Retinopathy is one of the most common microvascular complications caused by diabetes, which occurs due to changes in blood capillaries. One of the most important factors to determine the progression of retinopathy is measuring HbA1C. This study aimed to investigate the relationship between glycosylated hemoglobin levels, blood pressure (systolic and diastolic), and triglycerides with DRP in the population of diabetic patients.
MethodsThis descriptive and analytical study was conducted on 80 diabetic patients referred to Hafiz Sabzevar Diabetes Clinic in 1400. Based on fundoscopic examination, patients were divided into three general categories: patients without retinopathy, patients with proliferative diabetic retinopathy, and patients with non-proliferative retinopathy. Patient information was collected through a demographic questionnaire (including age, sex, insulin or oral drug use, and fasting blood sugar level) and a researcher-made checklist (including HbA1C, systolic blood pressure, diastolic blood pressure and triglycerides). Data were analyzed with spss 28. Descriptive statistical tests, ANOVA and Bonferroni's post hoc test were used for analysis.
ResultsThe results of the study showed that there is a significant difference in HbA1C, SBP and DBP levels between the three groups (P = 0.000). Post Hoc (Bonferroni) test was used to accurately determine this significant difference. The data showed that both retinopathy groups (NPDR and PDR) had higher levels of HbA1C and blood pressure (SBP and DBP) compared to the non-retinopathy group and this difference was statistically significant (P = 0.000). However, there was no significant difference between the three groups in terms of triglyceride levels (P = 0.96).
ConclusionHigh levels of glycosylated hemoglobin, systolic and diastolic blood pressure play an important role in the occurrence of diabetic retinopathy. Therefore, it is recommended to carefully control blood sugar and blood pressure of diabetic patients in order to prevent the occurrence of retinopathy.
La retinopatía es una de las complicaciones microvasculares más comunes provocadas por la diabetes, que se presenta por cambios en los capilares sanguíneos. Uno de los factores más importantes para determinar la progresión de la retinopatía es medir la HbA1C. Este estudio tuvo como objetivo investigar la relación entre los niveles de hemoglobina glicosilada, la presión arterial (sistólica y diastólica) y los triglicéridos con la PRM en la población de pacientes diabéticos.
MétodosEste estudio descriptivo y analítico se realizó en 80 pacientes diabéticos remitidos a la Clínica de Diabetes Hafiz Sabzevar en 1400. Con base en el examen de fondo de ojo, los pacientes se dividieron en tres categorías generales: pacientes sin retinopatía, pacientes con retinopatía diabética proliferativa y pacientes con retinopatía diabética no proliferativa. retinopatía proliferativa. La información del paciente se recopiló a través de un cuestionario demográfico (que incluía edad, sexo, uso de insulina o drogas orales y nivel de azúcar en sangre en ayunas) y una lista de verificación elaborada por el investigador (que incluía HbA1C, presión arterial sistólica, presión arterial diastólica y triglicéridos). Los datos se analizaron con spss 28. Para el análisis se utilizaron pruebas estadísticas descriptivas, ANOVA y prueba post hoc de Bonferroni.
ResultadosLos resultados del estudio mostraron que existe una diferencia significativa en los niveles de HbA1C, PAS y PAD entre los tres grupos (P = 0,000). Se utilizó la prueba Post Hoc (Bonferroni) para determinar con precisión esta diferencia significativa. Los datos mostraron que ambos grupos con retinopatía (NPDR y PDR) tenían niveles más altos de HbA1C y presión arterial (PAS y PAD) en comparación con el grupo sin retinopatía y esta diferencia fue estadísticamente significativa (P = 0,000). Sin embargo, no hubo diferencia significativa entre los tres grupos en cuanto a los niveles de triglicéridos (P = 0,96).
ConclusiónLos niveles elevados de hemoglobina glicosilada, la presión arterial sistólica y diastólica juegan un papel importante en la aparición de la retinopatía diabética. Por lo tanto, se recomienda controlar cuidadosamente el azúcar en la sangre y la presión arterial de los pacientes diabéticos para prevenir la aparición de retinopatía.
