Objective: The focus of this paper is to present the psychometric validation of the ABCDE-Psy, an hetero-administered psychological assessment scale for measuring people's acute stress response to critical and potentially traumatic events. Method: An item bank is proposed based on a literature review and expert opinion. Its psychometric validation follows the usual scheme of classical test theory. The scale was administered to two samples, the first watching simulated cases (n = 60) and the second participating in real environments (n = 213). Results: The ABCDE-Psy scale shows solid psychometric properties in terms of both reliability (α = .793; 95 % confidence interval 0.764 - 0.822) and validity. Construct validity was supported by a univariate model of the scale based on confirmatory factor analysis (CFI: 0.956, TLI: 0.976, χ2: 2.567, p = .784, R2: 0.681). Conclusions: The results demonstrate that the ABCDE-Psy scale can be used as a reliable and valid hetero-administered measure for primary psychological assessment of the acute stress response to potentially traumatic events. This has important practical and clinical implications and opens up a new area of research in emergency psychology.
Primary assessment is a vital medical process for dealing with trauma victims and the critically ill in emergency situations. The aim of this process is to promptly assess and treat all life-threatening injuries (Evans et al., 2021). Time is a critical factor in this process as the likelihood of recovery decreases significantly with time (Cowley, 1975; Gauss et al., 2019; Waalwijk et al., 2022).
Many of the assumptions that guide and underpin the primary assessment of physical health in emergency contexts (Thim et al., 2012) also apply to psychological assessment and intervention. One of these is assessment and intervention as soon as possible, with a window of opportunity of not more than six hours to prevent post-traumatic symptoms (Carmi et al., 2016; Cohen et al., 2016; Iyadurai et al., 2018; Zohar et al., 2011). This is possible by systematically assessing key psychological functions, promoting assessment and intervention at each stage of the care process, and adapting to people's changing needs (Eshel et al., 2018; Farchi et al., 2024).
The increasing presence of psychology professionals in emergency settings should be supported by procedures, techniques, assessment tools and intervention protocols that facilitate their work and decision-making. These protocols must be quick to apply and easy to integrate into routine assessment procedures (Thim et al., 2012). They also need to be sensitive to the entire continuum of people's stress response and not just to the presence of psychopathology, distinguishing them from other tools such as those aimed at psychiatric assessment in emergencies and/or those that assess post-traumatic risk in the months following an incident/accident.
Detection of the first stress response following a critical or potentially traumatic event relies on emergency professionals recognizing behavioral symptoms through subjective observation. Without underestimating the value that subjective assessment can provide, it seems evident that an objective, standardized approach developed to be more sensitive and rapid would allow for better management of symptoms and risk assessment (Matson et al., 2022). Few procedures and tools have been developed in this context, and those that have been used tend to be translations of other procedures or tools developed in a clinical context (post-traumatic stress or depression and anxiety scales; Pérez-González & Jarne, 2025). This fact means that in their conceptualization they are not suitable for this context. The main reason for this is that a person's response immediately after an incident and in the hours that follow cannot be considered a clinical indicator of psychopathology, due to duration criteria (the emotional reaction in the first hours can never be the object of a psychopathological diagnosis). Variables such as duration, intensity or ability to cope with the situation, among many others, can lead to them becoming psychopathological and, therefore, subsidiaries to clinical assessment. But this does not happen in the first stages. Therefore, such procedures and tools do not meet the specific needs of the emergency field, such as being a non-diagnostic measure and focusing on risk assessment in a minimum time, and not weeks and months after the incident (Matson et al., 2022). Psychological assessment in emergencies differs from other areas of psychology in three aspects: the temporal/spatial factor, the operational/brevity factor and can be managed by any healthcare emergency and/or crisis operator (Pérez-González & Jarne, 2025). Based on our own professional needs and perceived gaps, and after reviewing the literature, we find that there is no non-diagnostic measure for assessing a person's initial psychological response in the minutes and hours immediately following a potentially traumatic event.
