patterns in a population of about 6.5 million people registered with the SGSSS and using its health insurance providers. The population amounts to around 31% of all actively employed individuals covered by the Colombian healthcare system and 13.1% of the total population of Colombia. Between 1 June and 30 August 2012, we recorded prescriptions issued to all patients treated with antiepileptic drugs in Colombian towns and cities with reliable databases (municipalities with between 30000 and 7.5 million inhabitants).
We included data from all patients who had attended a healthcare centre and were treated with antiepileptic drugs for at least 3 months, regardless of sex and age. This inclusion criterion is intended to guarantee that all patients from the sample were treated continuously, which would reflect drug tolerability and treatment adherence. We excluded the patients who missed medical appointments at the end of the observation period, as these patients introduce a bias into a study aimed at describing long-term continuous drug treatment.
Based on drug consumption data, which are systematically gathered by a pharmaceutical distributor (Audifarma, S.A.), we created a database that would be used to record the following variables:
- 1.
Sociodemographic variables: sex, age (children: 0–17; young adults: 18–34; adults: 35–64; elderly: 65–99), town or city of residence.
- 2.
Antiepileptic drugs dispensed in Colombia and the corresponding dose (doses were calculated using the defined daily dose or DDD). We recorded antiepileptic drugs available in Colombia, noting whether they were prescribed in monotherapy or as combination therapy.
Polymedication was regarded as an alternative indicator of chronic disease, which is a risk factor in patients with epilepsy. We considered the following drugs/conditions: (a) antidiabetic treatment/diabetes mellitus, (b) antiparkinsonian drugs/Parkinson's disease, (c) antiretrovirals/human immunodeficiency virus infection-AIDS, (d) antidepressants/depression, (e) anxiolytics and hypnotics/anxiety or sleep disorders, (f) lipid-lowering drugs/dyslipidaemia, (g) methylphenidate/attention-deficit