Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosTo depict the picture of sleep disorders of head and neck cancer radiotherapy patients.
MethodThis research was a descriptive study, using total sampling in head and neck cancer radiotherapy patients in April 2019 at Hasanuddin University Hospital as many as 16 samples using PSQI questionnaire, Snoring score, Epworth Sleepness Scale, and Insomnia Severity Index.
Result14 people experienced sleep disorders of 16 patients. They are at risk for suffering from obstructive sleep apnea, and two people are easily sleepy, nine people have insomnia.
ConclusionHead and neck cancer radiotherapy patients suffer more insomnia sleep disorders and have a risk of suffering from obstructive sleep apnea (OSA).
Head and neck cancer is defined as all cancers arising from the upper aerodigestive tract, such as the sinonasal ducts, oral cavity, pharynx, and larynx, usually histopathologically in the form of squamous cell carcinoma. Globally, this cancer ranks ninth in cancer mortality rates. It is estimated that there were 550,319 cases of head and neck cancer and caused 305,096 deaths in 2008.1
Treatment for head and neck cancer patients includes surgery, radiation, and chemotherapy. All of these treatment methods can cause structural changes and cause chronic pain among sufferers of head and neck cancer. Akman et al. have proven this condition and obtained data that the patient's resting needs are disrupted, and his sleep quality is declared inadequate.2
With the increasing number of people with head and neck cancer (HNC) over the past few decades, the focus in this population has shifted from survival to a better quality of life. The incidence of OSAHS in patients with HNC ranges from 8 to 95%. However, little is known about the effects of HNC therapy on sleep disorders and vice versa. The implication is that the management of obstructive sleep apnea–hypopnea syndrome (OSAHS) has an essential role in improving the quality of life of head and neck cancer patients.3
Quality sleep is needed by cancer patients who are undergoing treatment in the hospital to regenerate and repair body cells. NREM sleep stimulates the production of growth hormone (Growth Hormone), which will help in repairing body tissues. According to Buyse and Taylor, REM sleep is needed to maintain brain tissue and is vital for cognitive recovery. Quality sleep serves to help optimize the healing of diseases for cancer patients.
Changes due to radiation can be acute and advanced. Acute changes include mucositis, decreased taste acuity, decreased moderate salivary production in the form of mucosal and skin atrophy, loss of soy sauce, connective tissue necrosis, osteonecrosis.4
The review article by Soussain et al. summarizes several types of central nervous system complications due to radiotherapy, including acute encephalopathy which affects up to 50% of patients after high doses or radiation fractions, and drowsiness syndrome which is mainly seen in pediatric patients, but can also affect adult patients in the first two months after radiotherapy. Prominent symptoms are sleepiness and excessive sleep, nausea, and anorexia; focal cerebral and spinal cord radionecrosis are complications due to severe radiation and are neuropathologically defined as necrosis with severe vascular lesions (stenosis, thrombosis, bleeding, fibrinoid vascular necrosis).5
It can be assumed that radiation therapy to the nasopharynx and neck can cause changes in airway stability and the function of the muscles of the upper airway dilator, which in turn affects the resistance of the upper airway.3 Therefore, head and neck cancer patients are suitable candidates to evaluate the effects of radiotherapy on sleep disorders. To our knowledge, there are no studies that specifically address the effects of radiotherapy in the head and neck region for sleep disorders in this group of patients.
MethodThis research was a descriptive study that looks at the picture of sleep disorders of head and neck cancer patients undergoing radiotherapy. This study was conducted in April 2019 in all head and neck cancer patients undergoing radiotherapy. The place of research was the radiotherapy section at Hasanuddin University Hospital. The study population was all head and neck cancer sufferers who underwent radiotherapy at Hasanuddin University Hospital. The research sample was determined by total sampling, which is a sampling technique where the number of samples is equal to the population.
The inclusion criteria used were as follows: adult patients aged 18–65 years old both male and female, patients suffering from head and neck cancer as evidenced by histopathological examination and imaging, underwent radiotherapy at Hasanuddin University Hospital in April 2019, and willing to be included in this study by signing informed consent. The exclusion criteria used were as follows: patients undergoing treatment modalities other than radiotherapy while undergoing radiotherapy, patients who have sleep disorders before being diagnosed with cancer, and decreased awareness (GCS<15).
