Pleural effusion may occur in patients with rheumatoid arthritis (RA), typically as an exudate but in rare occasions has features of pseudochylothorax (chyliform or cholesterinic effusion). Although this uncommon type of cholesterol-rich pleural effusion is linked more frequently to tuberculosis (54%), it may be present in around 9% of patients with RA.1,2
We present a 91-year-old man with a 22-years history of RA, on treatment with oral prednisone 5mg daily, presented at the emergency department with fever, hypotension and pulse oximetry saturation of 92% while receiving antibiotic treatment for a urinary tract infection. On admission, the patient had 38.2°C temperature, tachypnoea, hypoventilation on left lung as well as ulnar deviation and a palpable nodule on his left hand. His past medical history was otherwise remarkable for apnoea-hypopnoea syndrome requiring continuous positive airway pressure, and a bladder neoplasia treated with transurethral resection.
A chest X-ray showed a left pneumothorax, without evidence of recent trauma or respiratory symptoms. A computed tomography displayed findings consistent with a left hydropneumothorax. Following a thoracentesis, a purulent/milky material was obtained, and samples were sent for biochemistry, microbiology and anatomical pathology analysis. The pleural fluid's (PF) biochemical analysis was consistent with an exudate according to Light's criteria (PF-LDH/srm-LDH >0.6), with elevated cholesterol (946 mg/dL), low triglycerides (57 mg/dL) and glucose (17 mg/dL).
Stain and cultures for common microorganism and tuberculosis were negative. The anatomical pathology results were consistent with an inflammatory pattern, without malignant features.
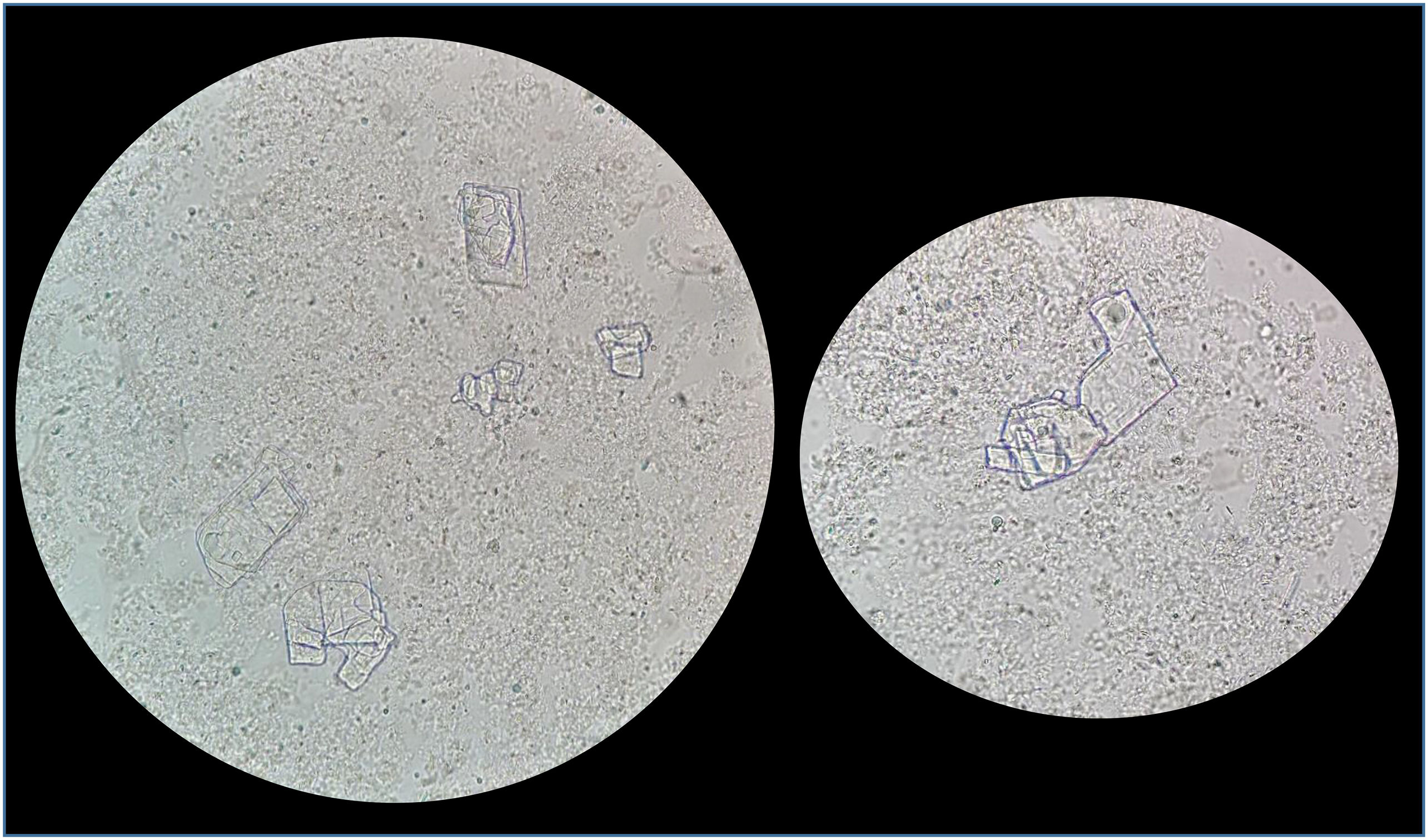
A triglyceride concentration >110 mg/dL confirms chylothorax and, contrarily, <50 mg/dL rules lipid effusions out. If the triglyceride concentration is between 50-110 mg/dL, the clear distinction between chylothorax and pseudochylothorax requires electrophoretic analysis of lipoproteins, quantifying chylomicrons, which confirm chylothorax.4 This is a laborious and expensive technique, currently not implemented in our centre. But further microscopic examination of the fluid revealed cholesterol crystals of irregular rhomboid-shaped with a notch on one side (Fig. 1), confirming the diagnosis of pseudochylothorax. Tuberculosis was confidently ruled out given low adenosine deaminase (<45 U/L) and interferon gamma (0 pg/mL) values. A pseudochylotorax was confirmed in the context of a long-standing seropositive RA in a patient with no previous disease modifying drugs, and pulmonary nodules.