hyperactivity disorder, (h) nitrovasodilators/ischaemic heart disease, (i) antihypertensives/arterial hypertension, (j) mood stabilisers/bipolar affective disorder, (k) antipsychotics/psychoses-schizophrenia, and (l) anti-dementia drugs/dementia-Alzheimer disease. In these cases, we analysed the viability of using each antiepileptic drug based on the effects that these agents may have on comorbidities.9–17
Following the principles of the Declaration of Helsinki, our study protocol was classified as ‘research without risk’. Data were analysed using SPSS statistical software, version 20.0 for Windows (IBM, USA). We used the t-test or ANOVA method for quantitative variables and the chi-square test for categorical variables. A logistic regression model was applied using antiepileptic monotherapy/combined therapy and comedication (yes/no) as the dependent variables; the covariates were those variables showing a significant association with the dependent variables in bivariate analyses. Statistical significance was set at P<.05.
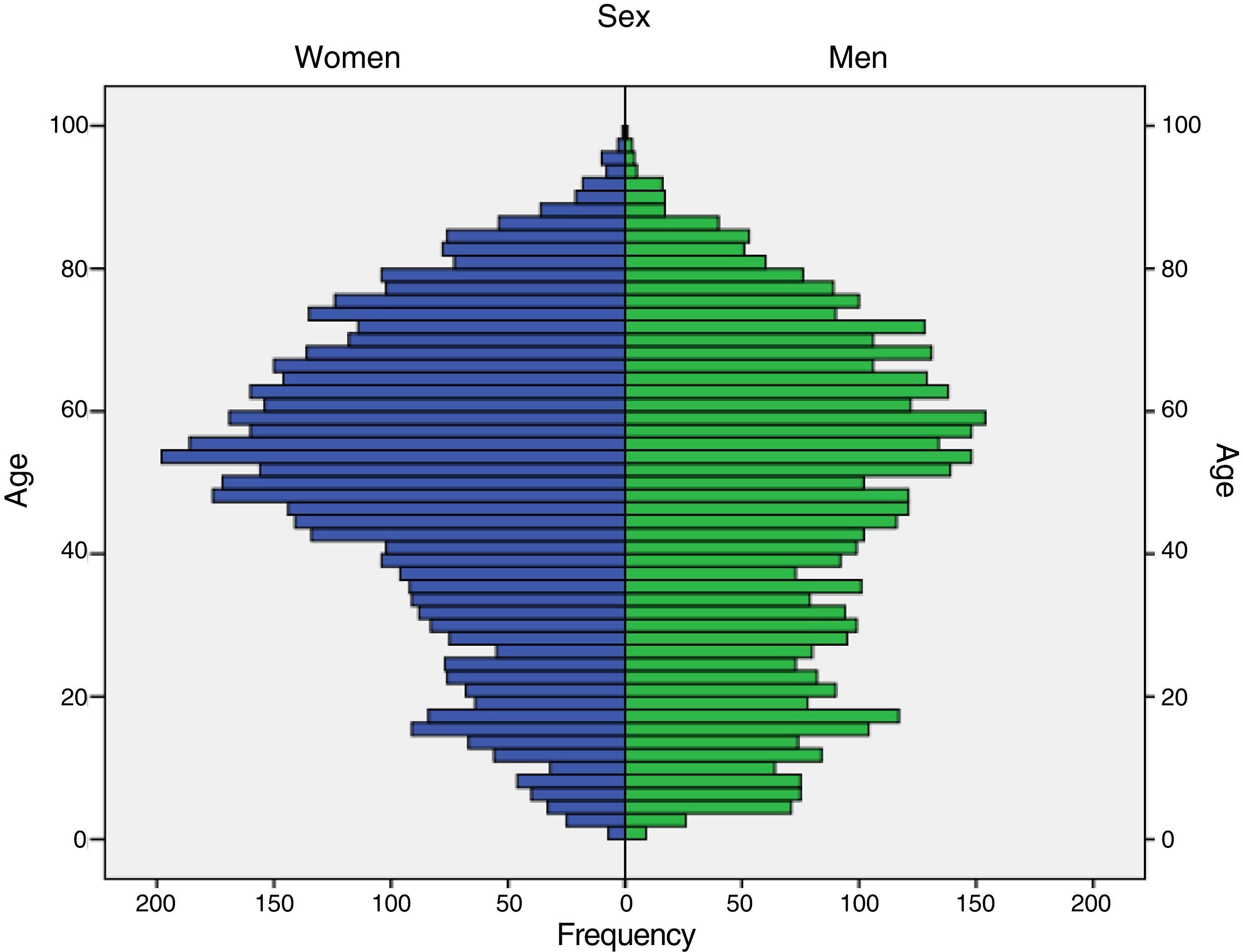
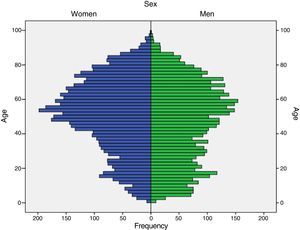
ResultsOf the 13793 patients affiliated with the SGSSS and receiving antiepileptics for at least 3 months, 7301 (52.9%) were women and 6491 (47.1%) were men; mean age was 48.9±22.0 years (range, 1–99 years) (Fig. 1). Differences between men and women were statistically significant in the following age groups: 0 to 17 years (59.2% vs 40.8%, P<.001), 18 to 34 years (52.9% vs 47.1%, P<.001), 35 to 64 years (44.6% vs 55.4%, P<.001), and older than 65 (44.6% vs 55.4%, P=.007).
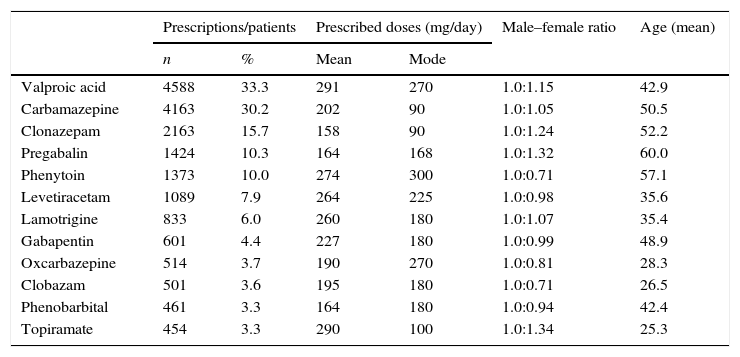
Table 1 shows prescription patterns for the most frequently used antiepileptics in Colombia. Broken down by pharmacological group, 72.9% of the patients received classic antiepileptics and 27.1% were treated with new antiepileptics. Carbamazepine and clonazepam were prescribed at typical doses whereas doses of valproic acid, phenytoin, levetiracetam, phenobarbital, and pregabalin were higher than the DDD. None of the patients received ethosuximide, felbamate, or tiagabine.
