Obesity causes important alterations in the respiratory physiology like sleep obstructive apnoea (SOA) and obesity-hypoventilation syndrome (OHS), both associated with high morbidity and mortality.
Also, these entities are clearly infradiagnosed and in the case of OHS the prevalence is unknown in the general obese population.
To determine the prevalence of OHS in the population of patients with morbid obesity and to know the comorbidity related with OHS, the associated respiratory symptoms and the pulse oximetry alterations.
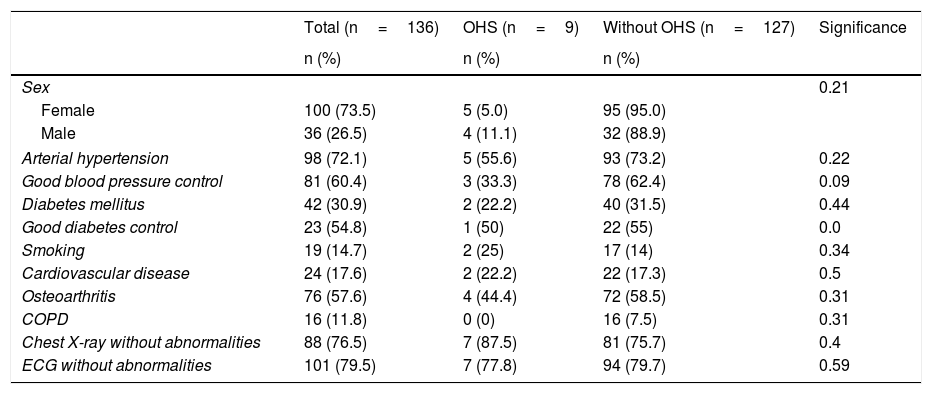
Patients and methodDescriptive study. Selection of 136 adult patients with morbid obesity (BMI>40). Collected were anthropometric data, toxic habits, concomitant disease, symptom data, analytic data, dyspnoea grade, sleepiness scale (Epworth Test), electrocardiogram, chest X-ray, spirometry, nocturne ambulatory pulse oximetry and arterial gasometry.
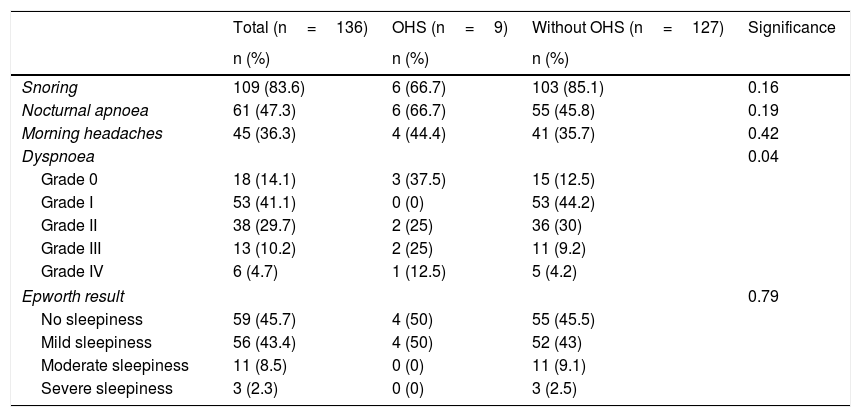
Results136 were studied, mean age 60 years old (SD 12.9 years), 73% (98) were women; 6.6% of patients presented diurnal hypercapnia indicative of OHS; 72% presented high blood pressure, 44% dyslipidaemia, 18% presented cardiovascular disease, 83% snored and 46% had apnoea; 30% presented stage II dyspnoea and 10% stage III.
