El tromboembolismo venoso (TEV) es una de las principales causas de mortalidad tras la cirugía bariátrica. El objetivo de este estudio fue evaluar la eficacia de la tromboprofilaxis (enoxaparina y rivaroxabán) en pacientes postoperados con gastrectomía en manga laparoscópica.
MétodosRealizamos este estudio prospectivo en pacientes que se sometieron a gastrectomía en manga laparoscópica desde abril de 2017 hasta enero de 2021. Todos los pacientes recibieron tromboprofilaxis con enoxaparina o rivaroxabán después de la operación. Registramos la incidencia de TEV confirmada en estos pacientes que se habían sometido a gastrectomía en manga laparoscópica y habían recibido tromboprofilaxis dentro de los 3 meses posteriores a la cirugía bariátrica.
ResultadosEstudiamos 1.000 pacientes con gastrectomía en manga divididos en dos grupos; El grupo 1 (n= 295 (59 %) mujeres y 205 (41 %) hombres) recibió enoxaparina, y el grupo 2 (n= 315 (63 %) mujeres y 185 (37 %) hombres) recibió rovaroxabán (promedio edad 43,8±3,5 45,2±3,1, respectivamente) y fueron seguidos durante 3 meses. La incidencia acumulada de TEV postoperatoria sintomática a los 3 meses fue del 0,001%. Este evento ocurrió después del alta hospitalaria. No se informaron casos de mortalidad relacionada con TEV para el grupo 1. Se diagnosticó un caso de TEV para el grupo 2 después de 3 meses.
ConclusionesLa tasa de TEV después de la cirugía bariátrica no es considerable, pero con el aumento global de la obesidad y la necesidad asociada de cirugía bariátrica como una forma efectiva de reducir el peso y la incidencia de morbilidades relacionadas con la obesidad, la TEV sigue siendo una complicación prevenible esencial en esta población. Por tanto, la tromboprofilaxis parece ser eficaz tras la cirugía bariátrica sin aumentar el riesgo de hemorragia.
Venous thromboembolism (VTE) refers to inappropriate blood clots in the veins. VTE encompassing deep vein thrombosis (DVT) in which clots are formed in the deep veins of the body; and pulmonary embolism (PE), which occurs when a clot breaks and enters the arteries of the lungs.1 The incidence of VTE in the United States is 900,000 people annually, and the incidence of mortality is 60,000-100,000 each year.2 Risk factors for VTE include male gender, higher BMI, obesity hypoventilation syndrome, pulmonary hypertension, older ages, prolonged immobility, multiple traumas, malignancy, major surgery, personal history of VTE, operation time and the type of bariatric surgery.3
Obesity, a public health issue, increases the risk of other diseases, such as diabetes mellitus, malignancies, gastrointestinal disorders, depression, atherosclerotic cardiovascular diseases, hypertension, and VTE.4 VTE is a growing public health problem and patients with obesity have a moderate to high risk for pulmonary embolism, this fact has been studied since 1997.5
The prevalence of obesity has tripled in the last three decades and surgical methods have been explored to reduce obesity in a patient.6 Based on World Obesity Atlas 2022 prediction, one billion people will be living with obesity including 1 in 5 women and 1 in 7 men by 2030.7 Bariatric surgery has evolved in the United States and worldwide over the past two decades and reduces the risk of potentially life-threatening weight-related health problems. Most bariatric surgeries include Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG)8 . However, bariatric surgery is not free from complications and is associated with 0.1% - 1.1 mortality.9,10 However bariatric surgery is categorized in minimally invasive surgery, but it has a series of post operative complications including dumping syndrome, anastomic leakages, malnutrition, VTE, bowel obstruction, and sepsis.11 Among these complications, VTE is a major cause of postdischarge mortality after bariatric surgery.12 The overall 30-day incidence of postdischarge VTE following bariatric surgery was 0.29%.13 Although the amount of VTE after bariatric surgery is not very high, still is the major cause of postdischarge mortality, as well as the increasing prevalence of obesity and subsequently bariatric surgeries have seen a significant increase in VTE complications.