Prescription patterns for antiepileptics included in the list of essential medicines in Colombia (2012).
| Prescriptions/patients | Prescribed doses (mg/day) | Male–female ratio | Age (mean) | |||
|---|---|---|---|---|---|---|
| n | % | Mean | Mode | |||
| Valproic acid | 4588 | 33.3 | 291 | 270 | 1.0:1.15 | 42.9 |
| Carbamazepine | 4163 | 30.2 | 202 | 90 | 1.0:1.05 | 50.5 |
| Clonazepam | 2163 | 15.7 | 158 | 90 | 1.0:1.24 | 52.2 |
| Pregabalin | 1424 | 10.3 | 164 | 168 | 1.0:1.32 | 60.0 |
| Phenytoin | 1373 | 10.0 | 274 | 300 | 1.0:0.71 | 57.1 |
| Levetiracetam | 1089 | 7.9 | 264 | 225 | 1.0:0.98 | 35.6 |
| Lamotrigine | 833 | 6.0 | 260 | 180 | 1.0:1.07 | 35.4 |
| Gabapentin | 601 | 4.4 | 227 | 180 | 1.0:0.99 | 48.9 |
| Oxcarbazepine | 514 | 3.7 | 190 | 270 | 1.0:0.81 | 28.3 |
| Clobazam | 501 | 3.6 | 195 | 180 | 1.0:0.71 | 26.5 |
| Phenobarbital | 461 | 3.3 | 164 | 180 | 1.0:0.94 | 42.4 |
| Topiramate | 454 | 3.3 | 290 | 100 | 1.0:1.34 | 25.3 |
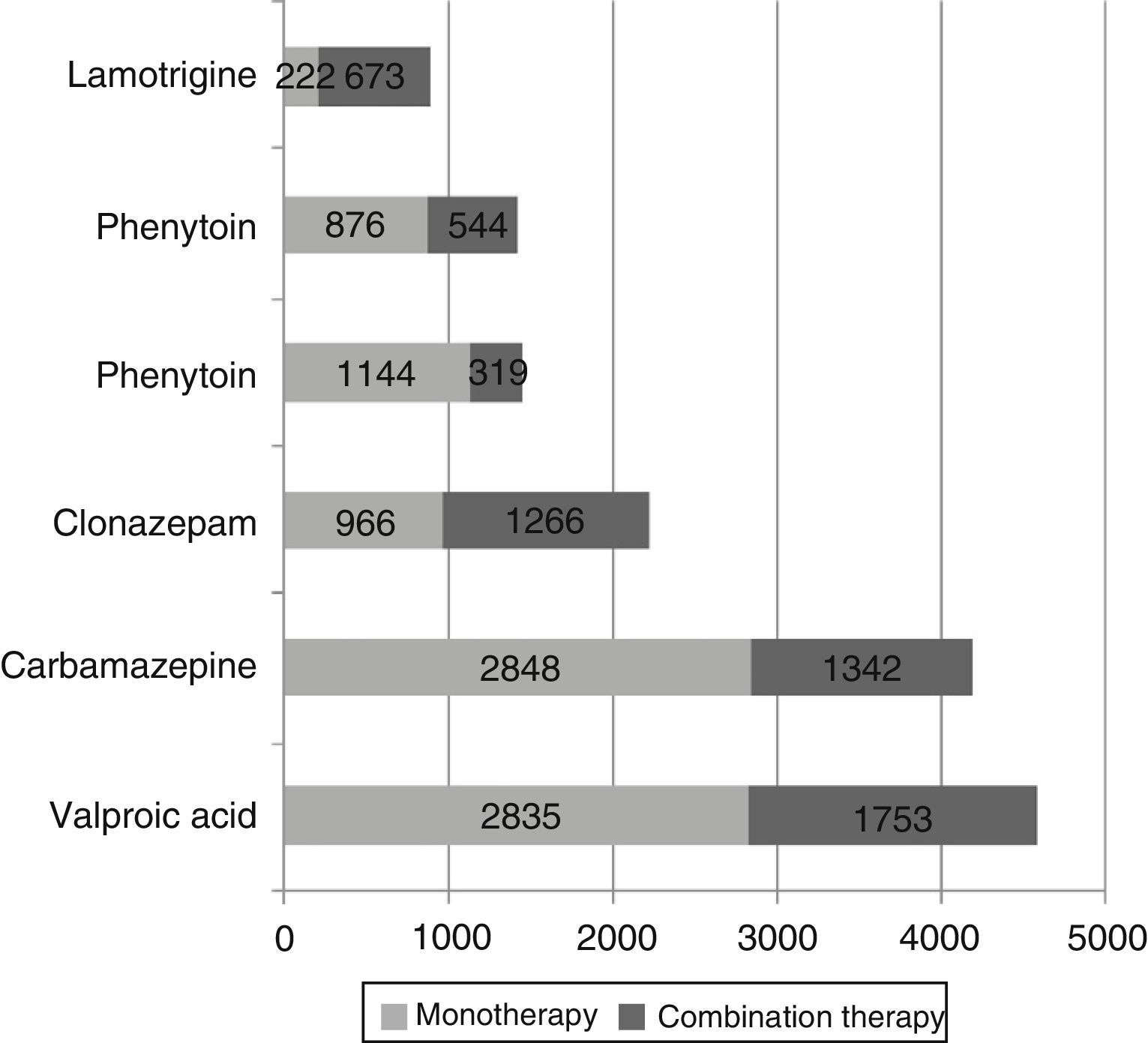
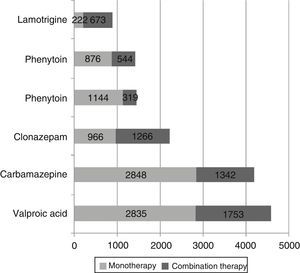
Of the patient total, 10257 (74.4%) received only one antiepileptic drug whereas 3536 patients (25.6%) were treated with at least 2 antiepileptics: 695 patients (5.0%) received 3, 124 (0.9%) received 4, and 23 (0.16%) received 