Syncope of unknown etiology can serve as an initial manifestation of pulmonary embolism (PE). Furthermore, syncope may lead to head trauma, increasing the risk of cerebral hemorrhage. However, delayed acute subdural hemorrhage (DASH) following PE-related syncope is rarely reported.
A 72-year-old woman was brought to the emergency department by her family after experiencing a sudden episode of syncope. She reported a two-week history of exertional dyspnea and a non-productive cough. Her medical history included hypertension, which was managed with oral antihypertensive medications, as well as pain and swelling in her right lower extremity three months prior. On physical examination, her vital signs were as follows: temperature 36.6 °C, pulse 116 beats per minute, respiratory rate 26 breaths per minute, and blood pressure 130/70 mmHg. She was alert, spoke fluently, and exhibited no signs of skin trauma, lower extremity swelling, or impaired limb movement.
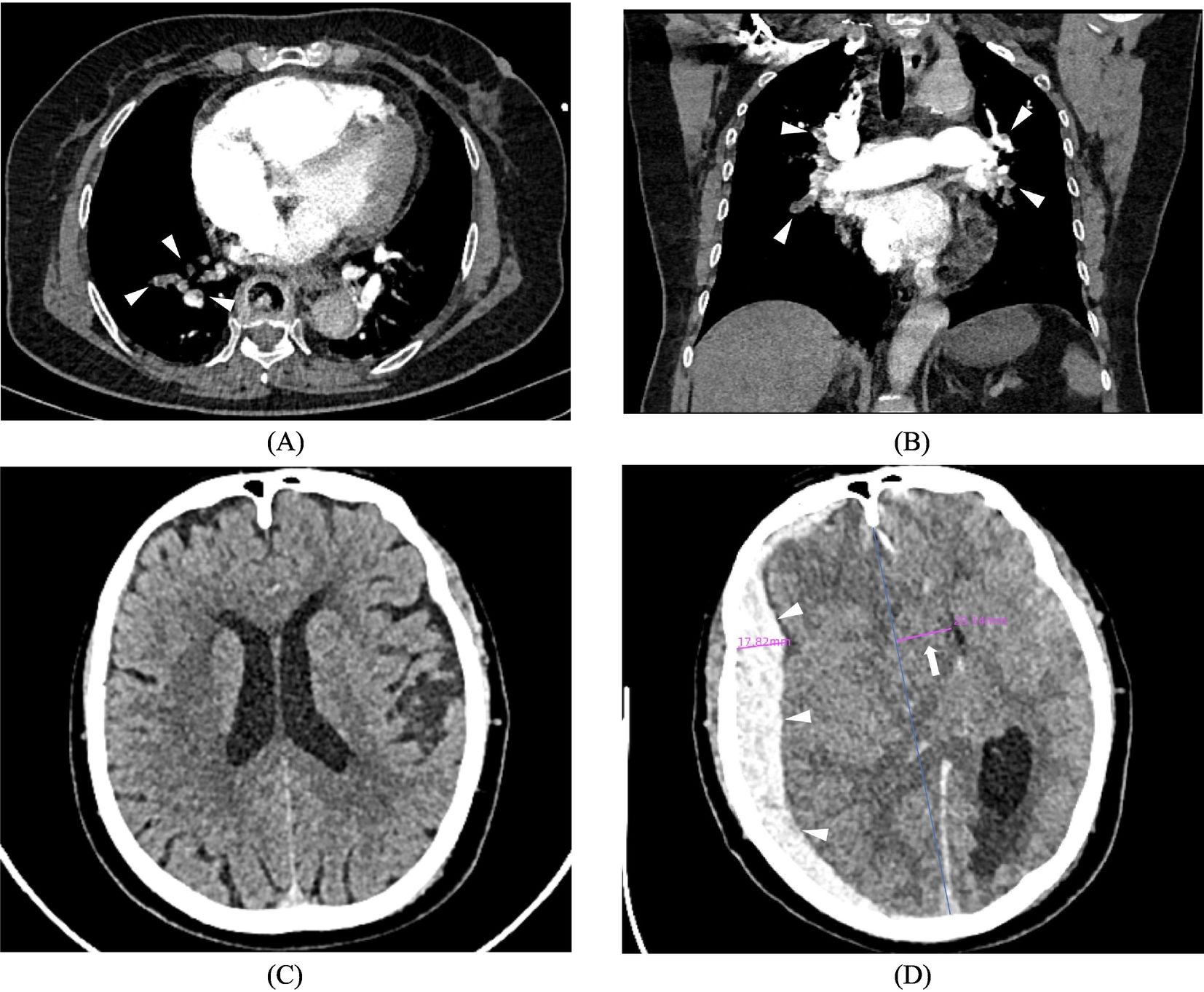
Laboratory tests revealed an elevated D-dimer level of 4.82 mg/L FEU (reference value, <0.5), while Troponin I and NT-proBNP levels were within normal limits. Arterial blood gas analysis showed a pH of 7.365 (reference range, 7.35–7.45), PO2 of 42 mmHg (reference range, 80–100), PCO2 of 25.7 mmHg (reference range, 35–45), and SaO2 of 77% (reference range, 91.9–99.0). Electrocardiography revealed a complete right bundle branch block. Emergency pulmonary artery CTA demonstrated multiple filling defects in both pulmonary arteries (Fig. 1A, B), confirming the diagnosis of PE. In contrast, head CT showed no evidence of hemorrhage or infarction (Fig. 1C).
Emergency pulmonary artery CTA in axial (A) and coronal (B) views revealed multiple filling defects in both pulmonary arteries (arrows), confirming the diagnosis of pulmonary embolism. (C) Initial emergency head CT showed no evidence of hemorrhage or infarction. (D) Repeat head CT revealed a large subdural hemorrhage (arrows) in the right frontotemporal-parietal-occipital region, with a significant midline shift (long arrow) and cerebral herniation.
