Stress hyperglycemia has been associated with a worse prognosis in patients hospitalized in critical care units. The aim of this study is to evaluate the impact of blood glucose and glycosylated hemoglobin (HbA1c) levels on the mortality of patients suffering a acute cerebro-vascular event, and to determine if this relationship depends on the presence of diabetes.
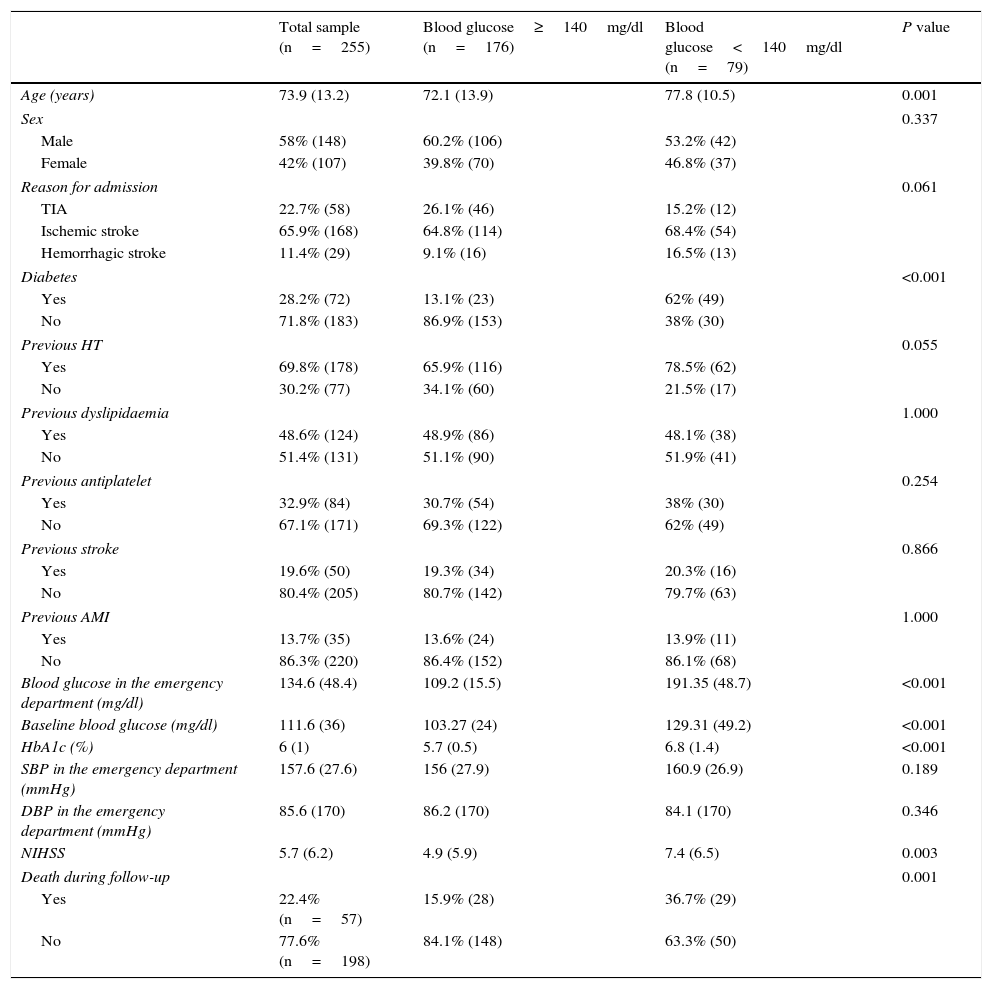
Material and methodsA retrospective analysis of 255 patients admitted to the ER for stroke was performed. Venous plasma glucose levels in the emergency room and HbA1c levels within the first 48h were analyzed.
The presence of diabetes was defined in terms of the patients’ medical history, as well as their levels of fasting plasma glucose and HbA1c.
Mortality was assessed within the first 30 months after the onset of the acute event.
Results28.2% of patients had diabetes.