The main aim of this study is to propose a psychometrically sound primary assessment tool to facilitate the assessment of the initial psychological state of people affected by an emergency or disaster. We also assess the usefulness of this scale for better understanding the acute stress response of affected people and for detecting possible psychological risks. This new scale must be able to detect possible complications in the different psychological functions in order to determine an intervention adapted to the needs identified and to allow assessment and intervention as soon as possible. In fact, the acronym ABCDE (Thim et al., 2012) comes from a mnemonic device for remembering the dimensions to be assessed.
The focus of this paper is therefore to present the ABCDE-Psy psychological assessment scale for measuring people's acute stress response to critical and potentially traumatic events, proposing a bank of items based on a review of the literature and expert opinion. For psychometric validation, we followed the usual scheme of classical test theory.
MethodScale constructionThe ABCDE-Psy scale was developed in three main phases, following the guidelines recommended by previous studies (Anita et al., 2023; Hinkin, 1998; Hinkin et al., 1997).
In the first phase, an initial bank of items was created to assess the acute stress response (ASR) construct. Based on an intensive literature review, the latent variable ASR was defined as a person's initial psychological response to a highly stressful or potentially traumatic event (Friedman, 2015). It is an immediate and transient response, usually with an acute course (high-intensity manifestations that change over hours and gradually decrease over days). ASR is considered a functional and adaptive response, adjusted to the stressor that causes it, and is in no way pathological in itself (WHO, 2022). Only when ASR remains invariant over time (intensity and duration criteria) can it be a risk factor for the development of traumatic psychopathology, as in the case of Acute Stress Disorder (ASD) or Posttraumatic Stress Disorder (PTSD) (Friedman, 2015). In the context of crisis and emergency interventions, the need for psychological care focuses on ASR, which is the target of the ABCDE-Psy scale.
As an adaptive response, ASR is not coded as a category in clinical diagnostic systems and has so far been defined more conceptually than operationally. Taking this into account, and in line with the ICD-11 description (2022), the ABCDE-Psy scale has chosen the broad general areas of standard psychological examination as the domains for assessing the ASR construct; that is, the level of mental activation and basic cognitive functions for mental functioning (Awareness/Orientation), the intensity of interaction with others through both motor (Behavior) and verbal (Communication) behavior, advanced cognitive functions including thought content (Deliberation/Thinking), and finally emotions (Emotion). The five domains are intended to cover the behavioral, mental (understood as the internal, non-directly observable aspects of the human psyche) and emotional spectra, which together constitute and coordinate what we understand by mind and human behavior. A description of each domain can be found in Supplementary material 1.
The scale is designed to be administered by a health professional who is not necessarily an expert in assessing the emotional state of people who have experienced a critical and potentially traumatic event. The items and domains are designed to help emergency teams identify possible risks in people's psychological state, provide guidance on how to act, and allow them to activate emergency psychological services for more specialized assistance. In this way, the ABCDE-Psy approach helps to quickly identify the need for psychological assistance and guides the intervention of the professionals involved, who are not necessarily specialized psychologists.
The items had to be able to assess a person's response in the first hours, considering both normal functioning and potential risk responses. Three of the research authors (experts in psychopathology and emergency psychology) discussed each item, discarding those that seemed confusing or redundant. They finally selected a total of 33 items, ensuring that they were representative of the five proposed domains.
The content validity of the selected items and each factor/dimension was assessed by nine external experts (three national academic experts, three national health experts, and three international health and academic experts). A total of seven responses (78 %) were received. For each item, the experts were asked how much they agreed with its wording, how well they understood it, how difficult they found it to assess and how well it fit into one of the domains of the scale (awareness, behavior, communication, deliberation and emotion). The experts gave the scale a reasonable score, highlighting its potential as a tool for assessing acute stress responses and the fact that it can be used by any health professional, not only psychologists, but especially emergency medical technicians (who are the first to arrive). The concordance index estimated by Feiss Kappa shows a significant fit (Z = 2.007, p = .045 for difficulty; Z = 1.617, p = .106 for understanding; and Z = 5.72, p < .001 for dimensional fit). Following feedback from the experts, some items were slightly reworded, and one item was split into two, resulting in 34 items (see Supplementary material 2).
