Gastric outlet obstruction (GOO) is a clinical syndrome characterized by abdominal pain and post-prandial vomiting due to a mechanical obstruction of the outlet of the stomach. Bezoars, concretions of undigested or partially digested material in the gastrointestinal tract, are a rare entity and GOO due to bezoar is an infrequent presentation.
Case descriptionWe present the case of a 48-year-old female, attending the emergency room for abdominal pain and distension, nausea, vomiting and clinical signs of intestinal obstruction. Imaging studies showed an asymmetric thickening of the gastric antrum with dilation of the stomach at the expense of intraluminal mass. An oesophageal gastroduodenoscopy revealed the presence of non-suctionableable solid food content, antral mucosa thickened with necrotic ulcer of nodular aspect and a pyloric stenosis. The histopathological study showed a poorly differentiated adenocarcinoma in the muscle wall.
ConclusionsThe development of a bezoar as a complication of duodenal carcinoma is a very rare entity. In the case discussed above, the main factor that is seen clinically and chronologically related to the development of our patient's bezoar is reduced antral motility and a partial obstruction of the outlet as a consequence of neoplastic involvement of the duodenum. Many patients remain asymptomatic for many years and develop symptomatology in an insidious manner, with vague symptoms including abdominal pain, nausea, vomiting, early satiety, anorexia, and weight loss. A detailed evaluation is necessary in order to exclude underlying disease, including malignancy, in patients who develop gastric bezoars.
La obstrucción gástrica (OG) es un síndrome clínico caracterizado por dolor abdominal y vómito posprandial debido a obstrucción mecánica de la porción distal del estómago. Los bezoares, acúmulos de material pobre o parcialmente digerido del tracto gastrointestinal son una entidad rara, y la OG secundaria a bezoar es una presentación infrecuente.
Descripción del casoPresentamos el caso de un paciente femenino de 48 años que acudió al servicio de urgencia por dolor abdominal y signos clínicos de obstrucción intestinal. Estudios de imagen demostraron engrosamiento asimétrico del antro gástrico con dilatación de la cámara gástrica a expensas de una masa intraluminal. La esofagogastroduodenoscopia demostró la presencia de material alimentario sólido no aspirable, con engrosamiento de la mucosa antral asociado a úlcera necrótica de aspecto nodular con estenosis de píloro. El estudio histopatológico de esta lesión demostró un adenocarcinoma pobremente diferenciado.
ConclusionesEl desarrollo de un bezoar como resultado de un carcinoma duodenal es una entidad muy infrecuente. En el caso expuesto, el principal factor asociado clínica y cronológicamente al desarrollo del bezoar fue la motilidad antral reducida y la obstrucción parcial que imposibilitó el vaciamiento gástrico secundario al involucro neoplásico de la unión gastroduodenal. La mayoría de los pacientes permanecen asintomáticos durante mucho tiempo y desarrollan síntomas de forma insidiosa, con síntomas inespecíficos como dolor abdominal, náusea, vómito, saciedad temprana, anorexia y pérdida de peso. Es necesario una búsqueda exhaustiva para determinar la enfermedad subyacente, incluyendo malignidad, en adultos con bezoar gástrico.
Small Intestine obstruction (SIO) is a common clinical disorder caused by multiple conditions. Common causes include postoperative adhesions (60%-80%) volvuli, intussusception, hernias, and tumors. The obstruction of the small intestine by a bezoar (SIO-B) is a rare entity, accounting for approximately 4% of SIO cases.1 A bezoar is a foreign body composed of undigested material trapped in the gastrointestinal tract, most commonly found as a hard mass or concretion in the stomach. It may consist of elements ingested whether deliberately or accidentally. The predisposing factors include a history of gastric surgery such as partial gastrectomy, vagotomy, and pyloroplasty, as well as peptic ulcer disease, chronic gastritis, and elderly or diabetic individuals with gastric motility disorders; also, Crohn's disease, dehydration, hypothyroidism, and gastrointestinal tract carcinoma. These conditions lead to a reduction of gastric acidity, gastric stasis, loss of function and/or pyloric stenosis.2
The development of an intestinal bezoar may be an indication of sufficient neoplastic growth to obstruct the gastric outlet or may cause hypomotility as a consequence of the neoplastic involvement of the gastric antrum.3 Most patients remain asymptomatic for many years and develop symptoms in an insidious way. Symptoms include abdominal pain, nausea, vomiting, early satiety, anorexia, and weight loss .4 We present a rare case of SIO caused by a bezoar as the first manifestation of a duodenal adenocarcinoma.