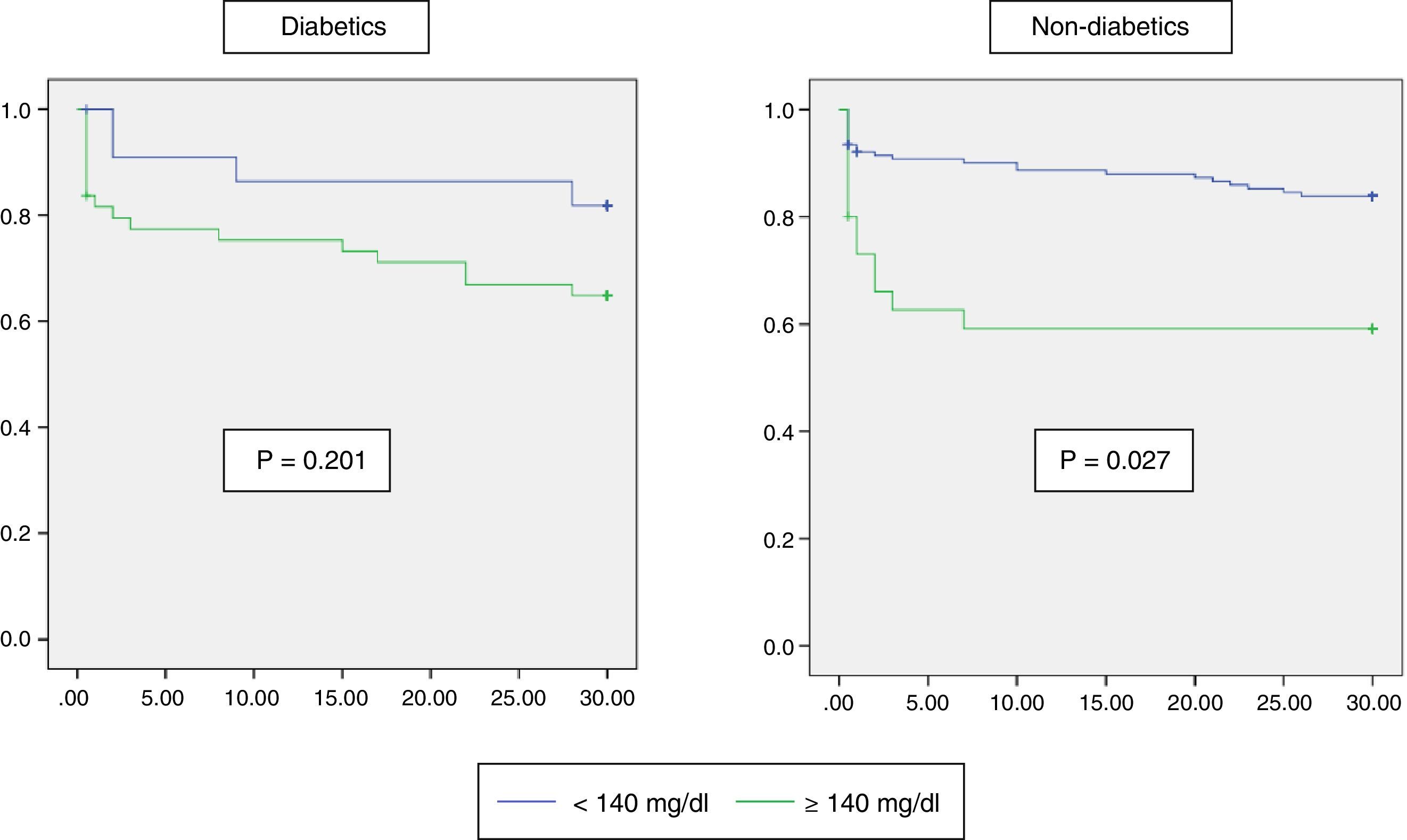
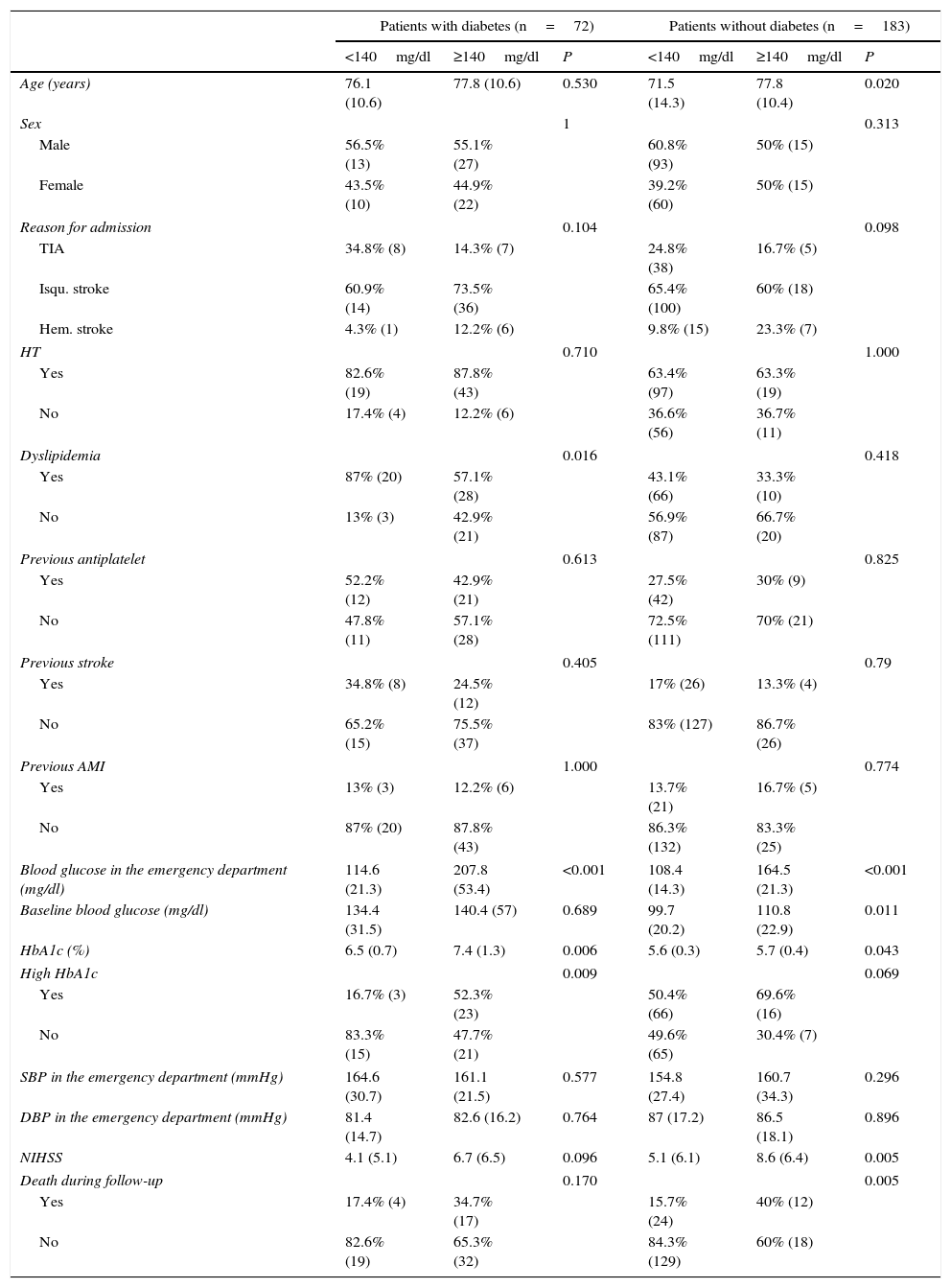
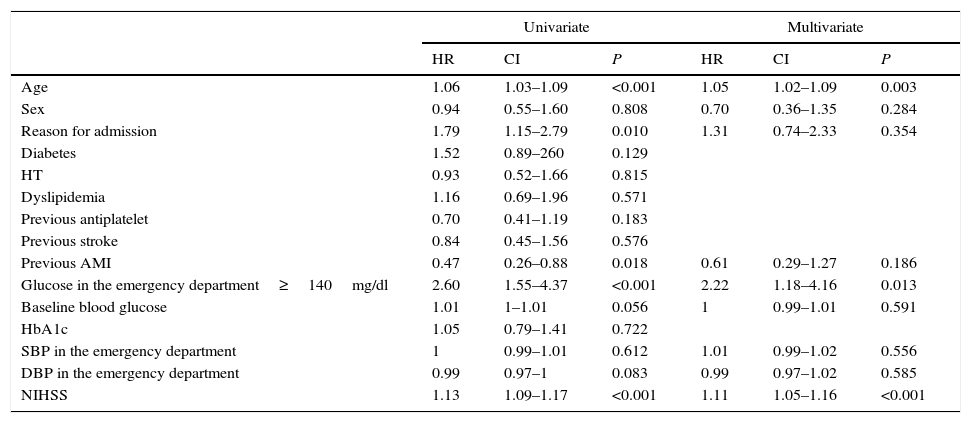
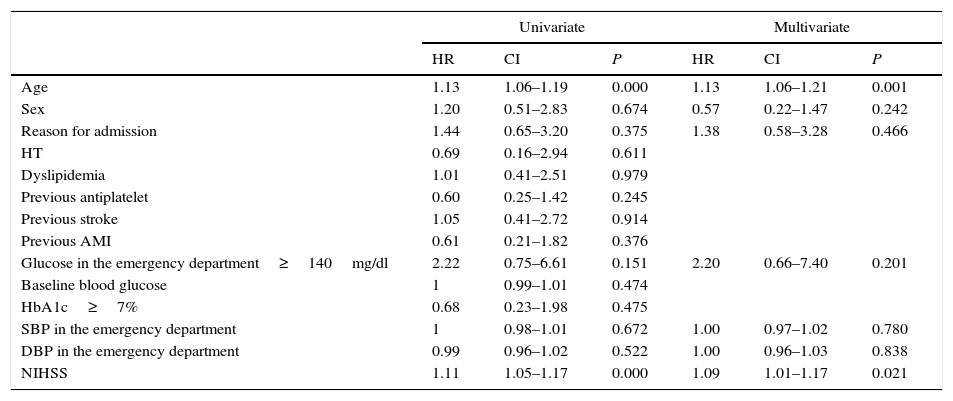
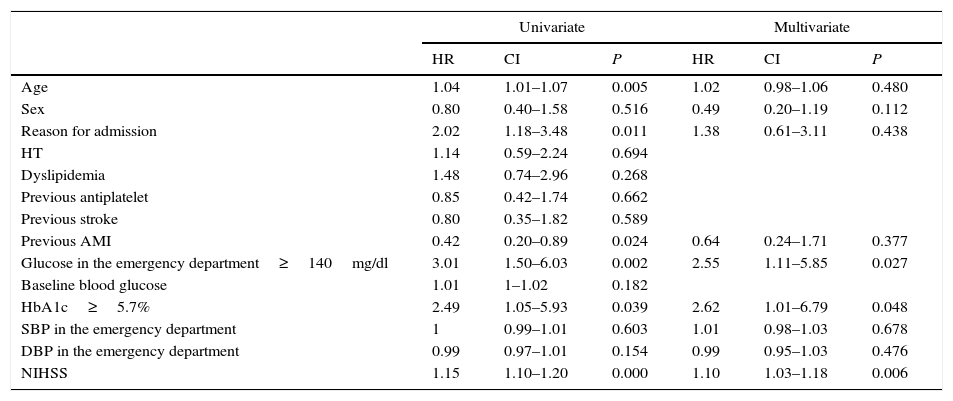
Higher mortality was observed in patients who had been admitted with plasma glucose levels≥140mg/dl (hazard ratio [HR]=2.22, 95% CI: 1.18–4.16, P=0.013) after adjusting for various factors. This relationship was not confirmed in diabetic patients (HR=2.20, 95% CI: 0.66–7.40, P=0.201) and was in non-diabetics (HR=2.55, 95% CI: 1.11–5.85, P=0.027).
In diabetics, HbA1c≥7% was not associated with poor prognosis (HR=0.68, 95% CI: 0.23–1.98, P=0.475), whereas non-diabetics with admission levels of HbA1c falling within the pre-diabetes range (5.7–6.4%) had a higher mortality (HR=2.62, 95% CI: 1.01–6.79, P=0.048).
ConclusionAdmission hyperglycemia is associated with a worse prognosis in patients without diabetes admitted for stroke, but this relationship was not seen in diabetics.
