Acute portal vein thrombosis (PVT) is defined as the recent formation of a thrombus in the portal vein and/or main branches, which can also involve the mesenteric or splenic veins.1
The aetiological factors are classified as local (30%), which include cancer and cirrhosis, followed by an intra-abdominal inflammatory focus; and systemic (70%), such as myeloproliferative syndromes, primary antiphospholipid syndrome, paroxysmal haemoglobinuria, factor II or factor V Leiden mutation and deficiency of proteins C, S and antithrombin III. Risk factors related to hormone profile, such as the use of oral contraceptives and pregnancy, are not well established. In 15% of cases there are several causes, while in 30% the cause remains unknown.1,2
We present the case of a 42-year-old male smoker (10 pack-years), who was not a heavy drinker, with a history of grade I obesity, type 2 diabetes, dyslipidaemia and azoospermia who went to Accident and Emergency complaining of sudden-onset epigastric pain accompanied by sweating and dizziness, rectorrhagia and pyrexia of 38°C. On physical examination, weight 99kg, height 177cm, BMI 31.6kg/m2, central fat distribution, gynaecomastia and hypogonadism. On abdominal palpation, he had left iliac fossa pain, without signs of peritonitis. Bloods showed leucocytes 18,900 with neutrophilia, Hb 14.4g/dl, prothrombin time 92%, aPTT 31.7s, fibrinogen 258mg/dl and CRP 16mg/l. X-ray of abdomen was normal.
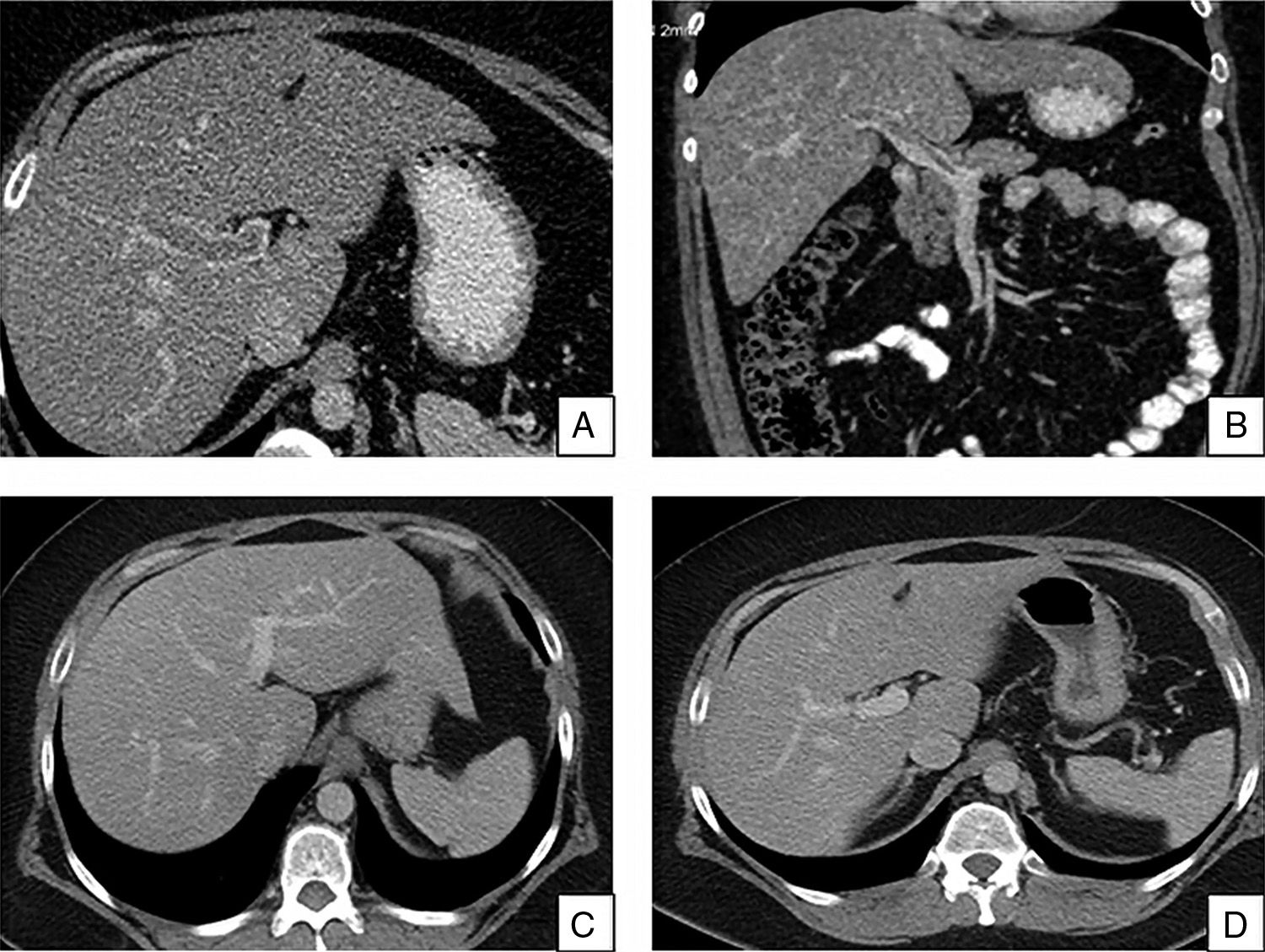
Colonoscopy showed lesions compatible with ischaemic colitis, 28–48cm from the border of the anus and this was confirmed by the biopsies. Computed tomography (CT) of abdomen with contrast (Fig. 1). showed partial thrombosis of the branches of the portal vein, predominantly in the left branch and the splenic and mesenteric veins, with no evidence of abscesses, neoplasia, pancreatitis or liver disease which might explain it. Thrombophilia study (proteins C, S and antithrombin III; antiphospholipid antibodies, paroxysmal nocturnal haemoglobinuria clone, prothrombin mutation G20210A, factor V Leiden mutation, JAK2 [V617F] gene and calreticulin) was normal.
