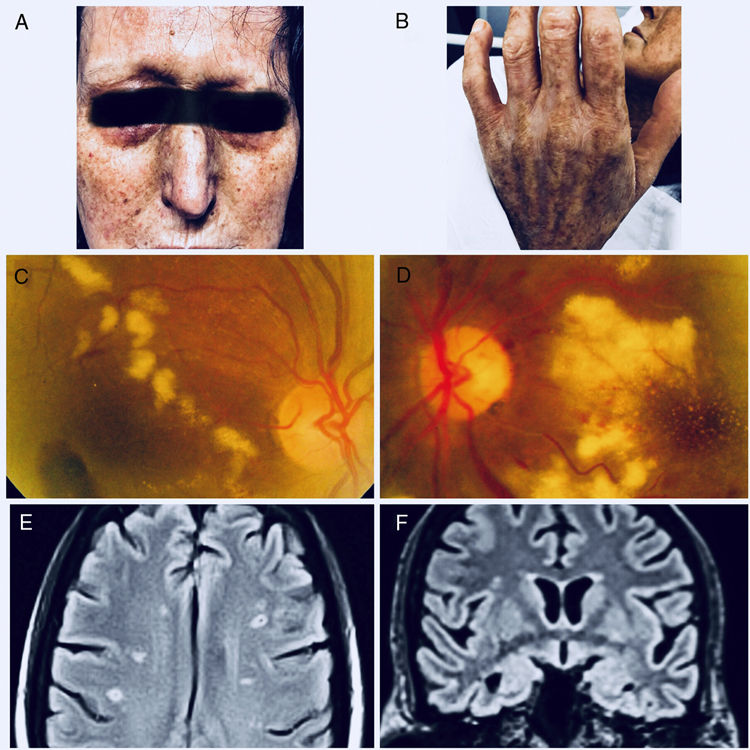
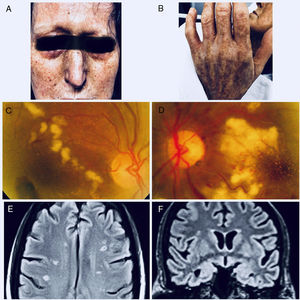
A 55-year-old woman with a 3-year history of sclerodermiform syndrome undergoing treatment with systemic corticosteroids who presented with a week of low-grade fever, confusional syndrome and visual hallucinations. On physical examination there are white papular lesions that converge forming raised lichenoid zones and between these other hyperpigmented with facial, trunk and limb involvement There was sclerodactyly, microstomy and alopecia in eyebrows (‘Leonine-like’ face) (Fig. 1A and B). The neurological examination showed temporary disorientation, limitation to supraversion and dysarthria. Ophthalmological examination revealed sclerotic and tortuous vessels with whitish lesions, reminiscent of Purtscher's fleckens and hemorrhages affecting the posterior pole (Fig. 1C and D). MRI revealed multiple points of hyperintensity in both hemispheres compatible with lacunar infarcts (Fig. 1E and F). The laboratory tests revealed a globular sedimentation rate of 8.5mm/h and creatinine levels of 5mg/dL, without finding signs of hemolysis, with normal levels of enzyme ADAMTS13, which ruled out microangiopathy of the type thrombocytopenic purpura. The proteinogram presented a monoclonal peak of 9g/L of immunoglobulin G-Kappa. The skin biopsy showed myxoid dermal material with fibroblastic proliferation, while that of bone marrow and the absence of Bence-Jones chains in urine rule out the presence of multiple myeloma. A diagnosis of scleromyxedema with systemic involvement due to microangiopathic thrombotic crisis is reached, and despite the poor prognosis, treatment with plasmapheresis and eculizumab 900mg/week is started, obtaining a two-week improvement in the neurological status and renal disease, which is why the hospital discharge for ambulatory control.
SJR es una prestigiosa métrica basada en la idea de que todas las citaciones no son iguales. SJR usa un algoritmo similar al page rank de Google; es una medida cuantitativa y cualitativa al impacto de una publicación.
Ver másSNIP permite comparar el impacto de revistas de diferentes campos temáticos, corrigiendo las diferencias en la probabilidad de ser citado que existe entre revistas de distintas materias.
Ver másLa tasa de aceptación de las revistas se calcula dividiendo el número total de artículos aceptados (inicialmente y después de la revisión estándar) por el número total de envíos (aceptados y rechazados).
Ver más