In non-diabetic patients, HbA1c levels in the pre-diabetes range are associated with higher mortality.
La hiperglucemia de estrés se ha relacionado con peor pronóstico en pacientes ingresados en unidades de críticos. El objetivo del estudio es evaluar el efecto de la glucemia en urgencias y la hemoglobina glucosilada (HbA1c) en la mortalidad en pacientes con accidente cerebrovascular y ver si esta relación depende de la presencia de diabetes.
Material y métodosAnálisis retrospectivo de 255 pacientes ingresados por un episodio cerebrovascular agudo. Se recogieron los datos de glucemia en urgencias y HbA1c en las primeras 48h.
La presencia de diabetes se definió en función de los antecedentes médicos, valores de glucemia basal y HbA1c en el ingreso.
Se evaluó la mortalidad en los primeros 30 meses tras el episodio agudo.
ResultadosEl 28,2% de los pacientes presentaban diabetes.
Se observó mayor mortalidad en pacientes con glucemia al ingreso≥140mg/dl (hazard ratio [HR]=2,22; IC95%: 1,18–4,16; P=0,013) tras ajustar por distintos factores. Esta relación no se confirmó en pacientes diabéticos (HR=2,20; IC95%: 0,66–7,40; P=0,201) pero sí en no diabéticos (HR=2,55; IC95%: 1,11–5,85; P=0,027).
En diabéticos, una HbA1c≥7% no se asoció a peor pronóstico (HR=0,68; IC95%: 0,23–1,98; P=0,475) mientras que los no diabéticos con HbA1c al ingreso en rango de prediabetes (5,7–6,4%) presentaron mayor mortalidad (HR=2,62; IC95%: 1,01–6,79; P=0,048).
ConclusiónLa hiperglucemia al ingreso se asocia con un peor pronóstico en pacientes sin diabetes ingresados por un accidente cerebrovascular agudo, pero esta relación no se demuestra en diabéticos.
En pacientes no diabéticos, una HbA1c en rango de prediabetes se relaciona con mayor mortalidad.