Diabetes is a prevalent metabolic disorder that accounts for a major cause of cardiovascular, hepatic, and stroke diseases1,2. The prevalence of diabetes is estimated to reach 438 million people in the world by 20303. Complications of diabetes include short-term and long-term complications, and the latter include microvascular and macrovascular diseases or cardiovascular complications, which can affect almost every organ of the body. Microvascular complications include nephropathy, retinopathy, and neuropathy, and macrovascular complications include hypertension, ischemia, myocardial infarction, and peripheral and cerebral vascular disease. An increase in the risk of neuropathy and especially retinopathy with the prolongation of diabetes has been shown in various studies4,5.
Retinopathy falls into the most prevalent microvascular complications caused by diabetes, which occurs due to changes in capillaries. These changes lead to the lack of blood perfusion in parts of the retina, and retinal vessels proliferate abnormally in response to blood nonperfusion. Damage to retinal vessels causes liquid and blood leakage inside the retinal tissue (macular edema) or results in the growth of fragile vascular branches and retinal degeneration6, ultimately creating a blurred and unclear image sent by the retina to the brain. This disease is one of the four important causes of blindness in the ages of 20-74 years and a major cause of blindness in diabetic patients in the United States and other parts of the world7.
The most important risk factors for diabetic retinopathy (DRP) include the duration of diabetes, type 1 diabetes, hyperglycemia, hypertension, pregnancy, increased HbA1C, blood lipids, and smoking. Hypertension can induce the release of VEGF by increasing stress on endothelium cells and their elongation, thereby elevating perfusion. The useful effect of blood pressure control on the progression of retinopathy has been reported in some studies8. An increase in serum triglycerides and cholesterol is also associated with a rise in hard exudate in the retina. In a prospective study, a decrease in hard exudate was observed in patients with macular edema and serum lipid disorder after the start of treatment with atorvastatin9. HbA1C measurement is a critical factor to determine the progression of retinopathy, and Wisconsin presented evidence of a direct relationship between the severity of retinopathy and HbA1C levels10. Stockholm observed that maintaining HbA1C levels below 7% could prevent the development and progression of retinopathy11.
The conflicting results of previous studies and the increased prevalence of diabetes followed by DRP necessitate the study of risk factors related to this disease. This study aimed to investigate the relationship between glycosylated hemoglobin levels, blood pressure (systolic and diastolic), and triglycerides with DRP in the population of diabetic patients referred to the Hafiz Diabetes Clinic (HDC) in Sabzevar city.
MethodsThis descriptive-analytical study was conducted on 80 diabetic patients referring to the HDC in Sabzevar city in 2021. The inclusion criteria were patients with type 2 diabetes (FBS > 126 mg/dl) and ophthalmologist examination. Exclusion criteria were patients with type 1 diabetes, known kidney disease, pregnancy, liver disease, and lack of recorded information. Based on the study of Rahimi et al12, the sample size was calculated to be 80 people.
Sampling was done as available from all patients who were evaluated by a retinal disease specialist for the presence and severity of retinopathy. The participants were then divided into three major groups, no retinopathy (NR), non-proliferative retinopathy (NPRP), and proliferative retinopathy (PRP), based on the fundoscopy examination.
Demographic information including age, gender, use of insulin or oral medication, and fasting blood sugar levels, were obtained from the patients. A researcher-made checklist (including glycosylated hemoglobin (HbA1c), systolic blood pressure, diastolic blood pressure, and triglycerides) was completed on the medario website. The information of patients referring to the HDC in Sabzevar, along with the requested routine tests and laboratory data, is recorded on this website. This study was approved by the ethics committee of Sabzevar University of Medical Sciences with the ethics code IR.MEDSAB.REC.1400.006. Full informed consent was obtained from all patients participating in this study. Patients were also assured about the confidentiality of information. Data were analyzed statistically by SPSS 28 using descriptive tests, analysis of variance (ANOVA), and the Bonferroni correction.