5 or more antiepileptic drugs. Fig. 2 shows the number of patients receiving each drug either in monotherapy or as combination therapy: as a general rule, these antiepileptics were more frequently used in monotherapy. The most frequently prescribed combinations of antiepileptics were valproic acid+clonazepam (n=387; 10.9%), valproic acid+carbamazepine (n=352; 10.0%), carbamazepine+clonazepam (n=199; 5.6%), and valproic acid+phenytoin (n=156; 4.4%). The most frequent combinations of 3 antiepileptics were valproic acid+carbamazepine+clonazepam (n=81; 11.7%), valproic acid+carbamazepine+levetiracetam (n=41; 5.9%), and valproic acid+clonazepam+lamotrigine (n=39; 5.6%). We found statistically significant differences in the percentage of patients receiving monotherapy between men and women (71.4% vs 77.0%, P<.001).
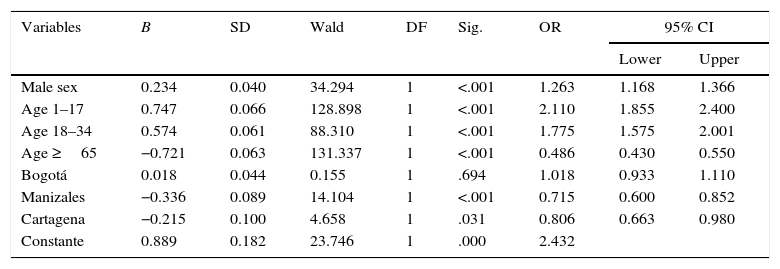
Using a binary logistic regression model, we analysed the relationship between use of combination therapy and other variables. Male sex and ages between 1 and 17 years, and between 18 and 34 years, were the variables associated with a higher probability of receiving combination therapy; in contrast, being treated in Manizales or Cartagena was associated with a significantly lower probability (Table 2).