VTE is a preventable disease, and thromboprophylaxis is the main strategy to reduce VTE-induced mortality after bariatric surgery.14 Enoxaparin, which is sold inder the brand name Lovenox®, is used to treat and prevent deep vein thrombosis and embolism during pregnancy and following certain types of surgery such as SG, and RYGB. In addition, Rivaroxaban is under the brand of XARELTO®, and is usually prescribed for treatment and prevention of blood clots. It may prevent other clinical conditions such as the risk of ischemic strokes, as well as deep vein thrombosis (DVT), and embolic events.15 The main aim of this study is to evaluate the efficiency of thromboprophylaxis on VTE, including Enoxaparin and Rivaroxaban, in 1000 patients following sleeve gastrectomy surgery. To the best of our knowledge, this is the first study on evaluation of thromboprophylaxis medicine outcomes among laparoscopic sleeve gastrectomy patients in this large scale population.
Materials and methodsStudy designWe performed a population-based, retrospective study of patients who underwent laparoscopic sleeve gastrectomy surgery at Erfan Hospital, Tehran, Iran from Apr 2017 to Jan 2021 under supervision of *** and his team. We included adult patients (≥35 yrs.), with BMIs ≥40 kg/m2 that underwent laparoscopic sleeve gastrectomy surgery. The mean operation time was 55 min. There were two groups of patients and we tried to classify the patients equally and randomly into those two groups to have equal number of patients in each group. Group 1 (n=500) received Enoxaparin (ATC code: B01AB05) 2.5 mg every 12 hours for thromboprophylaxis. Group 2 (n=500) received Rivaroxaban (ATC code: B01AF01) 10 mg every 24 hours. Based on the guidelines and recommendations, thromboprophylaxis should be started on the first day of admission, i.e., as soon as there is a risk of development of VTE.12 The physical status classification system (ASA) and The Edmonton Obesity Staging System (EOSS) scores were archived on patients’ records. The study was done based on the guidelines set by the Institutional Review Board of Erfan Hospital, Tehran, Iran. The Ethics Committee (Helsinki board number: 2017245) approved this study. The protocol was approved by Erfan Hospital Ethics Committee which is registered under the registration number IR.TAHO.FRE.PER.1398.087. Follow-up data on identified patients were extracted from the day of admission to the end of the third month or death. In this study we assessed the incidence of VTE, for 3 months after laparoscopic sleeve gastrectomy surgery in all patients who received Enoxaparin or Rivaroxaban. The definition of bleeding was based on the International Society on Thrombosis and Hemostasis, in which major bleedings are defined as any type of hemorrhage that result in death, are life-threatening, cause chronic sequelae or consume major health-care resources, causing a fall in hemoglobin level lower that 20gL−1 (1.24mmolL−1), or leading to transfusion of two or more units of whole blood or red cells.16,17