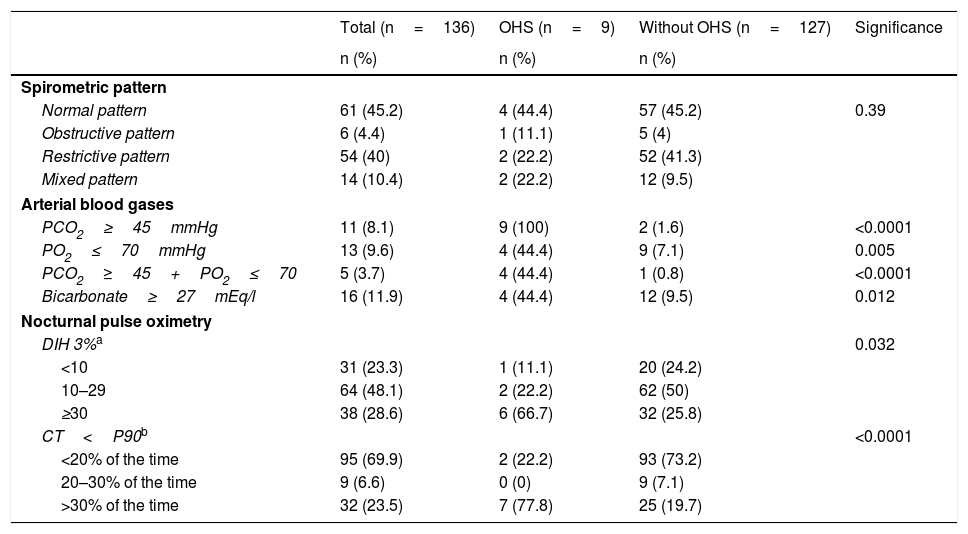
The desaturation/hour index was above 3% ≥30 of occasions in 28.6% of patients and the percentage of patients with saturations <90% more than 30% of the time was 23.5%. The results were worse in patients with OHS.
ConclusionsThe prevalence of OHS was lower than expected. Noteworthy were the high comorbidity of cardiovascular disease and the high frequency of respiratory symptoms associated with important alterations of pulse oximetry.
La obesidad ocasiona alteraciones importantes de la fisiología respiratoria como el síndrome de apnea-hipoapnea del sueño (SAHS) y el síndrome de obesidad-hipoventilación (SOH), asociados ambos a elevada morbimortalidad.
Además, estas entidades están claramente infradiagnosticadas y en el caso de SOH se desconoce la prevalencia en población general obesa. Los objetivos del estudio son: determinar la prevalencia del SOH en población de pacientes con obesidad mórbida y conocer la comorbilidad asociada al SOH, la clínica respiratoria y las alteraciones de la pulsioximetría.
Pacientes y métodoEstudio descriptivo. Se seleccionaron 136 pacientes adultos con obesidad mórbida (IMC >40). Se recogieron datos antropométricos, hábitos tóxicos, enfermedades concomitantes, registro de síntomas, datos analíticos, grado de disnea, escala de somnolencia, electrocardiograma y radiografía de tórax. También se realizó espirometría, pulsioximetría nocturna domiciliaria y gasometría arterial.
ResultadosSe estudiaron 136 pacientes, con una media de edad de 60 años (DE: 12,9 años); el 73% (98) fueron mujeres. El 6,6% presentaban hipercapnia diurna indicativa de SOH. Presentaban hipertensión arterial (HTA) el 72%, dislipidemia el 44% y enfermedad cardiovascular (ECV) el 18%, sin diferencias según presentaran o no SOH. Tenían ronquidos el 83% y apneas el 46%. El 30% presentaban disnea grado II y el 10% grado III.
El índice de desaturaciones/hora (IDH) superior al 3% en ≥30 ocasiones estaba presente en el 28,6% de los pacientes y el porcentaje de tiempo con saturaciones de O2<90% más del 30% del tiempo lo presentaban el 23,5%, resultados peores en pacientes con SOH.
ConclusionesLa prevalencia de SOH es más baja de la esperada. Destacan la elevada comorbilidad cardiovascular y frecuentes síntomas respiratorios, presenten o no SOH, así como alteraciones importantes en la pulsioximetría.