Variables associated with combined antiepileptic treatment in a binary logistic regression model (Colombia, 2012).
| Variables | B | SD | Wald | DF | Sig. | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Male sex | 0.234 | 0.040 | 34.294 | 1 | <.001 | 1.263 | 1.168 | 1.366 |
| Age 1–17 | 0.747 | 0.066 | 128.898 | 1 | <.001 | 2.110 | 1.855 | 2.400 |
| Age 18–34 | 0.574 | 0.061 | 88.310 | 1 | <.001 | 1.775 | 1.575 | 2.001 |
| Age ≥65 | −0.721 | 0.063 | 131.337 | 1 | <.001 | 0.486 | 0.430 | 0.550 |
| Bogotá | 0.018 | 0.044 | 0.155 | 1 | .694 | 1.018 | 0.933 | 1.110 |
| Manizales | −0.336 | 0.089 | 14.104 | 1 | <.001 | 0.715 | 0.600 | 0.852 |
| Cartagena | −0.215 | 0.100 | 4.658 | 1 | .031 | 0.806 | 0.663 | 0.980 |
| Constante | 0.889 | 0.182 | 23.746 | 1 | .000 | 2.432 | ||
B: regression coefficient; SD: standard deviation; DF: degrees of freedom; 95% CI: 95% confidence interval; OR: odds ratio; Sig: statistical significance.
Epilepsy is frequently accompanied by a number of comorbidities which require specific treatment. Of our sample, 7710 patients (55.9%) were receiving at least one drug belonging to one of the following drug groups, which reflects the presence of comorbidities and may result in drug–drug interactions: antihypertensives (n=4704, 61.0% of the sample), lipid-lowering drugs (n=3531, 45.8%), antidepressants (n=2829, 36.7%; 25.8% of these patients were treated with tricyclic antidepressants), antipsychotics (n=1546, 20.1%), anxiolytics (n=612, 7.9%), lithium (n=139, 1.8%), anti-dementia drugs (n=62, 0.8%), and methylphenidate (n=19, 0.24%). A total of 1020 patients (7.4%) concomitantly received 3 psychoactive drugs, 92 (0.66%) received 4 psychoactive drugs, and 5 (0.04%) received 5. We found statistically significant differences in concomitant medication between sexes: women were more frequently polymedicated than men (59.5% vs 51.9%, P<.001).
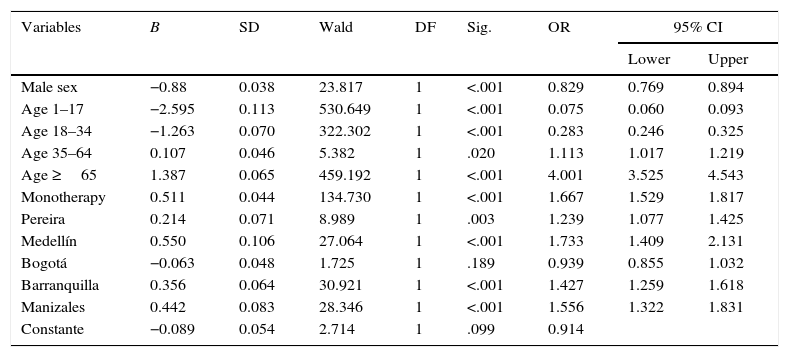
According to a binary logistic regression analysis of the association between concomitant medication and other variables, patients aged 35 to 64 or 65 or older, those receiving antiepileptics in monotherapy, and those treated in Pereira, Medellín, Barranquilla, or Manizales were significantly more likely to receive one or more drugs from another drug group. The variables male sex, ages 1 to 17 years, and ages 18 to 34 years were associated with a lower probability of concomitant medication (Table 3).
Variables associated with antiepileptic treatment and polymedication in a binary logistic regression model (Colombia, 2012).