Statistical analysisData were analyzed using SAS (statistical analysis systems) version 9.4.
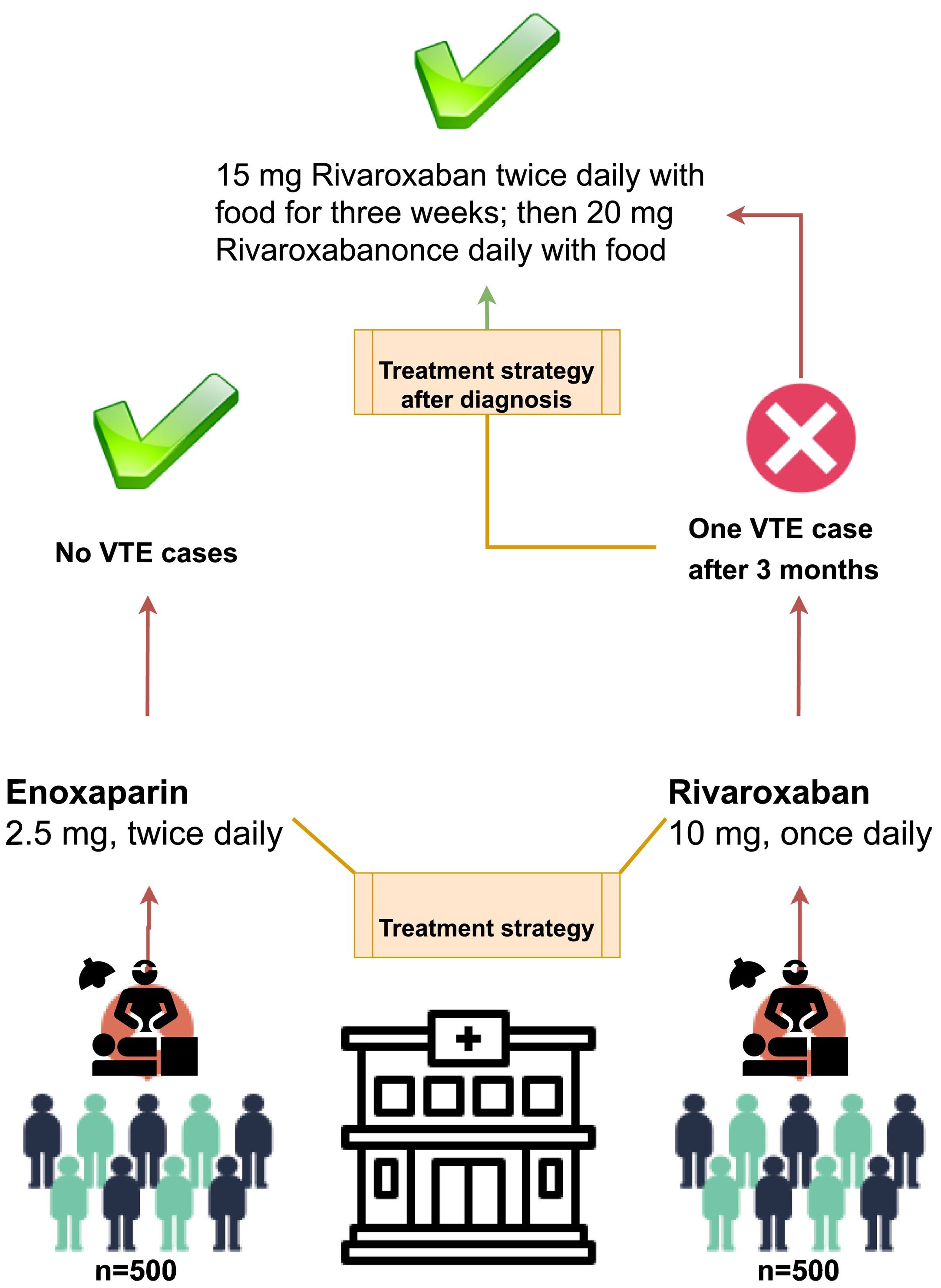
ResultsIn total, 1,000 patients underwent laparoscopic sleeve gastrectomy surgery between Apr 2017 and Jan 2021. All of subjects completed at least 3 months of follow-up. Patient’s characteristics are presented in Table 1. The mean age of all patients was 44.5 years old (standard deviation±3.3 yr) and most were under the age of 50. There were more females (61%) than males (39%). The median body weight was 127.6 kg. The mean BMI of subjects was 48.4±3.65 and the BMIs of 16.4% of patients were ≥55 kg/m2. The median follow-up time was 3 months. The age and sex of patients when they underwent bariatric surgery are illustrated in Table 1. The mean ASA score of patients was 2.1 (standard deviation 0.7) and EOSS grade was stage 2.3 (standard deviation 1.1). Fig. 1 presents more details on the strategies we considered in this study with summary of results from the target groups undergoing bariatric surgery whom were evaluated for VTE complications.
Patient’s characteristics when they underwent sleeve gastrectomy.
| Group 1 | Group 2 | |
|---|---|---|
| Number of patients | 500 | 500 |
| Treatment strategy and prescribed doses | Enoxaparin 2.5 mg twice daily | Rivaroxaban 10 mg once daily |
| Mean age | 43.8±3.5 | 45.2±3.1 |
| Mean BMI | 47.2±1.7 | 49.6±5.6 |
| ASA | 2.1 ( SD 0.8) | 2.1 (SD 0.7) |
| EOSS | 2.3 (SD 0.9) | 2.3 (SD 1.1) |
| Gender n (%) | Female 295 (59%)Male 205 (41%) | Female 315 (63%)Male 185 (37%) |
| Patients diagnosed with VTE/total subjects | 0/500 | 1/500 (0.05%)Female 0/315 (0%)Male 1/185 (0.54%) |
The cumulative incidence of symptomatic postoperative VTE at 3 months was 1/1000 patients or 0.001%. The only VTE case observed was a 44-year-old male with BMI 46.2 kg/m2, with no history of VTE (and no family history of VTE) or smoking who received Rivaroxaban same as other patients in group 2. Patient had no history of steroid/immunosuppressant use in his life. This case was diagnosed 23 days after hospital discharge and laboratory variables included serum creatinine (0.92 mg/dL), albumin (4.10 g/dL), hematocrit (40.95%), and platelet count (265.32 109/L) for the patient after VTE diagnosis. Details regarding this patient are demonstrated in Table 2. At the 3-month follow up period of all other patients underwent bariatric surgery and received Enoxaparin or Rivaroxaban, there was no reported VTE-related mortality.