Data collection began when head and neck cancer patients underwent radiotherapy at the Hasanuddin University Hospital. Patients were asked to fill out a PSQI questionnaire, Snoring score, Epworth Sleepness Scale, and Insomnia Severity Index. Data is then collected and processed.
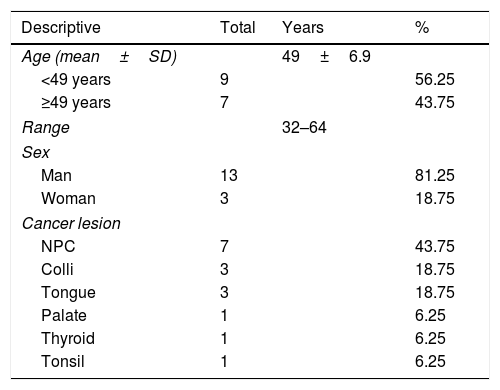
ResultThe study was conducted in April 2019 in the radiotherapy section of Hasanuddin University Hospital in 16 samples. This study uses a descriptive design to look at sleep disorders in head and neck cancer patients using the Pittsburgh Sleep Quality Index (PSQI) questionnaire, Snoring score, Epworth sleepiness scale, and Insomnia Severity Index (ISI). Patient subject characteristics include age, sex, and location of cancerous lesions.
From Table 1, it is found that the minimum age of head and neck sufferers undergoing radiotherapy is 32, and the maximum age is 64. There are 13 male patients (81.25%) and three women (18.75%). Head and neck cancer is dominated by nasopharyngeal carcinoma in 7 cases (43.75%).
Characteristics of the study sample based on age, sex, and location of cancer lesions (N=16).
| Descriptive | Total | Years | % |
|---|---|---|---|
| Age (mean±SD) | 49±6.9 | ||
| <49 years | 9 | 56.25 | |
| ≥49 years | 7 | 43.75 | |
| Range | 32–64 | ||
| Sex | |||
| Man | 13 | 81.25 | |
| Woman | 3 | 18.75 | |
| Cancer lesion | |||
| NPC | 7 | 43.75 | |
| Colli | 3 | 18.75 | |
| Tongue | 3 | 18.75 | |
| Palate | 1 | 6.25 | |
| Thyroid | 1 | 6.25 | |
| Tonsil | 1 | 6.25 | |
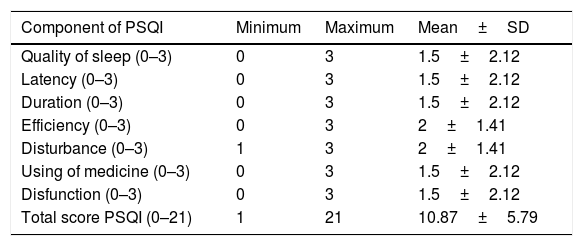
From Table 2, the minimum PSQI sub-score is 0 except for the sleep disturbance component, and the minimum value is 1. The maximum value of the PSQI sub-score is 3. The mean value of each component ranges from 1.5 to 2. The minimum total PSQI value is one and the maximum 21, with a mean value of 10.87.
Subscore PSQI and total score PSQI.
| Component of PSQI | Minimum | Maximum | Mean±SD |
|---|---|---|---|
| Quality of sleep (0–3) | 0 | 3 | 1.5±2.12 |
| Latency (0–3) | 0 | 3 | 1.5±2.12 |
| Duration (0–3) | 0 | 3 | 1.5±2.12 |
| Efficiency (0–3) | 0 | 3 | 2±1.41 |
| Disturbance (0–3) | 1 | 3 | 2±1.41 |
| Using of medicine (0–3) | 0 | 3 | 1.5±2.12 |
| Disfunction (0–3) | 0 | 3 | 1.5±2.12 |
| Total score PSQI (0–21) | 1 | 21 | 10.87±5.79 |
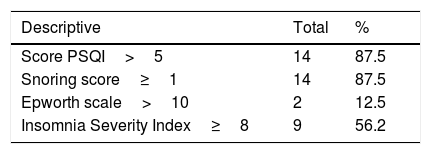
From Table 3, it was found that from the PSQI measurements, there were 14 people who experienced sleep disorders. From the Snoring score measurement, 14 people are at risk for suffering from obstructive sleep apnea. With the Epworth Scale measurement, there are two people who are easily sleepy. Furthermore, by measuring the Insomnia Severity Index, nine people suffered from insomnia with the details of 8 people included in the category of subthreshold insomnia and one person in the moderate insomnia category.
