We read with great interest the article by Berdugo-Hurtado et al., describing linitis plastica (LP) as a diagnostic challenge1. As the authors clearly explain, LP can be a diagnostic challenge in 30–36% of cases where there is no histopathology confirmation from endoscopic biopsies2. More invasive diagnostic techniques are often used in these patients, such as exploratory laparoscopy or laparotomy, with the latter performed when the former is not possible.
Although exploratory laparoscopy or laparotomy is indicated when there is no clear preoperative diagnosis, these techniques are not without risk. Accordingly, the patient may refuse or delay these diagnostic techniques without a clear preoperative diagnosis, or have a high surgical risk, which would contraindicate surgery. We believe that positron emission tomography combined with computed tomography (PET-CT) could be useful in these cases.
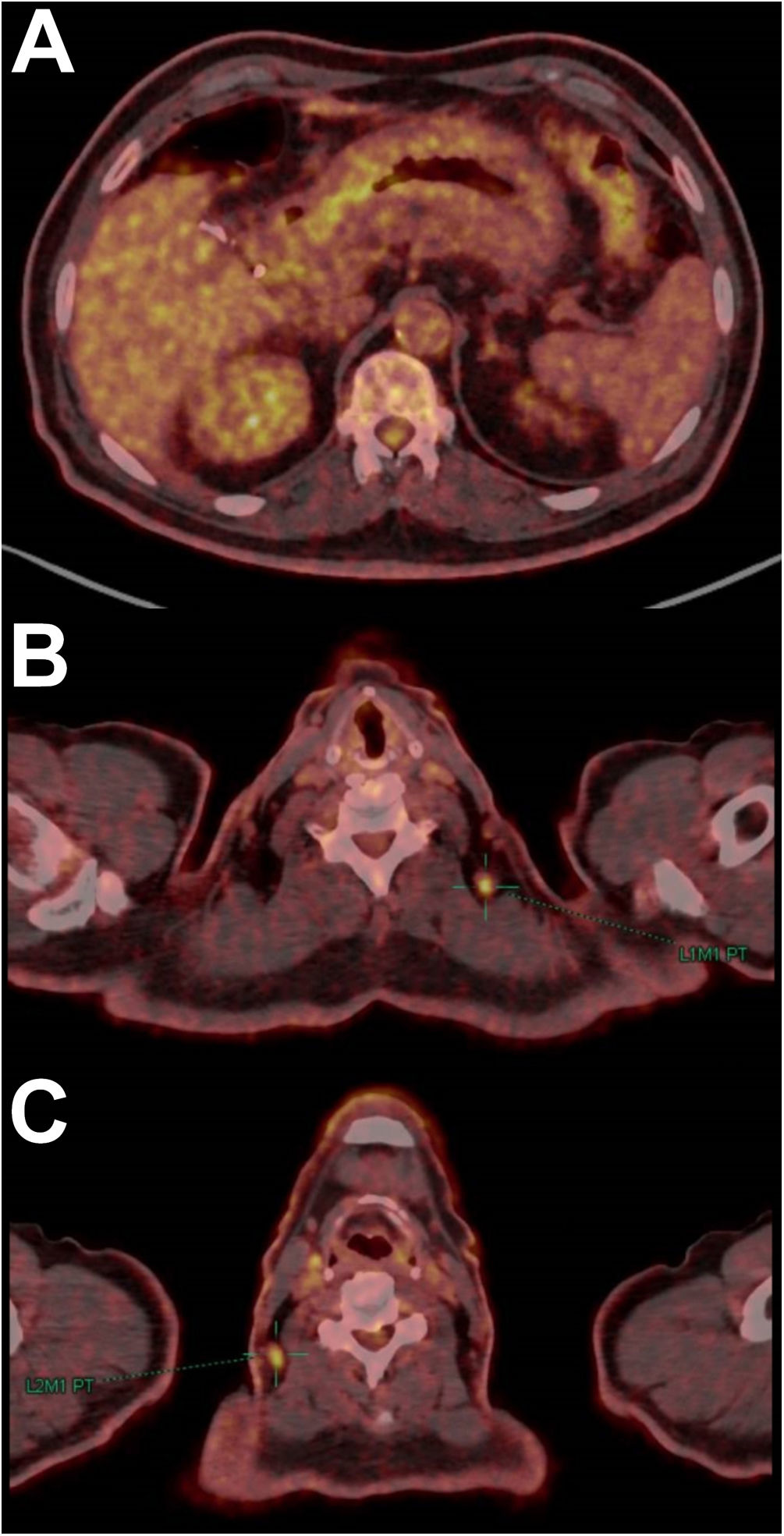
We recently had a clinical case similar to the one described by Berdugo-Hurtado et al.1 Our patient was a 62-year-old male who consulted with dyspepsia, early satiety and weight loss of 12kg in the previous 4 months. Gastroscopy revealed a thickening of the gastric mucosal folds in the regions of the body and antrum; multiple routine endoscopic biopsies were taken. CT revealed a diffuse thickening of the gastric wall, more evident in the distal body and antrum. Endoscopic ultrasound revealed thickening of all layers of the gastric wall in the body and antrum; fine-needle aspiration biopsies were taken from the gastric wall, plus multiple biopsies with a conventional oesophagogastroscope. The biopsies showed regenerative glandular foveolar hyperplasia and chronic gastritis. As no evidence of malignancy was found in the biopsies or of lymphadenopathy or peritoneal implants in the CT scan, the patient was unwilling to undergo exploratory laparoscopy without a clear preoperative diagnosis, so it was decided to request a PET-CT (Fig. 1), and this was performed two months after the previous CT. Due to the low metabolic activity in the abdomen, the PET-CT findings were of uncertain pathological value. Still, the nodular images and the rarefaction of the perigastric fat visible in the CT part of the PET-CT, the slight metabolic enhancement in the gastric antrum, and the increased metabolic activity in the left supraclavicular fossa (Troisier sign/Virchow node), led to the diagnosis of gastric adenocarcinoma with lymph node metastasis and peritoneal carcinomatosis. Finally, with the suspected diagnosis provided by the PET-CT, the patient agreed to undergo exploratory laparoscopy, with this being a more definitive diagnostic test than a biopsy of the left supraclavicular lymphadenopathy in a patient without high surgical risk. The laparoscopy revealed diffuse gastric thickening and multiple peritoneal implants, and the biopsies were compatible with diffuse gastric adenocarcinoma with peritoneal carcinomatosis.