(A and B) Abdominal CT with contrast showing filling defect in the main portal vein and its branches, predominantly in the left portal branch, in the portal-splenic-mesenteric axis, compatible with partial thrombosis of portal vein and main branches. (C and D) Repeat abdominal CT at six months showing complete recanalisation of the main portal vein, branches and the portal-splenic-mesenteric axis.
Study of chronic liver disease was negative (transferrin saturation 22%, ferritin 492mg/dl, ceruloplasmin 23.6mg/dl, alpha-1-antitrypsin 156mg/dl, TSH 3.54mIU/l, HBsAg −ve, HCV −ve, autoimmunity negative) and liver biopsy, which showed signs of simple steatosis, ruling out cirrhosis. Endoscopy ruled out oesophageal varices.
Chromosomal analysis performed to investigate the azoospermia and testicular atrophy was compatible with a karyotype 47,XXY, with a hormonal profile consistent with hypergonadotropic hypogonadism (LH 14.77IU/ml, FSH 30IU/l and testosterone 74.1ng/dl). The patient was diagnosed with Klinefelter syndrome (KS) and started on treatment with topical testosterone.
In view of the episodes of rectorrhagia, he was treated with subcutaneous enoxaparin 100mg/day. As his clinical and radiological progress were good, it was decided to maintain the same dose for six months.1
KS is the most common disorder of the sex chromosomes (47,XXY or mosaic). Phenotypically they have testicular atrophy, gynaecomastia and hypergonadotropic hypogonadism. The estimated prevalence is 153 per 100,000 males.3 Due to the wide phenotypic variation, only 25% of the total are diagnosed, some during a sterility study.4
Individuals with KS have an increased risk of venous thromboembolism (VTE), which may be explained by the androgen deficiency that increases the levels of plasminogen activator inhibitor-1 (PAI-1), causing hypofibrinolysis, platelet hyperaggregation, and an increase in factor VIII activity.5
The risk of developing venous thrombosis (VT) or pulmonary embolism (PE) is 5–20 times higher than that of the general population.6 A Swedish retrospective study, with 1085 patients diagnosed with KS, showed that the cumulative incidence of VTE was 8.6% at the age of 50 and 20.8% at the age of 70, being comparable to hereditary thrombophilias.7 However, the risk of PVT or mesenteric vein thrombosis (MVT) has not been determined.
The first case of MVT in a patient with KS was published in 1988. In that case, MVT manifested as rectal bleeding and intestinal infarction, requiring resection. Anticoagulation was started postoperatively, but the duration was not specified. Aetiological study showed only a slight decrease in protein C levels. At follow-up, there was no evidence of re-thrombosis.8
Two cases of PVT and MVT associated with KS were later published in which no local or systemic factors for thrombosis were found. Outcomes were good in both cases, with patency of the PVT and MVT partially restored, probably due to the early administration of anticoagulation.9,10
In conclusion, we have presented the case of a patient with a recent diagnosis of KS in whom no local or systemic prothrombotic factor was identified who developed portal-splenic-mesenteric venous thrombosis. After treatment with low-molecular-weight heparin for six months, he was found to have full recanalisation, with no evidence of new thrombosis at his 12-month follow-up. The optimal duration of anticoagulant treatment in PVT has not been fully established. However, it is recommended that treatment should be maintained for at least six months, and that permanent anticoagulation be considered in patients with an underlying prothrombotic factor.1 As a high prevalence of thromboembolic events has been reported in KS, the need for long-term or even permanent anticoagulation should be considered in these patients.
Please cite this article as: Larraín M, Castillo-Regalado E, Puig-Jove C, Sala M, Masnou H. Trombosis venosa portal y del eje esplenomesentérico en un paciente con síndrome de Klinefelter. Gastroenterol Hepatol. 2018;41:563–565.