| Variables | B | SD | Wald | DF | Sig. | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Male sex | −0.88 | 0.038 | 23.817 | 1 | <.001 | 0.829 | 0.769 | 0.894 |
| Age 1–17 | −2.595 | 0.113 | 530.649 | 1 | <.001 | 0.075 | 0.060 | 0.093 |
| Age 18–34 | −1.263 | 0.070 | 322.302 | 1 | <.001 | 0.283 | 0.246 | 0.325 |
| Age 35–64 | 0.107 | 0.046 | 5.382 | 1 | .020 | 1.113 | 1.017 | 1.219 |
| Age ≥65 | 1.387 | 0.065 | 459.192 | 1 | <.001 | 4.001 | 3.525 | 4.543 |
| Monotherapy | 0.511 | 0.044 | 134.730 | 1 | <.001 | 1.667 | 1.529 | 1.817 |
| Pereira | 0.214 | 0.071 | 8.989 | 1 | .003 | 1.239 | 1.077 | 1.425 |
| Medellín | 0.550 | 0.106 | 27.064 | 1 | <.001 | 1.733 | 1.409 | 2.131 |
| Bogotá | −0.063 | 0.048 | 1.725 | 1 | .189 | 0.939 | 0.855 | 1.032 |
| Barranquilla | 0.356 | 0.064 | 30.921 | 1 | <.001 | 1.427 | 1.259 | 1.618 |
| Manizales | 0.442 | 0.083 | 28.346 | 1 | <.001 | 1.556 | 1.322 | 1.831 |
| Constante | −0.089 | 0.054 | 2.714 | 1 | .099 | 0.914 | ||
B: regression coefficient; SD: standard deviation; DF: degrees of freedom; 95% CI: 95% confidence interval; OR: odds ratio; Sig: statistical significance.
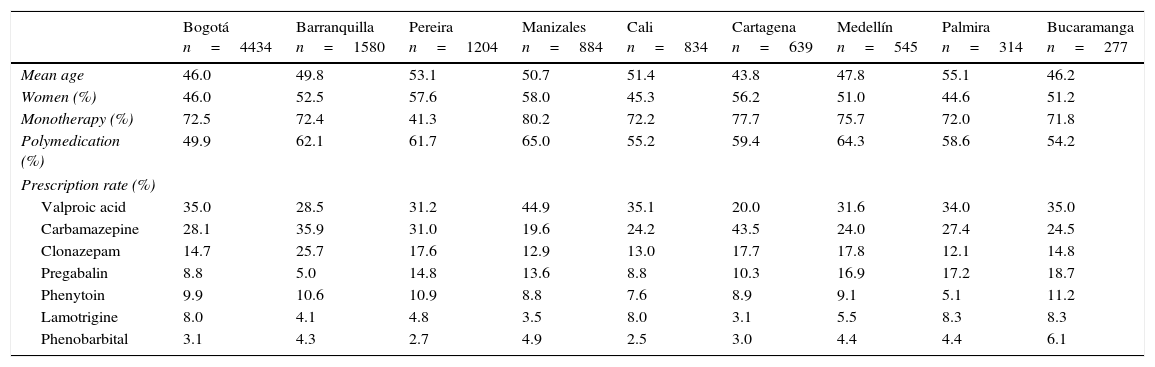
We compared demographic variables and prescription data between the 88 Colombian towns and cities included in this study. However, given the small number of patients in some municipalities, Tables 4 and 5 include only the 9 most populated cities, which account for 80.9% of this sample. We found significant differences in use of monotherapy and concomitant medication between cities. Antiepileptic consumption is expressed in DDD (Table 5) for ease of use in subsequent analyses.
Comparison of selected demographic variables and prescription data for antiepileptic drugs in 9 Colombian cities in 2012.
| Bogotá n=4434 | Barranquilla n=1580 | Pereira n=1204 | Manizales n=884 | Cali n=834 | Cartagena n=639 | Medellín n=545 | Palmira n=314 | Bucaramanga n=277 | |
|---|---|---|---|---|---|---|---|---|---|