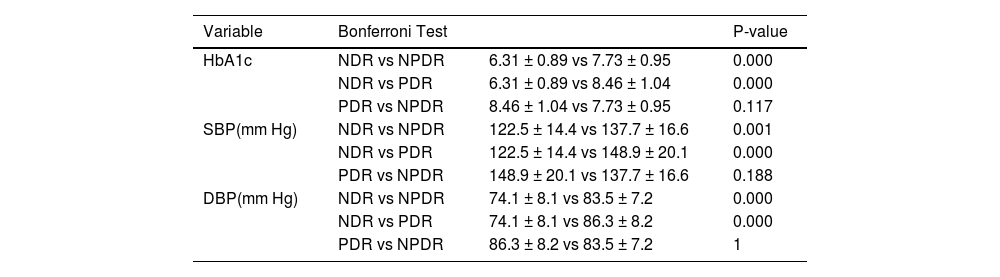
ResultsAll participants (80 people) completed the study. The average age of the participants was 55.89 ± 10.56. The groups did not have statistically significant differences in terms of demographic variables. Individual characteristics of the participants are given by group in Table 1 (Table 1). It is also stated in Table 2 the average paraclinical data between NDR, NPDR and PDR groups (Table 2). The paraclinical parameters were compared between the three groups. Considering the normality of the data (Smirno's Kolmogorov test) and homogeneity of variances (Levin's test), ANNOVA parametric test was used for data analysis. HbA1C and blood pressure (SBP and DBP) variables were significantly different among these three groups. However, there was no significant difference between the three groups in terms of triglyceride levels (Table 3). Post Hoc tests (Bonferroni) were used to determine this significant difference (Table 4). As shown in Table 4, in relation to HbA1C and blood pressure (SBP and DBP) variables, both NPDR and PDR groups have shown a significant difference compared to the NDR group. In other words, the data showed that both retinopathy groups (NPDR and PDR), regardless of whether they are proliferative or not, have higher levels of HbA1C and blood pressure (SBP and DBP) compared to the non-retinopathy group, and this difference was statistically significant.
Comparison of demographic characteristics of participants in each group.
| Variable | Group | NDR | NPDR | PDR |
|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | ||
| Age | 54.84±10.7 | 55.24±11.1 | 57.6±9.9 | |
| Gender | Male | 19 (42.2%) | 13(52%) | 4 (40%) |
| Female | 26 (57.7%) | 12 (48%) | 6 (60%) | |
| Taking insulin or oral antidiabetic medication | 42(93.3%) | 21(84%) | 8(80%) | |
| Fasting blood sugar level | 171.6 ± 32.6 | 186.5 ± 37.2 | 188.5 ± 36.6 |
ANNOVA test to compare paraclinical data between NDR, NPDR and PDR groups.
| ANOVA | ||||||
|---|---|---|---|---|---|---|
| Sum of Squares | df | Mean Square | F | P-value | ||
| HbA1c | Between Groups | 56.166 | 2 | 28.083 | 32.321 | 0.000 |
| Within Groups | 66.902 | 77 | .869 | |||
| Total | 123.068 | 79 | ||||
| SBP | Between Groups | 7514.099 | 2 | 3757.049 | 14.891 | 0.000 |
| Within Groups | 19427.451 | 77 | 252.305 | |||
| Total | 26941.550 | 79 | ||||
| DBP | Between Groups | 2095.847 | 2 | 1047.924 | 17.011 | 0.000 |
| Within Groups | 4743.540 | 77 | 61.604 | |||
| Total | 6839.387 | 79 | ||||
| TG | Between Groups | 139.460 | 2 | 69.730 | .036 | 0.96 |
| Within Groups | 150873.540 | 77 | 1959.397 | |||
| Total | 151013.000 | 79 | ||||
Post hoc tests.