The second phase involved the first administration of the scale in a controlled and simulated environment. For this purpose, six videos were created to simulate eight profiles of psychological responses to different emergency situations, taken from real cases. The video scripts were written by the authors and focused on six representative situations of the work of a health emergency psychologist (delivering bad news, psychological care of a traffic accident victim, care of a victim of sexual violence, support of family members in the event of sudden death, and dealing with the risk of suicide) with four typical response patterns (inhibited/dissociated, restless/agitated, emotionally overwhelmed, and showing self-aggressive behavior). Before carrying out the simulation, a pilot test (n = 19; 13 technicians and six psychologists) was conducted to test the items, and particularly, the functioning of the session. The inclusion criterion was a minimum of three years of experience in emergency care and 12 were women (63.15 %) and the rest were men. During the pilot test, the participants were trained to use the scale before watching the simulated cases on video. Each professional answered all 34 scale items after each video, indicating the presence or absence of the content of each item in each of the cases presented, based on their own professional assessment criteria. They also responded to other additional assessment measures (PCL-ICD-11 and the checklist of the psychologists of Emergency Medical System [EMS] of Catalonia) to have evidence of concurrent validity with external variables. The PCL-ICD-11 is used to assess the presence and severity of PTSD symptoms. It consists of seven items with a Likert-type response from 1 to 5. It has good psychometric properties of internal consistency (α > .85) and diagnostic validity for identifying PTSD (AUC > .90 and kappa ≥ .75; Reguera et al., 2021). The checklist is a risk assessment tool for Acute Stress Disorder. It consists of 57 items divided into four groups of symptoms (cognitive, emotional, behavioral and physiological). It is a non-validated assessment measure but is widely used by EMS psychologists in clinical practice. The reliability data in our sample is α > .94, as shown in Table 1.
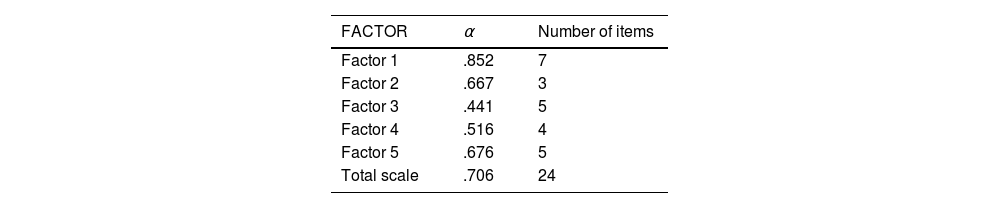
Reliability analysis of the scale from the first pilot test (n = 19).
Note: The 95 % confidence interval is shown in parentheses.
Finally, the third phase consisted of selecting a reduced number of items based on the scale's application to a test sample, and then psychometrically testing the result.
The test scale was administered to a test sample (n = 60) with trained assessors. Emergency medical technicians (EMT) and psychologists were asked to assess the content of the videos (the same eight simulated cases) using the designed scale and the other assessment measures described above (PCL-ICD-11 and EMS psychologists’ checklist). This test sample consisted of 39 EMTs and 21 psychologists. The participants ranged in age from 22 to 62 years, with a mean of 38.88 years (X̄ = 40.88 for EMTs and X̄ = 35.11 for psychologists). The mean years of experience were 14.68 and 5.00 for the EMTs and psychologists respectively. All participants voluntarily attended the training sessions on the scale and its use after watching the simulated videos outside their working hours. They received no financial or labor compensation.
For this test sample, the estimation of Cronbach's α, considering the scale as a unidimensional structure, showed an interesting result (α = .706), but the scale was constructed for multidimensional assessment. Therefore, the possible factor structure was estimated through an Exploratory Factor Analysis (EFA), limiting the extraction to the first five theoretical indicators, obtaining a total of 57.48 % of explained variance and reliability values for each dimension, as shown in Table 2. Both values were considered sufficient to maintain the test scale as a final scale reduced to 24 items, eliminating factor loadings <0.400. Of course, given the limited size of the test sample, the results do not allow this factorial structure to be considered a proven solution. The option of a unidimensional scale is clearly the best, but this initial exploration has allowed us to identify some factors that could provide complementary information.