| Mean age | 46.0 | 49.8 | 53.1 | 50.7 | 51.4 | 43.8 | 47.8 | 55.1 | 46.2 |
| Women (%) | 46.0 | 52.5 | 57.6 | 58.0 | 45.3 | 56.2 | 51.0 | 44.6 | 51.2 |
| Monotherapy (%) | 72.5 | 72.4 | 41.3 | 80.2 | 72.2 | 77.7 | 75.7 | 72.0 | 71.8 |
| Polymedication (%) | 49.9 | 62.1 | 61.7 | 65.0 | 55.2 | 59.4 | 64.3 | 58.6 | 54.2 |
| Prescription rate (%) | |||||||||
| Valproic acid | 35.0 | 28.5 | 31.2 | 44.9 | 35.1 | 20.0 | 31.6 | 34.0 | 35.0 |
| Carbamazepine | 28.1 | 35.9 | 31.0 | 19.6 | 24.2 | 43.5 | 24.0 | 27.4 | 24.5 |
| Clonazepam | 14.7 | 25.7 | 17.6 | 12.9 | 13.0 | 17.7 | 17.8 | 12.1 | 14.8 |
| Pregabalin | 8.8 | 5.0 | 14.8 | 13.6 | 8.8 | 10.3 | 16.9 | 17.2 | 18.7 |
| Phenytoin | 9.9 | 10.6 | 10.9 | 8.8 | 7.6 | 8.9 | 9.1 | 5.1 | 11.2 |
| Lamotrigine | 8.0 | 4.1 | 4.8 | 3.5 | 8.0 | 3.1 | 5.5 | 8.3 | 8.3 |
| Phenobarbital | 3.1 | 4.3 | 2.7 | 4.9 | 2.5 | 3.0 | 4.4 | 4.4 | 6.1 |
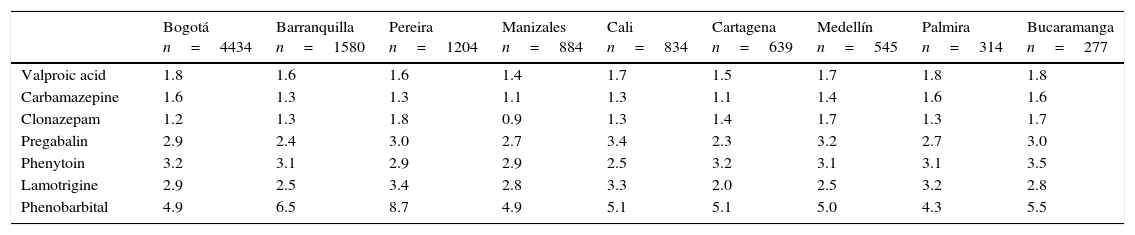
Relationship between the mean administered dose and the defined daily dose (DDD) of antiepileptics in 9 Colombian cities in 2012.
| Bogotá n=4434 | Barranquilla n=1580 | Pereira n=1204 | Manizales n=884 | Cali n=834 | Cartagena n=639 | Medellín n=545 | Palmira n=314 | Bucaramanga n=277 | |
|---|---|---|---|---|---|---|---|---|---|
| Valproic acid | 1.8 | 1.6 | 1.6 | 1.4 | 1.7 | 1.5 | 1.7 | 1.8 | 1.8 |
| Carbamazepine | 1.6 | 1.3 | 1.3 | 1.1 | 1.3 | 1.1 | 1.4 | 1.6 | 1.6 |
| Clonazepam | 1.2 | 1.3 | 1.8 | 0.9 | 1.3 | 1.4 | 1.7 | 1.3 | 1.7 |
| Pregabalin | 2.9 | 2.4 | 3.0 | 2.7 | 3.4 | 2.3 | 3.2 | 2.7 | 3.0 |
| Phenytoin | 3.2 | 3.1 | 2.9 | 2.9 | 2.5 | 3.2 | 3.1 | 3.1 | 3.5 |
| Lamotrigine | 2.9 | 2.5 | 3.4 | 2.8 | 3.3 | 2.0 | 2.5 | 3.2 | 2.8 |
| Phenobarbital | 4.9 | 6.5 | 8.7 | 4.9 | 5.1 | 5.1 | 5.0 | 4.3 | 5.5 |
This study allowed us to determine the prescription pattern of the antiepileptic drugs most frequently used in patients registered with the SGSSS. Our data can be used by healthcare providers in decisions aiming to improve care for patients with epilepsy and other neuropsychiatric disorders.
