This case report describes the surgical procedures performed for treatment of single gingival recession in the anterior area.
CaseA 20-year-old female patient came with a chief complaint of the tooth looks longer than before. Intraoral examination showed gingival recession # 31. Initial therapy includes scaling and root planning was performed before the surgical procedure. Coronally repositioned flap then vestibulectomy was performed. One week follow-up showed completely recession coverage and one-month follow-up showed that treatment still maintains recession coverage.
ConclusionCoronally repositioned flap combined with vestibulectomy showed a successful treatment in correcting the gingival recession for complete healing and esthetic outcome.
Gingival recession is defined as the exposure of the root surface due to the movement of the gingival margin in the apical direction. This is a broad clinical manifestation and may involve single or multiple tooth surfaces. The main cause of gingival recession is the wrong way to brush your teeth; however, other predisposing factors include dental plaque, high frenum pull, root protrusion area, thin narrow band of the gingiva, iatrogenic factors, and gingival recession after surgery. Root hypersensitivity, esthetic problems, and abrasion can accompany gingival recession and can interfere with overall health problems.1–3
The most commonly used clinical classification of gingival recession is the Miller (1985) classification. Miller classified gingival recession into 4 classes based on the relationship with mucogingival line and interproximal bone. The classification will be explained as follows4,5:
- 1.
Class I: gingival margin recession does not pass through the mucogingival junction and there is no loss of interproximal bone. Surgical therapy for this defect can cover all exposed roots.
- 2.
Class II: recession defects pass mucogingival junction without loss of interproximal bone. As with Miller's Class I, surgical therapy for this type of defect can cover all exposed roots.
- 3.
Class III: recession defects have reached or even passed the mucogingival junction. Soft tissue and apical interdental bone from the cementoenamel junction but more coronal than the basis of recession. With surgical therapy, only a portion of root closure can be achieved.
- 4.
Class IV: margin recession passes through the mucogingival junction with loss of soft tissue and bone located more apically than the basis of recession. Root coverage with surgical therapy is not possible.