We consider the results of this third phase to be sufficient to apply the scale in this format as a final scale to a real sample in order to carry out a full psychometric study.
ParticipantsThe sample used to validate the final scale (see Annex number 1) included emergency medical professionals from the Emergency Medical System (EMS) of Catalonia. The EMS is organized in health regions and the sampling was carried out in the most populated area (Metropolitan Area around Barcelona), which guarantees the high representativeness of the phenomenon studied. An accidental sampling was carried out since the responses were obtained in each care act and that was precisely the inclusion criterion, that urgent psychological assistance was requested. The final sample size was set by defining a value of α = 0.05 and a maximum sampling error of 0.04 under the assumption of maximum population indeterminacy π = 1-π = 0.50.
A total of 213 responses were obtained over a period of less than three months. Of the participants, 65.7 % were psychologists, 31.4 % were EMTs and 2.9 % were physicians. The age ranged from 19 to 57 years with a mean of 35.16 years (X̄ = 34.31 for psychologists, X̄ = 36.00 for EMTs and X̄ = 45.67 for physicians). More than half of the sample was female (62.4 %). The mean number of years of experience was 1.83 for psychologists, 9.87 for EMTs and 16.67 for physicians. Further information on the participating professionals is given in Table 3.
Table 4 shows data describing the interventions carried out during the application of the scale, including the age and sex of the people assisted and the main reason for the incident requiring professional attention.
Descriptive results of the interventions carried out during the application of the scale to the assisted people.
Following its conceptual and operational definition, the ABCDE-Psy scale was administered in the field. This version contains a total of 24 dichotomous response items (presence/absence) to be answered by the professional when carrying out the primary psychological assessment of the affected person after an experience of crisis and emergency. The scale takes about five minutes to complete.
Each professional also completed an ad hoc satisfaction survey on the use of the scale. The survey consists of 10 items that assess the user's satisfaction with the scale and the extent to which it improves their professional competence.
Data collection procedureA health area in Catalonia (metropolitan area S in Barcelona) was selected for the application of the final sample. The purpose of the scale and how to use it were explained to all emergency professionals. To this end, an explanatory video and an infographic were produced and displayed in a visible place in the ambulance to remind them of the use of the ABCDE-Psy scale. All professionals in the care units (ambulances) were instructed to fill in the scale to assess the mental state of the person being treated in any care situation where it was felt that the incident could have a psychological impact on the person. Therefore, the scale was applied to different types of incidents, including sudden death (caring for family members), traffic accidents, sexual violence, anxiety, drowning, fire, violent death (including suicide), other violence, and other circumstances implying psychological distress.
All participants voluntarily completed the scale immediately after the professional assessment of the person in question. To do this, a link was provided on the health tablets to complete the proposed items (managed by the Qualtrics platform under license from the Universitat Oberta de Catalunya). After using the ABCDE-Psy scale, each professional completed the satisfaction survey. In all cases, the administration was carried out in accordance with current data protection regulations and was validated by the Ethics Committee of the same university (CE22-PF40) and by that of the Institut d'Investigació Sanitaria Pere Virgili (077/2023). The sample did not receive any financial or labor compensation for their participation.
ResultsBased on the application of the final scale to the described sample (n = 213), the usual psychometric indicators of classical test theory were analyzed. Table 5 summarizes the main statistics of the observed distribution of each component of the scale.
These values give distributions with a negative bias, as expected, and a small dispersion range, also as expected. This would indicate a very low complexity scale proposal based on free population distributions.