The patient underwent a percutaneous procedure for chest tube drainage followed by pleurodesis with doxycycline. In addition, prednisone dose was increased to 30 mg, and leflunomide was initiated to control RA inflammatory activity. The patient presented full resolution during follow-up with the aforementioned measures and respiratory physiotherapy.
Pseudochylotorax in the context of RA is a rare complication with only a few examples described in the literature. Most of the cases are reported as asymptomatic right-sided pleural effusions, although patients sometimes present with dyspnoea. It is associated with middle-aged men, long-standing RA and the presence of rheumatoid nodules. Thickening of the pleura is characteristic and believed to be the cause of the fluid accumulation since it presumably blocks the drainage into the lymphatic system. Within this pathophysiological context, the neutrophil and red blood cells are lysed and the cholesterol and lecithin-globulin complexes are released.2,3 Nevertheless, as Horta-Bass G. said, a number of patients without pleural thickening have been described,3,5 implying that other pathogenic mechanisms are possible.
Some biochemical parameters are also common between patients. Although pseudochylothorax is a non-specific exudate, some laboratory features help in the diagnosis. The presence of cholesterol crystals is confirmatory, but it must be noted that it is absent in approximately 10% of the cases.3 Such crystals have satiny luster, with a characteristic rhomboidal shape. Remarkably, when under polarized light microscopy they show birefringence.1
Other laboratory data supporting the diagnosis are cholesterol concentrations >200 mg/dL, triglycerides <110 mg/dL and cholesterol/triglycerides ratio >1.1,3 The latter parameter is more sensitive (97.4%), since there are cases where cholesterol and triglyceride concentrations do not increase or decrease excessively, but the ratio remains affected.3 In contrast, glucose concentrations <60 mg/dL have been described in 70–80% of rheumatoid effusions. As for pH, the effusion fluid is usually acid with values below 7.35–7.30.4
In summary, the diagnosis of pleural effusions requires a combination of biochemical, microbiological and anatomopathological analysis as well as a detailed clinical history, physical examination and imaging tests, highlighting the relevance of communication between different hospital departments.
Ethical disclosuresNo included since there are no personal details of patient, including illustrations.
FundingNone declared.