Result of the score (N=16).
| Descriptive | Total | % |
|---|---|---|
| Score PSQI>5 | 14 | 87.5 |
| Snoring score≥1 | 14 | 87.5 |
| Epworth scale>10 | 2 | 12.5 |
| Insomnia Severity Index≥8 | 9 | 56.2 |
Rating: PSQI>5 disturbance of sleep, snoring: ≥1 high-risk obstructive sleep apnea, epworth: abnormal>10, ISI: total score: 0–7 no clinically significant insomnia, 8–14 subthreshold insomnia, 15–21 clinical insomnia (moderate insomnia), 22–28 clinical insomnia (severe insomnia).
Sleep disturbance can be proven by using the PSQI questionnaire. While the measurement of the gold standard of sleep monitoring is a polysomnographic tool. However, the use of polysomnography is still limited because it is expensive and requires the space and time and energy needed. Questions about sleep aids.
Sleep disturbance can occur due to reduced quality, the quantity of sleep, or disruption of circadian rhythms. This study using assessment of sleep disorders, i.e., Pittsburgh Sleep Quality Index (PSQI), to measure the quality and sleep patterns of adults and snoring scores.6 An instrument for assessing snoring or risk of obstructive sleep apnea and dysfunction due to snoring is the Epworth sleepiness scale, to measure the tendency to sleep every day, Insomnia Severity Index (ISI), and to assess the severity of insomnia and its effects.
According to the International Classification of Sleep Disorders (ICSD), III insomnia is a subjective perception of insomnia, duration, consolidation, or quality of sleep, even though the patient is given the opportunity for adequate time to sleep. Insomnia is divided into; chronic insomnia disorder, short-term insomnia disorder, and other insomnia disorders.6
Insomnia suffered by cancer patients undergoing radiotherapy is generally short term (less than three months). The precipitating factors are discomfort due to the effects of radiotherapy and the tendency to urinate at night. All patients undergoing radiotherapy are advised to drink plenty of water. Over time, patients will begin to adapt. Sleep disturbance will improve.
Hypersomnia is a symptom that arises at any time from a tendency to get sleepy or to fall asleep at an intensity and expectation to stay awake and awake. Based on ICSD-2, hypersomnia is divided into several types based on its etiology; namely, central hypersomnia, hypersomnia due to breathing disorders, circadian rhythm disorders, and other causes that cause sleep disorders. Sleep fragmentation and lack of sleep will cause a high urge to sleep. It causes drowsiness, especially during the day. But in this study, patients who underwent radiotherapy still did not feel drowsiness even though sleep time was reduced at night. This is caused by discomfort and pain that lasts during radiotherapy treatment.
Obstructive sleep apnea (OSA) is a sleep disorder characterized by a partial or partial obstruction of the airways that causes apnea or hypopnea during sleep. It will be followed by oxygen desaturase and usually ends with short arousal. Symptoms include snoring, stopping breathing during sleep, suffocating or choking, not refreshing sleep, excessive sleepiness throughout the day, nocturia, morning headaches, insomnia, impaired concentration, and memory. Head and neck cancer patients have the possibility of suffering from OSA. In this study, 14 patients or almost all patients had a high risk of suffering from OSA. It needs to be studied further because some of the effects of radiotherapy have in common with OSA symptoms. Besides, the pathophysiology of OSA in head and neck cancer is based on the ability to maintain the airway during sleep. The main factor in the collapse of the upper airway during radiotherapy is xerostomia. The effect of the matrix on the upper airway, the superior pharyngeal constrictor muscle can pull the back tongue and reduce the distance between the base and the back of the pharyngeal wall. Impaired muscular control, impaired function of the pharyngeal dilator muscle, and effects on the tissue around the respiratory center are additional factors. Sinusitis radiation by hardening of the skin that causes nasal obstruction can increase the likelihood of pharyngeal airway obstructions by the mechanism previously described.
ConclusionHead and neck cancer radiotherapy patients suffer more sleep disorders in the form of insomnia and have a high risk of suffering from obstructive sleep apnea (OSA).
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.