The overall reliability of the scale was estimated using the intraclass correlation coefficient, and was found to be α = .793 (95 % Confidence Interval 0.764 - 0.822). The unidimensional consideration of the scale is based on the fact that the dimensions considered do not have sufficient empirical anchoring to be considered as independent constructs in this measurement structure. Table 6 shows the results of the Confirmatory Factor Analysis, as evidence of construct validity in the unidimensional scenario and in the multifactorial scenario (analysis performed with Mplus) for the 18 items finally selected. Items with correlations with the total scale below 0.800 were eliminated from subsequent analyses to maximize unidimensional effects. Given the distribution observed in the scale items, an arbitrary solution was chosen that involves fewer restrictions (AGLS – Arbitrary Generalized Least Square).
The scale is considered as unifactorial and the different components as secondary indicators without sufficient entity as separate measurement factors. The correlations between the dimensions and the total scale ranged from r = .45 to r = .82, all of which were clearly statistically significant (p < .001).
With regard to evidence of concurrent validity, the lack of a measure similar to the ABCDE-Psy prevented a sufficiently rigorous approach to the issue. This question does not imply a limitation of the validity analysis since the validity evidence provided is clear. However, indirect indicators should be sought over time to estimate in a more robust way the predictive capacity of the scale and its classification capacity. As evidence of ecological validity, we can present the data from the satisfaction survey of the professionals who administered the scale. In this case, 86 % of the professionals in the final sample considered it to be simple, useful and relevant; that they had adequate time to administer it; that they would use it in their daily professional activity; that they would recommend it to others; and that it would give them confidence in decision-making and final triage. Therefore, pending further study, the initial data are considered sufficient.
Finally, Table 7 presents a proposed scale based on the observed distributions, in which the total score plays the main role and the dimension scores play a secondary role. The use of centiles was chosen because of the asymmetry observed in the original distributions.
Of course, this table is only descriptive in nature and therefore the key data is the interpretation that should be attached to each score obtained. To this end, we propose the following interpretation of the results of the scale, pending the specification and demonstration of convergent and ecological validity (Table 8).
Interpretation criteria.
The main aim of this study was to develop and validate a hetero-administered psychological assessment scale to assess people's acute stress response to critical and potentially traumatic events. Currently, there are no assessment tools with these characteristics, and those that are used are translations of tools for measuring psychopathology (post-traumatic stress or depression and anxiety scales; Pérez-González & Jarne, 2025). For its part, the ABCDE-Psy scale is a non-diagnostic measure adapted to the specific needs of the emergency field. Firstly, it is a very short measure with only 18 items and takes less than five minutes to complete, which means that it considers the important time factor in the emergency field (Carmi et al., 2016; Cohen et al., 2016; Iyadurai et al., 2018). Secondly, it comprehensively assesses people's acute stress response by examining all psychological functions (Awareness, attention and orientation; Behavior; Communication; Deliberation/Thinking; and Emotion), just as any professional would do to assess a person's psychological state (ICD-11, 2022). It is also consistent with the ABCDE mnemonic device for assessing physical status (Thim et al., 2012). Thirdly, it is a non-invasive tool that respects the person's natural response and recovery (Layne et al., 2007; NICE, 2018). The ABCDE-Psy scale guides primary assessment without requiring input from the affected person.
The methodology was respectful and prudent, first using simulated videos and only applying the items to a real sample after testing. The assessment context was also considered, and the methodology was therefore ethically sensitive to the severity of the events that trigger an acute stress response and to the needs of those involved (PAHO, 2022). Firstly, all interventions in the context of emergencies are carried out with informed (verbal) consent (Pérez-González et al., 2023). Secondly, it is a non-invasive scale, carried out by the professional and does not alter the intervention protocol. The most appropriate professional action is derived from the first assistance and psychological examination of the affected person (which includes the ABCDE-Psy scale), such as decision-making regarding patient safety, the application of Psychological First Aid (PFA), the activation of other specialized resources or transfer to the hospital emergencies. In this way, decisions are based on the patient's stress response profile, so interventions are pertinent, and the application of the scale does not delay the necessary care. Contrarily, the use of the ABCDE-Psy scale helps to prioritize actions to reduce the emotional impact after the event. Likewise, both the methodology and the context in which the ABCDE-Psy scale is used were designed to ensure a response that is as plausible as possible in relation to reality. In addition to being hetero-administered by professionals, and not a self-report measure that requires a response by the person in ASR, the scale was always applied in accordance with the principle of ecological validity of measurement without altering real conditions (Andrade, 2018). Thus, in the context of the video simulations, it was possible to apply other assessment measures, but this was not feasible in the real sample, as the aim was to minimize interference and validate the scale in a context as close as possible to the real application context. Taken together, the ABCDE-Psy scale and its application context pursue a principle of beneficence where the assessment has a clear purpose: to improve the psychological state of the affected person, detect possible risks and facilitate decision-making about the most appropriate resources and interventions (Farchi et al., 2024).