PET-CT. Axial slices. A) Slight metabolic enhancement in the gastric antrum, several perigastric nodular lesions which do not show increased metabolic activity, and rarefaction of the fat surrounding the stomach. B) Focus of moderate metabolic activity in the left supraclavicular fossa. C) Focus of moderate metabolic activity in the right basocervical region.
Given that poorly differentiated, diffuse, mucinous, or signet-ring cell gastric adenocarcinoma can have poor uptake of 18F-fluorodeoxyglucose on PET-CT2, this test could be of value in guiding the diagnosis of diseases responsible for the diffuse thickening of the gastric wall. Moreover, as occurred in our case, if the diffuse thickening of the gastric wall was due to adenocarcinoma not diagnosed in the preoperative study, PET-CT could reveal distant lesions with increased metabolic activity suspicious of metastasis, these being findings that would support the diagnosis of linitis plastica.
In the event of diffuse thickening of the gastric wall with normal biopsies or results compatible with lymphoid and foveolar hyperplasia and/or chronic gastritis, the differential diagnosis on PET-CT should be established with Menetrier disease (if the gastric mucosa folds are thickened), granulomatous diseases such as tuberculosis, LP and lymphoma2–5.
When the gastric mucosa folds are thickened, a differential diagnosis should be established, particularly with Menetrier disease and waffle-like LP. In Menetrier disease, there is an increase in metabolic activity only in the mucosa3. In contrast, although the metabolic activity may be low in LP, it takes place in the entire gastric wall thickness, even in lymphadenopathy and/or peritoneal implants, if there are any2,4.
In granulomatous diseases such as isolated gastric tuberculosis, which in turn is very rare, the maximum standardised uptake value (SUVmax) will be high, usually above 12, in both the gastric wall and locoregional lymphadenopathy5. In addition, the patient coming from an endemic area, family and personal history, plus tuberculin tests or the interferon-gamma release assay, could help guide the diagnosis.
With regard to LP and lymphoma, it has been documented that lymphoma tends to have a SUVmax >10.4 (sensitivity 59.6% and specificity 78.1%) and the variable SUVmax/maximum wall thickness measured in cm (THKmax) >5.9 (sensitivity 69.2% and specificity 74%). At the same time, in LP the values are lower than these cut-off points4.
In conclusion, although PET-CT does not provide a confirmatory diagnosis, it can guide the diagnosis of gastric wall thickening with normal biopsies or biopsies compatible with lymphoid hyperplasia, foveolar hyperplasia and/or chronic gastritis, allowing the patient to decide about having an exploratory laparoscopy or laparotomy. However, although due to its high diagnostic accuracy, exploratory laparoscopy or laparotomy is indicated when there is no clear preoperative diagnosis of linitis plastica, in patients with high surgical risk, poor performance status, or who reject exploratory laparoscopy or laparotomy, deep-endoscopic biopsies could be repeated in areas with greater metabolic activity, or any accessible lymph nodes or peritoneal implants biopsied percutaneously.