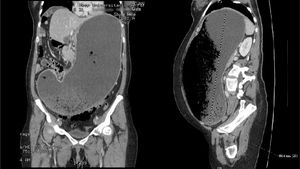
Clinical caseA 48-year-old female was admitted to the Internal Medicine Department for a colic-type abdominal pain of 6 months of evolution, as well as an increased abdominal perimeter, nausea, post-prandial vomiting of gastrointestinal content, constipation, and weight loss of 5kg in the previous three months. On physical examination, she presented significant abdominal distension, diffuse abdominal pain, and signs of dehydration. A CT scan of the abdomen showed asymmetric thickening of the gastric antrum and dilation of the stomach up to the greater pelvis at the expense of an intraluminal mass with mottled pattern conformed by gastric contents and gas which displaced the intestinal loops to the right hemiabdomen (Figure 1).
CT scan of the abdomen that revealed asymmetric thickening of the gastric antrum, dilation of the stomach up to the greater pelvis at the expense of intraluminal mass with a mottled pattern composed by the presence of gastric material and gas, as well as displacement of the intestinal loops to the right hemiabdomen.
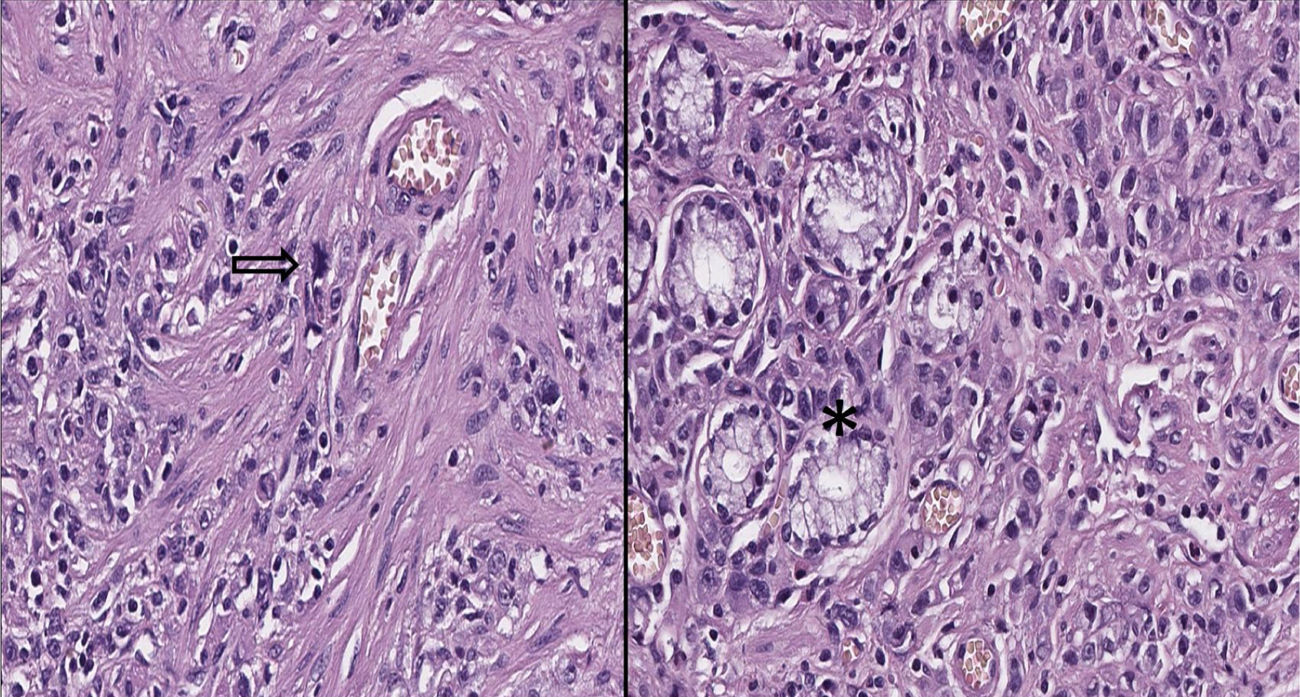
Esophagogastroduodenoscopy revealed the presence of a large non-aspirable bezoar that occluded the distal gastric lumen, we also found thickened antral mucosa with necrotic ulcer of nodular aspect and moderate pyloric stenosis. Biopsies of the antrum were performed and the histopathological study showed severe chronic gastritis due to the presence of Helicobacter pylori; and a poorly differentiated adenocarcinoma in muscle wall associated with necrotic ulcer (Figure 2).
Left image: In the lower-left area is observed the presence of malignant epithelial cells that infiltrate through the smooth muscle bundles, intermingled with chronic inflammatory cells; in the center of the image there is mitosis (Arrow, original magnification to 40X). Right image: There are residual glands which are displayed on the left side of the image (asterisk).
Due to unresectable disease, a gastrojejunal anastomosis in omega was performed. After a 5-day observation with good clinical evolution, the patient was discharged to continue ambulatory treatment.
DiscussionMalignant neoplasms of the small bowel are considered of low prevalence. The most frequent location is in the duodenum and its diagnostic complexity leads to therapeutic delay and worse prognosis.5