The present study demonstrates the strong psychometric properties of the ABCDE-Psy scale. Reliability was consistently good to excellent. Construct validity was supported by an unifactorial model of the scale based on confirmatory factor analysis. Even with the five factors found through exploratory factor analysis of the scale's application to simulated videos, the unidimensional consideration of the acute stress response from the ABCDE-Psy scale was not compromised. Taken together, the results demonstrate that the ABCDE-Psy scale can be used as a reliable and valid hetero-administered measure for primary psychological assessment of people's acute stress response to critical and potentially traumatic events.
The ABCDE-Psy scale has important practical and clinical implications. Firstly, it can be used to assess the current psychological state of people affected by a potentially traumatic event, such as an emergency incident. In this regard, it is important to remember that these people may present with highly variable psychological responses. For example, the maladaptive response may manifest itself in some people as a more inhibited, absent and catatonic response profile, whereas other people faced with the same type of critical experience may show a restless, agitated and even aggressive profile. It is therefore essential to carry out an exhaustive psychological examination that covers all psychological functions and allows for a comprehensive assessment and intervention, not based on possible independent manifestations. Only in this way is it possible to tailor interventions to the individual needs of those affected (Eshel et al., 2018; Farchi et al., 2024) and to truly place them at the center of care (WHO, 2015).
Secondly, the ABCDE-Psy scale can be used not only to identify people's current psychological responses, but also to assess risk. This risk assessment is useful both for triage at the scene and for identifying urgent and immediate care needs, guiding professional intervention and the need for referral. It is important to remember that our ability to identify those at risk remains very limited, hampering efforts to achieve appropriate referral and follow-up and to deliver the intensive prevention programs that are currently in place (Glaspey et al., 2017). The first step towards achieving this could be the development of brief detection tools that can be administered in a short period of time, such as the ABCDE-Psy scale. This will improve the detection and referral process, as professionals will be able to assess priorities and risks at any time and tailor interventions to these needs. This will allow for effective and targeted prevention measures, such as identifying suicidal ideation, thus facilitating follow-up and improving the process. It is important to remember that early intervention in emergency psychology, with a preventive approach, is crucial to address mental health problems (Gidron et al., 2018). The lack of accurate tools to identify people at risk often limits our ability to provide effective interventions in a timely manner. This can have serious consequences, particularly for critical issues such as suicidal ideation or self-destructive behavior.
Thirdly, assessment with the ABCDE-Psy scale does not have to be a single application measure, but can be used by professionals as a pre-test and post-test measure to assess the minimum change since the early intervention offered to the person. The aim is to be able to assess whether the intervention provided has succeeded in mobilizing the person and reducing the risk initially identified, and to adjust intervention and referral needs accordingly. It should be remembered that people's ASR when faced with a potentially traumatic event has a rapid onset course (Carmi et al., 2016; Cohen et al., 2016; Iyadurai et al., 2018) and that risk responses are more malleable in the first moments (Gidron et al., 2018; Farchi et al., 2018). In order for this intervention not to conflict with the principle of minimal intervention, which guarantees intervention in cases of risk without interfering with people's natural recovery process (Layne et al., 2007; NICE, 2018), it is necessary to be very precise and to be able to accurately assess the effect of each minimal intervention.
Finally, according to the professionals who have used it, the ABCDE-Psy scale has a direct impact on pre-hospital (and even out-of-hospital) care, both in the use of the tool itself and in improving professionals’ skills and confidence in decision-making and final triage. In this regard, it can be a powerful tool to reduce the cost-benefit equation by reducing the former and increasing the latter, as well as improving communication between the team of professionals.