Many surgical techniques, such as laterally positioned flaps, coronally repositioned flaps, free gingival grafts, have been proposed to achieve root coverage from exposed root surfaces. Among these techniques, the coronally repositioned flap (CRF) procedure is the most commonly used technique for root coverage, which is based on the coronal movement of soft tissue on the exposed root surface.2,6
Miller's Class I gingival recession does not pass through the mucogingival junction and there are a number of keratinized gingiva at the apical root exposed. To treat Miller class I recession defects, it has been reported that CRF is used as an effective technique and provides good clinical results.2 In this case report, a case with Miller's Class I gingival recession was treated using a coronally repositioned flap accompanied by vestibulectomy. This case report aims to explain surgical treatment for a single gingival recession in the anterior teeth so that the patient's esthetic needs are achieved.
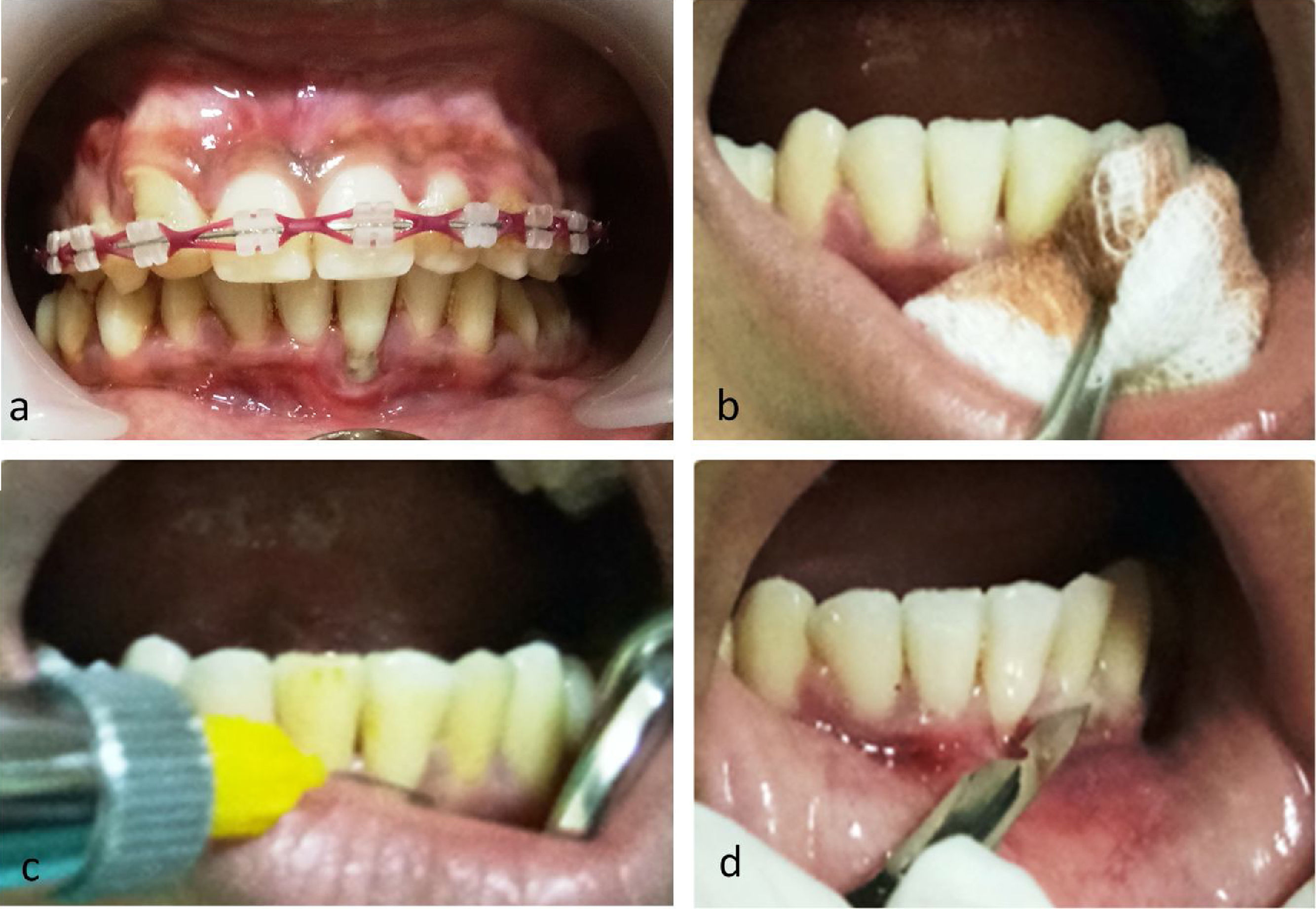
Case reportA female patient aged 20 years came to Hasanuddin University Dental Hospital, in the Department of Periodontology, with complaints of teeth appearing to be longer than before. An intra-oral examination revealed gingival recession of 3mm in the category Miller's Class I and the use of ortho fixed in the maxillary dentition (Fig. 1a). In this case, correction of the gingival recession was performed using a coronally repositioned flap accompanied by vestibulectomy.
In such cases, the choice of a coronally repositioned flap (CRF) aims to obtain optimal root coverage. Because the CRF usually shortens the vestibulum, a vestibulectomy is performed so that esthetic root coverage can be obtained. Initial therapy is done by scaling and root planning and patients are given dental health education.
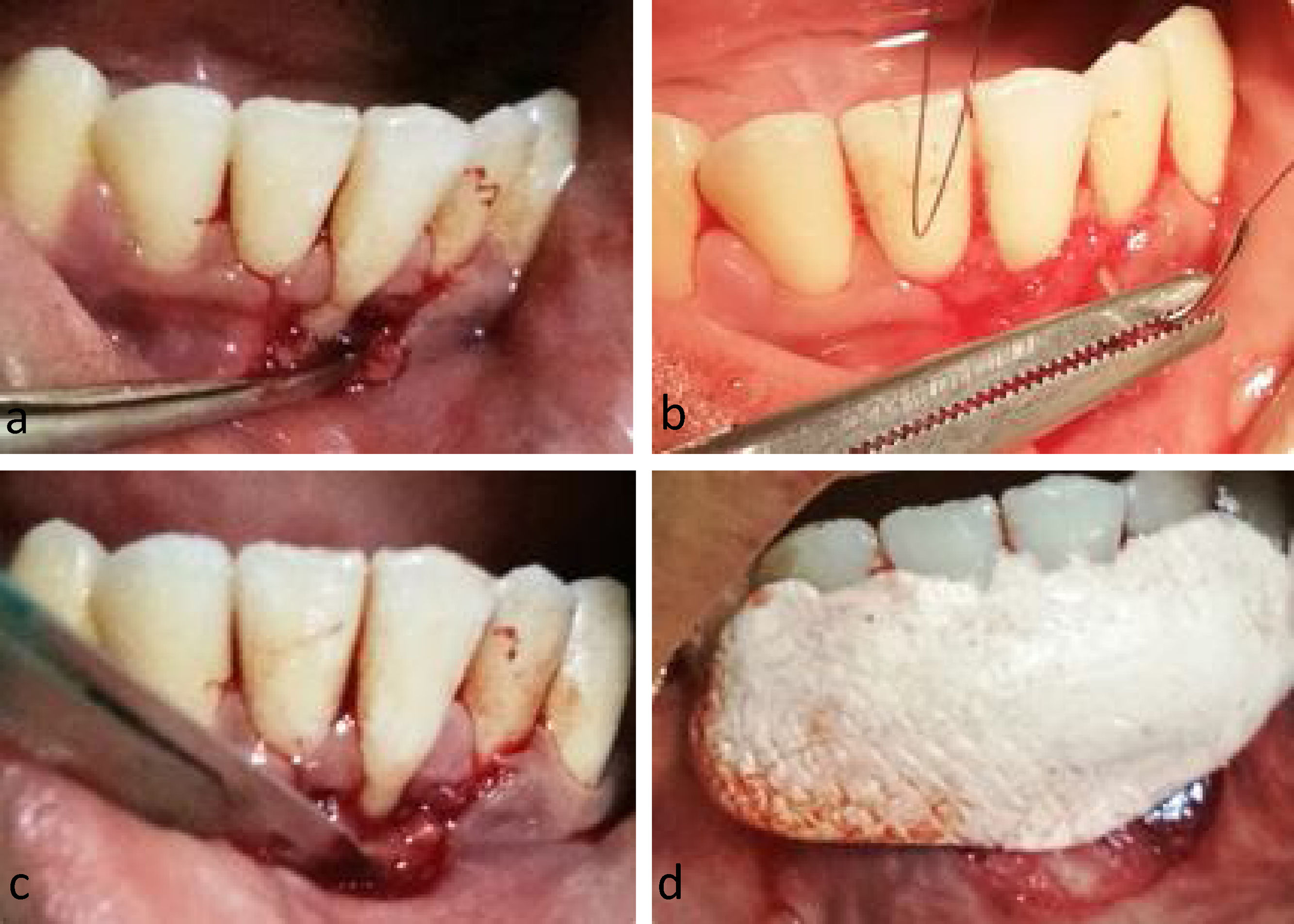
The surgical procedure begins with disinfection of the operating area with betadine solution (Fig. 1b), then local anesthesia is carried out with infiltration in region #32–41 (Fig. 1c). Papilla preservation incisions were made from mesial #32 to mesial #41 using scalpel no.15. Then a vertical incision was made to limit the area of operation (Fig. 1d). Next, a full-thickness flap is opened by using the periosteal elevator until the mucobuccal fold (Fig. 2a). The operating area is irrigated with saline solution. Then the flap is positioned coronally and sutured with the sling suture (Fig. 2b). The vestibulectomy was then carried out to increase the width of the attached gingiva (Fig. 2c). Irrigated again with saline solution. Cover the tissue in the area under surgery using periodontal dressing (Fig. 2d).