Further investigation after admission revealed a venous blood glucose level of 18.29 mmol/L (reference range, 3.9–6.1) and glucosuria (3+). Bedside venous ultrasound of the lower limbs showed a pulsatile spectrum in the common femoral vein. Cardiac ultrasound findings were consistent with moderate tricuspid regurgitation and suspected pulmonary hypertension. After ruling out contraindications, the patient was initiated on enoxaparin anticoagulation therapy. Fifteen hours later, she developed a headache that progressively worsened over the next three hours, accompanied by vomiting and loss of consciousness. A repeat cranial CT scan revealed an extensive subdural hemorrhage on the right side, accompanied by cerebral herniation (Fig. 1D). Despite undergoing emergency intracranial hematoma evacuation and decompression surgery, her condition deteriorated, and she passed away 43 h after the procedure.
Research indicates that the incidence of delayed cerebral hemorrhage is approximately 7.6 per 1000 cases. DASH is rarely reported in the literature and primarily occurs in elderly individuals with mild traumatic head injury, particularly those on antiplatelet or anticoagulant therapy. However, cases have also been documented in young patients without coagulation abnormalities or identifiable risk factors, such as medication use. In this article, we present the first reported case of DASH associated with syncope due to PE, which significantly complicates the treatment strategy. Although the patient received one day of anticoagulant therapy, preoperative coagulation studies—including PT, APTT, and INR—were within normal ranges, effectively ruling out anticoagulation as a contributing factor to the hemorrhage.
In summary, patients with PE may develop subdural hemorrhage secondary to syncope. Given the potential for delayed onset and life-threatening consequences, clinicians should maintain a high index of suspicion and consider repeat head CT scans, particularly within the first 24 h after the syncopal episode.
Ethical considerationThis study was conducted in accordance with the principles of the Declaration of Helsinki. Ethics committee approval is not required for case reports at our institution. Informed consent for publication was obtained from the patient's son.
FundingNo funding was received for this work.
The authors of the present manuscript declare no conflicts of interest.