LimitationsThis study has several limitations. Firstly, the scale was applied to a real sample in a single health area in Catalonia (metropolitan area S in Barcelona) and in a specific season (summer). Given the possibility of differences between areas and seasons, especially in the type of events to which the scale is applied, future research will need to use the scale in a larger sample across all of Catalonia. It is also necessary to test the scale in other contexts, such as telephone helplines, in order to assess any necessary adaptations. Secondly, it should be noted that the ABCDE-Psy scale is not yet part of the emergency team's care procedure, which is why it had to be applied on a voluntary basis by the professionals using it. This may have an impact on the results obtained, especially with regard to the professionals’ satisfaction with the scale, as it is expected that those most motivated to use it would have used it more. This second limitation is currently being addressed based on the good results obtained in the present study, both at the healthcare and research level. On one hand and as an assessment tool, both in ordinary interventions and in Multiple Affected Incidents (MAI; Cuartero & Pérez-González, 2023) work is being done to homogenize the healthcare report of professionals by adding the assessment with the ABCDE-Psy scale. On the other hand, in other ongoing research, the use of the ABCDE-Psy scale is already mandatory for all professionals. Thirdly, it should be noted that it was difficult to find other tools with which to compare the ABCDE-Psy scale, as there was no other measure to assess its characteristics. This limits concurrent validity. Fourthly, although the experience of psychologists may seem limited in terms of years, it is important to note that it refers only to experience in the field of emergencies, and not to all their clinical experience. Even more so if we consider that psychological intervention is not discretionary and provided in a homogeneous manner to everyone, but to people who present a risk in ASR. In any case, the short experience in the field of emergencies is understandable if we take into account that today there is no specialty or profile of "emergency psychologist" at a European level, except in Portugal. Within emergency medical systems, it is a profile that has been incorporated very recently. Similarly, the health training of psychologists is complemented by specific postgraduate training in emergency psychology that is very recently offered by universities. Finally, language is another limitation to consider. The ABCDE-Psy scale was developed and validated in Spanish (Spain). Once validated, it could be used in Latin America, but it will be necessary to have versions in Catalan, Basque and Galician for national use and in English for international use. In this regard, it is known that the acute response to stress is mediated by many variables of a cultural nature. For example, culture determines to a certain extent the level of emotional expressiveness or the perspective of protection of the family and/or social group against the possibilities of individual response (Jobson et al., 2022; Patel & Hall, 2021). Our sample is part of the broad context of Western culture and more specifically of the Mediterranean one. In the future, the reliability and validity of the scale should be studied in other Western contexts (Nordic or Anglo-Saxon countries, for example) and other cultures (Islamic or Far Eastern, for example). This includes the expressions of the assessment items both in their content and in their linguistic expression. However, we believe that, in terms of concepts, the scale scheme, insofar as it represents the universal response of the species, can serve as a basis for this task.
ConclusionsThe ABCDE-Psy fills the gap for an assessment tool in the field of emergencies that assesses people's acute stress response to critical and potentially traumatic events. The psychometric study carried out demonstrates the good psychometric properties of the scale in terms of reliability and validity. The use of the ABCDE-Psy scale facilitates the assessment process of professionals, reduces the amount of time required and improves the effectiveness of current procedures. Likewise, the availability of a scale for assessing the acute stress response opens the door to new research opportunities based on assessment and intervention in the context of crises and emergencies.
AgreementsWe are grateful to the professionals for their participation and commitment to this study. We would also especially like to thank Maria José Santos Arevalo, Xavi Rico Rodríguez, Gemma Cuartero and Miquel Torelló Masa for their invaluable help and dedication throughout this research.
Source of fundingThis research was supported by the MAPFRE Foundation and the Department of Research and Universities of the Government of Catalonia (2021 SGR 00366).
Note: The items are not validated in English. The content of the table is only a translation of the items in Spanish for eraser understanding.