DiscussionAccording to Pini-Prato et al. (1997), mucogingival therapy can completely cover root surfaces in Miller's Class I and II defects, in part on Miller's Class III defects (70–75%), and do not produce coverage at all in Miller's Class IV defects. Shortly after surgery, root coverage increases to 80% due to creeping attachments.4
Gingival recession can occur in single or multiple teeth from the causative factor. Recession can be caused by physiological or pathological factors. Physiological recession-related with age, while recession is pathologically categorized in pathological anatomy, mechanical, and infectious. Anatomical pathology includes tooth malposition, prominent root shape, or thin alveolar bone covering the root. Mechanical pathology is caused by the false technique of brushing teeth, brushing teeth with great force or because of bad habits such as the use of improper toothpicks. Pathological infections, for example in periodontal disease.5
Treatment planning for a gingival recession is based on the etiology and severity of the recession. Before treatment of the gingival recession, the etiological factors of the recession must be treated first. Gingival recession management can be done surgically or non-surgical. Handling a recession with a surgical procedure in addition to aiming to cover the recession area also serves to reduce hypersensitivity, prevent a more severe recession and for esthetic correction especially recession in the anterior area. Surgical treatment success is related to the selection of surgical techniques, procedures during surgery, suturing techniques, and postoperative care.5
ConclusionThe results of this case report show that the technique of coronally repositioned flap with vestibulectomy can be an effective treatment for a single gingival recession in the anterior teeth and can obtain the esthetic needs of patients.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the International Conference on Women and Societal Perspective on Quality of Life (WOSQUAL-2019). Full-text and the content of it is under responsibility of authors of the article.