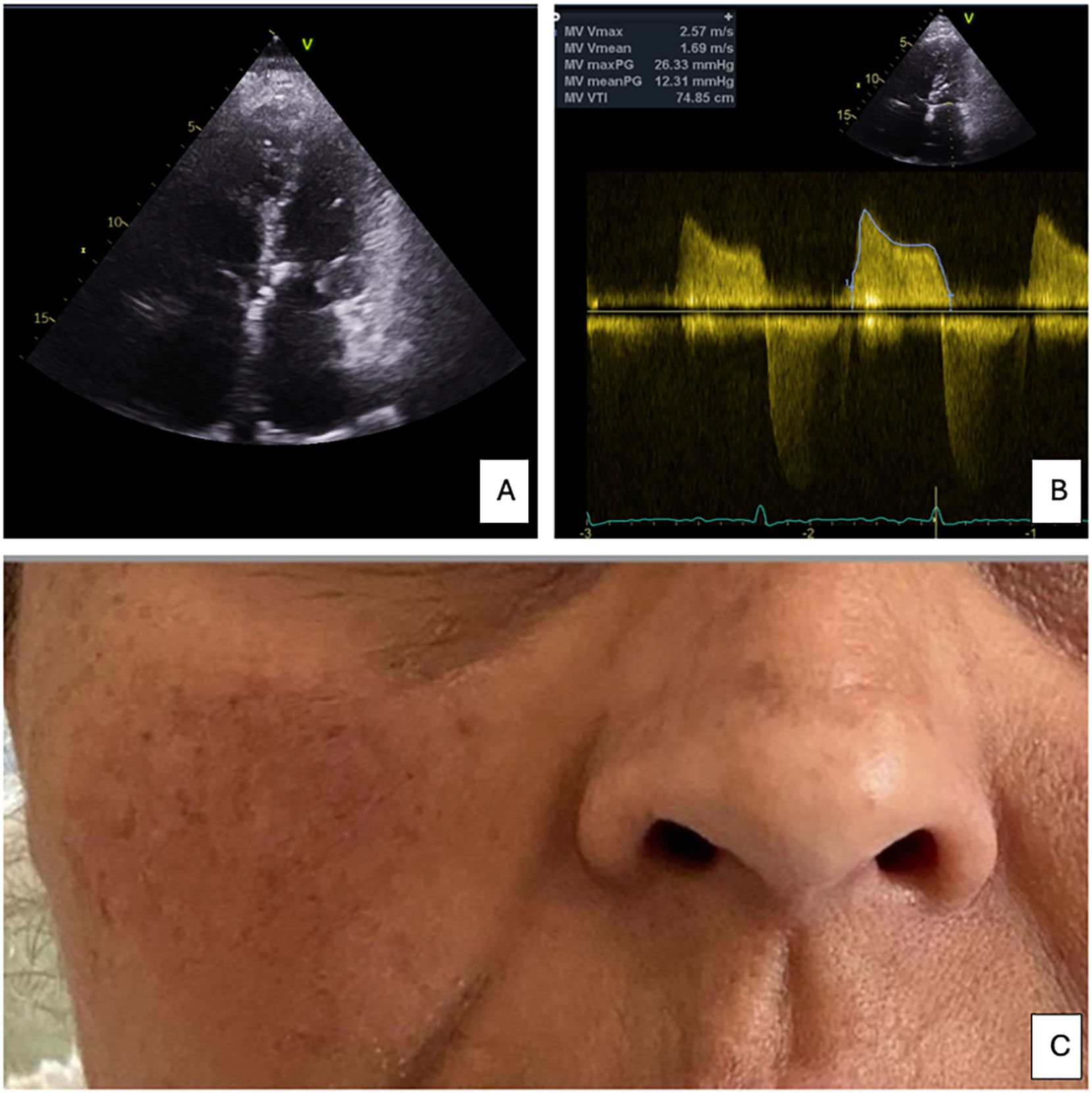
A 45-year-old woman presented with progressive dyspnea on exertion, palpitations, and a malar rash across her cheeks and nasal bridge (Fig. 1, C). She reported no history of recurrent joint pain, photosensitivity or oral ulcers. Physical examination revealed arrhythmic sounds, without any murmur detected, and erythematous rash sparing the nasolabial folds. An echocardiogram showed severe mitral stenosis (MS) with a valve area of 1.2 cm2 (0.85cm2 3D area) and a mean gradient of 12 mmHg, consistent with chronic rheumatic heart disease, signs of pulmonary hypertension and mildly reduced right ventricular function (Fig. 1, A and B). Laboratory workup included positive antinuclear antibodies, but anti-dsDNA was negative, making systemic lupus erythematosus (SLE) a less likely primary etiology of the rash. Her MS had been managed three years previously with percutaneous mitral balloon valvuloplasty, so she was referred to the Heart Team for potential valve surgery.
DiscussionMitral stenosis, which is frequently caused by rheumatic heart disease, often presents with symptoms of heart failure and palpitations (1). Mitral facies, a classic but frequently underrecognized sign of MS, manifests as plethoric or pinkish-purple patches on the cheeks. Although rare in developed countries, it is seen in patients with untreated, chronic MS and pulmonary hypertension. Mitral facies may resemble malar rashes associated with SLE, erysipela, rosacea, or pellagra. In this case, however, the patient's rash was painless, purplish, and lacks systemic symptoms. The pathogenesis is thought to involve peripheral vasoconstriction due to low cardiac output, and may be worsened by pulmonary hypertension, atrial fibrillation, and hypoxemia. Echocardiography remains the cornerstone for diagnosing MS, assessing the mitral valve area, and guiding management decisions. In this patient, echocardiography revealed severe mitral stenosis, signs of pulmonary hypertension and mildly reduced right ventricular function. She also had a history of atrial fibrillation. In rare instances, patients with significant MS may not present with a classic diastolic murmur, as in this case.
This case highlights the importance of a comprehensive evaluation for non-cardiac manifestations, such as rash, which may indicate advanced MS. Mitral facies may be a marker of long-standing impaired cardiac output and severe pulmonary hypertension. Although a rash may initially suggest autoimmune disease, the presence of cardiac findings should prompt clinicians to investigate primary valvular pathology.