| Variable | Bonferroni Test | P-value | |
|---|---|---|---|
| HbA1c | NDR vs NPDR | 6.31 ± 0.89 vs 7.73 ± 0.95 | 0.000 |
| NDR vs PDR | 6.31 ± 0.89 vs 8.46 ± 1.04 | 0.000 | |
| PDR vs NPDR | 8.46 ± 1.04 vs 7.73 ± 0.95 | 0.117 | |
| SBP(mm Hg) | NDR vs NPDR | 122.5 ± 14.4 vs 137.7 ± 16.6 | 0.001 |
| NDR vs PDR | 122.5 ± 14.4 vs 148.9 ± 20.1 | 0.000 | |
| PDR vs NPDR | 148.9 ± 20.1 vs 137.7 ± 16.6 | 0.188 | |
| DBP(mm Hg) | NDR vs NPDR | 74.1 ± 8.1 vs 83.5 ± 7.2 | 0.000 |
| NDR vs PDR | 74.1 ± 8.1 vs 86.3 ± 8.2 | 0.000 | |
| PDR vs NPDR | 86.3 ± 8.2 vs 83.5 ± 7.2 | 1 | |
The present study was conducted to investigate the relationship between the level of HbA1c and retinopathy in diabetic patients referring to the HDC in Sabzevar. The findings show that the incidence of retinopathy is influenced by a high level of HbA1c, which causes an increase in the incidence of both PRP and NPRP. Our results also indicate that the elevated incidence of PRP and NPRP in both groups is affected by high systolic and diastolic blood pressures. However, triglyceride levels were not different in patients with and without retinopathy.
The development of DRP is strongly associated with a longer duration of diabetes, increased blood sugar, and hypertension13,14. A higher level of HbA1c is significantly associated with the progression of DRP, and strict blood glucose control reduces the incidence and severity of retinopathy15. Recent studies suggest a strong association between glycemic variability and DRP in type 2 diabetes13. In addition, clear evidence is available on the relationship between hypertension and DRP. The strict control of blood pressure reduces the deterioration of retinopathy16.
Chronic hyperglycemia, blood lipids, and hypertension have frequently been shown to be involved in the pathogenesis of DRP. The precise mechanisms by which a disorder is caused by elevated glucose are poorly defined, and the involvement of multiple pathways is not surprising17. Evidence indicates that inflammation is a cause of DRP. Leukocytes cause vascular blockage through some mechanisms, and this blockage results in angiogenesis due to ischemia mediated by angiogenesis factors, such as the vascular endothelial growth factor17.
Studies suggest that the prevention of DRP is one of the best and most useful treatments for this complication, hence the control of metabolic abnormalities of diabetes has a major effect on the development of this complication18. This complication can be prevented by various methods, one of which is the optimum metabolic control of blood sugar16. Sugar control in the normal range prevents inflammation, thereby preventing retinal ischemia and DRP17. In line with previous studies, our study has shown that precise sugar control prevents retinal ischemia and DRP.
Another method to prevent DRP is to control blood pressure within the normal range. Normal blood pressure is an important factor to prevent the occurrence of DRP19. Similar to other studies, our study also indicates a relationship between blood pressure and retinopathy. Unlike other studies, our study shows the relationship between blood pressure and PRP and NPRP, indicating that this factor was more in PRP patients than in NPRP ones.
Another treatment method is to reduce blood lipids, which play an important role in creating microaneurysms in the retina in addition to increasing the chance of atherosclerosis, retinal vessel stenosis, and retinal ischemia, resulting in retinal retinopathy20. Our study demonstrates the relationship between triglycerides and PRP and NPRP, showing that this factor was more in PRP patients than in NPRP ones, but it was not statistically significant. This probably indicates the need for more sample size or the passage of more time for the incidence of retinopathy.
As explained above, maintaining blood pressure, blood sugar, and blood lipids are the three main methods to prevent the incidence of DRP. Besides the prevention of DRP development, maintaining these three factors in the normal range can also help reduce the incidence rate of this complication, thereby increasing patients' years of life without blindness. The normal blood sugar level is examined using the Hb1AC factor, which has been shown to be one of the best factors for measuring blood sugar levels. This factor is used to monitor long-term blood sugar control, treatment regulation, quality assessment of diabetes care, and risk prediction of complications21.
The limitations of our research include the limited number of subjects and laboratory errors. As a general conclusion, it can be stated that the normal level of Hb1AC plays a role in preventing any type of retinopathy. Therefore, proper control of blood sugar in diabetic patients to maintain the normal range of Hb1AC can play a key role in preventing the incidence of retinopathy
AppreciationThis study is the result of a thesis approved by Sabzevar University of Medical Sciences. We would like to express our gratitude to the Deputy of Research and Technology of Sabzevar University of Medical Sciences, the director and staff of Hafeez Diabetes Clinic and all the patients who participated in this study. The present study was carried out with the financial support of the Research and Technology Vice-Chancellor of Sabzevar University of Medical Sciences.