Details regarding the VTE patient.
| Patient’s characteristics | Notes |
|---|---|
| Treatment strategy and prescribed doses | Rivaroxaban 10 mg once daily |
| Age | 44 |
| BMI | 46.2 |
| Gender | Male |
| ASA | 2.0 |
| EOSS | 2.2 |
| Documented venous insufficiency | No |
| History of VTE | No |
| History of PTE | Yes |
| History of Smoking | No |
| Varicose veins | No |
| Oral contraceptive use | - |
| Family history of VTE | No |
| VTE treatment after diagnosis | 15 mg twice daily with food for three weeks; then 20 mg once daily with food |
Bariatric surgery has a series of complications such as VTE, which is the major cause of post-discharge mortality following bariatric surgery.12 Increased age, weight, male gender, and having the history of VTE are the main risk factors for postoperative VTE.18 Although the rate of VTE after bariatric surgery is not very high, with increasing the rate of obesity and the need for bariatric surgery as an effective approach to reducing weight, VTE remains an important preventable complication in the populations.12,19
Since patients with obesity undergoing bariatric surgery are at risk of thromboembolic complications18 and based on the guidelines issued by the American College of Chest Physicians that recommends the use of thromboprophylaxis for bariatric surgery patients.20 In our study of patients undergoing bariatric surgery, all patients received thromboprophylaxis with each Enoxaparin or Rivaroxaban postoperatively and up until discharge from hospital for VTE prophylaxis.
All patients in this study received a fixed dose of Enoxaparin 2.5 mg twice daily or Rivaroxaban 10 mg once daily with or without food. The incidence of VTE at 3 months after bariatric surgery was 0.001%. The only male subject diagnosed with VTE was 44 years old with no history of VTE, smoking, documented venous insufficiency or varicose veins but he had history of pulmonary thromboendarterectomy (PTE). After VTE diagnosis, the patient received 15 mg of Rivaroxaban twice daily with food for three weeks, then 20 mg of Rivaroxaban prescribed once daily with food. Overall laboratory tests demonstrated normal levels of creatinine (0.92 mg/dL), albumin (4.10 g/dL), hematocrit (40.95%), and platelet count (265.32 109/L) even after VTE diagnosis. More information on clinical background of this patient is presented in table 2. The ASA score for all patients involved in this survey was ASA II which is considered a morbidly obese condition and is defined as mild systemic disease. On the other side, EOSS scoring analysis revealed that the target group in this study had 2.3 EOSS score. EOSS stage 2 indicated that patient has established obesity-related comorbidities requiring medical intervention. The mortality rate was zero at the 3-month follow-up period which is mainly due to the low population of this study. Therefore, we have approved that thromboprophylaxis might be effective in preventing VTE in patient undergoing bariatric surgery. However, further studies with large population, long-term follow-up and considering more clinical evaluations are needed to strongly confirm this relationship and efficacy of those thromboprophylaxis medicines on VTE complications after bariatric surgery. In this study we tried to focus on single-ethnicity target group, and its population-based nature, and with single-center surgical team performances, with follow-up of patients in the community. Furthermore, researchers can continue this survey on patients with higher scores of ASA and EOSS which consists of individuals with higher risks of post-operative complications.
In addition, in this study, the VTE was observed 23 days after discharging the patient from the hospital with laboratory variables including serum creatinine (0.92 mg/dL), albumin (4.10 g/dL), hematocrit (40.95%), and platelet count (265.32 109/L) after VTE diagnosis. This result is consistent with the findings reported across several published studies reporting that most VTE events occurred in bariatric surgery patients within 3 months after discharging from the hospital.21–27 Therefore, treatment with thromboprophylaxis with follow-up of patients at least for 3 months after hospital discharge is essential and should be considered for patients following bariatric surgery.
ConclusionVTE is a preventable complication that has a risk of mortality after bariatric surgery. However, treatment of thromboprophylaxis with Enoxaparin and Rivaroxaban might be an effective strategy after bariatric surgery with a low incidence of severe bleeding complications. The only patient diagnosed with VTE, had no history of VTE, smoking, varicose vein, and family history of VTE, but he had history of PTE. This information can be taken into account during and after bariatric surgery.
Authors' contributionsConception and design: TA; Administrative support: TA; Collection and assembly of data: BB, JO; Data analysis and interpretation: BB, JO; Manuscript writing: All authors; Final approval of manuscript: All authors.
Funding statementThis is a self-funded study.
I would like to appreciate all who helped us to exert this study.