The primary adenocarcinoma of the small intestine is a rare neoplasm and is the most common histological subtype of the site, accounting for 40% of cases. Carcinoid tumors are the second most common type, accounting for 36% of cases. The male gender has a higher incidence compared to females.6 The etiology of most cancers of the small bowel is unknown, although a number of risk factors and predisposing factors have been described such as familial adenomatous polyposis, celiac disease, cystic fibrosis, hereditary non-polyposis colorectal cancer (HNPCC), Peutz-Jeghers syndrome, Crohn's disease, and peptic ulcer disease. Chow et al suggested that red meat and foods smoked and cured in salt were possible dietary risk factors .7 Negri et al, on the other hand, found a direct relationship with bread, pasta, rice and sugar and an inverse relationship with the consumption of coffee, fruits, and vegetables.8
In a single-center study of 217 individuals, approximately 66% of patients with tumors of the small bowel had abdominal pain at diagnosis. Other findings were intestinal occlusion (40%) and bleeding (24%) .9 According to the statistics, the appearance of tumors in the 3rd and 4th portions of the duodenum is 45%; 40% in the second portion, and only 15% in the first portion of the duodenum.10
Regarding treatment, chemotherapy and radiation have shown disappointing results. A surgical intervention provides a curative resection in 40-65% of patients, with 5-year survival rates of 40-60% for resected tumors compared to 15-30% for unresectable tumors.11
The development of a bezoar as a complication of duodenal carcinoma is very rare. In the case discussed above, the main factor that is seen clinically and chronologically related to the development of our patient's bezoar is a reduced antral motility and a partial obstruction of the outflow as a consequence of the neoplastic involvement of the duodenum. Many patients remain asymptomatic for many years and develop symptomatology in an insidious manner, with vague symptoms including abdominal pain, nausea, vomiting, early satiety, anorexia, and weight loss. Therefore, a detailed evaluation is necessary in order to exclude underlying disease, including malignancy, in patients who develop gastric bezoars.
Conflict of interest disclosureThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare that there is no conflict of interest regarding the publication of this paper.