Our data demonstrate significant differences in the antiepileptics prescribed to patients of different sexes and age groups: in those younger than 35, the drugs are more frequently prescribed to men, whereas in those older than 35, they are more frequently used in women. Young men with epilepsy are treated more frequently in monotherapy and receive fewer concomitant medications than men older than 35. However, only 28% of all epileptic patients are younger than 35; we may therefore conclude that most patients treated with antiepileptic drugs present both epilepsy and age-related comorbidities.19–24 We should point out that, since the list of drugs allowed by the Compulsory Health Plan is fixed, more than 74.8% of all patients are treated with drugs included in that list, although patients may also be treated with other drugs that are not listed if a request by a TSC or guardian is approved.18
The high use of classic antiepileptics (72.9%) in our sample contrasts with data reported in the literature; according to recent studies, classic antiepileptics are losing ground to newer ones due to the therapeutic potential and lower risk of adverse effects of the latter, and to the increased use of these new antiepileptics for neuropathic pain.21 In addition, patients in our sample received higher doses than recommended for most of the antiepileptic agents (Table 1) except for carbamazepine and clonazepam; this fact may reflect failure to control the disease with other agents leading to the need to increase the dose, or use of antiepileptics for indications that are not preapproved.18,21 Interestingly, we found a high percentage of patients receiving phenobarbital, a drug presenting substantial disadvantages compared to other less toxic antiepileptic agents.20,22,23
Other studies have reported similar figures for combination therapy with antiepileptics (17%–42%).20,22,23 Combination therapy may increase the risk of adverse effects in these patients; however, concomitant prescription of classic and new antiepileptics may constitute a more effective treatment approach in those patients in whom a single agent fails to achieve seizure control. In addition, some of these agents are administered at higher doses than recommended and may therefore result in more adverse reactions and decreased treatment adherence.19,25–28
Based on the list of concomitantly prescribed drugs, the most prevalent comorbidities were found to be hypertension, dyslipidaemia, and depression; our data agree with those reported in other studies.9,14,16 We should be mindful of the potential interactions with calcium channel blockers: carbamazepine and phenobarbital may induce enzymes of cytochrome P450, responsible for drug metabolism, which would decrease the levels of calcium channel blockers. Likewise, treatment with antidepressants may prolong the Q-T interval, resulting in more pronounced anticholinergic effects and sudden cardiac death in patients with a history of cardiovascular risk; these drugs can also decrease the seizure threshold in epileptic patients.26 Evaluating the risks and benefits of these drug combinations includes considering other antidepressants which do not increase the negative effects of medication.28–31 Schizophrenia, anxiety, bipolar affective disorder, Alzheimer disease, and attention deficit/hyperactivity disorder are frequent comorbidities in patients treated with antiepileptic drugs. The potential for interaction between antiepileptics and the psychoactive drugs necessary to manage these conditions increases the risk of central and autonomic nervous system alterations and may affect the quality of life of epileptic patients.10–13,17,28
We were not surprised to find differences in prescription patterns between the Colombian towns and cities included in our study, as well as differences in the frequency of use of some antiepileptics (Tables 2–5); pharmacoepidemiological studies in Colombia consistently reveal high variability in medical care, and especially in prescription patterns.30
Our study has a number of limitations: data were obtained from databases rather than from patients or prescribing doctors, and patients’ medical histories were not consulted. These limitations may be overcome in the studies designed for the second phase of this line of research. We need more data on the classification of epilepsy, the incidence of adverse effects, treatment adherence, the degree of seizure control, and relapses. We do not know whether the antiepileptic drugs prescribed to our patients were appropriate since we did not evaluate baseline or follow-up data. As our study included a set population who received the drugs included in a specific list, the data can only be extrapolated to similar populations.
According to prescription patterns in our population, the most frequently prescribed antiepileptics are those included in the list of essential medicines in Colombia; they are most commonly prescribed in monotherapy and some of them are administered at higher doses than recommended. We found a considerable number of patients receiving 2, 3, and even 4 psychoactive drugs; the cause of this phenomenon is unknown. Polymedication increases the risk of extrapyramidal and autonomic adverse reactions. Hypertension, dyslipidaemia, depression, schizophrenia, anxiety, bipolar affective disorder, Alzheimer disease, and attention deficit/hyperactivity disorder were the most common comorbidities; the presence of these disorders should make clinicians aware of the importance of improving epilepsy treatment for these patients.
We need to determine the possible reasons for using higher doses than recommended and the potential indications of these drugs. Studies in this field should aim to improve prescription criteria in patients registered with the SGSSS of Colombia.30,31 The effectiveness of antiepileptic agents should be analysed in this group of patients to assess the appropriateness of doses and concomitant medications; future research must focus on developing tools for reducing the risk of drug–drug interactions.
FundingThe study was financed by Universidad Tecnológica de Pereira and Audifarma S.A.
This study has not been presented at any of the SEN's meetings.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Morales-Plaza CD, Machado-Alba JE. Patrones de prescripción de antiepilépticos en pacientes colombianos afiliados al Sistema General de Seguridad Social en Salud. Neurología. 2017;32:6–14.