The gastrointestinal tract is the site of 70% of synchronous cancers. Simultaneous occurrence of gastric carcinoma and lymphoma are relatively common, but the synchronous presence of triple primary cancer occurring in the stomach is exceptionally rare.1
Only a few cases of triple synchronous gastric malignancies have been reported in the literature.2,3 Here we present an exceptional case of a male with Helicobacter pylori (HP) infection and incomplete intestinal metaplasia (IIM) who developed three synchronous gastric tumors: signet ring cell carcinoma, MALT lymphoma and large cell neuroendocrine carcinoma (NEC).
In November 2011, a 48-year-old Caucasian man was admitted to our hospital with hematemesis. The patient was heavy smoker and was not taking gastro-erosive medications. Routine laboratory tests showed a normocytic and normochromic anemia. Fiberoptic endoscopy revealed subcardial mucosa laceration, bleeding signs, erythematous mucosa in gastric body with inflammation and edematous duodenal bulb without peptic ulcer. Biopsy from antrum revealed inflammation compatible with chronic gastritis and intestinal metaplasia. Urease test resulted positive.
Eleven months later after HP treatment failure to OCA-10 and OLA-10, subsequent gastroscopy demonstrated gastric wall thickening with pseudonodular appearance, antrum mucosa with mixed white and erythematous areas and protruded spots. Biopsies from body and antrum showed signet-ring carcinoma, atrophic gastritis, IMM and HP infection.
Computerized tomography (CT) scanning showed thickened gastric folds, pulmonary infiltration in left upper lobe, lingular atelectasis, 2.5cm pulmonary nodule in lower lobe, focal hepatic lesions and multiple adenopathies. Laparoscopic surgery did not show serous inflammation but confirmed lymphadenopathy greater than 1cm previously observed in the CT scan. Total gastrectomy was performed with omentectomy and D2 lymphadenectomy. R0 resection with lymph node stations 1 to 11 removed and esophagus-jejunal T-L anastomosis, L-L jejunum-jejunum Roux en-Y anastomosis and closure of duodenal stump was carried out.
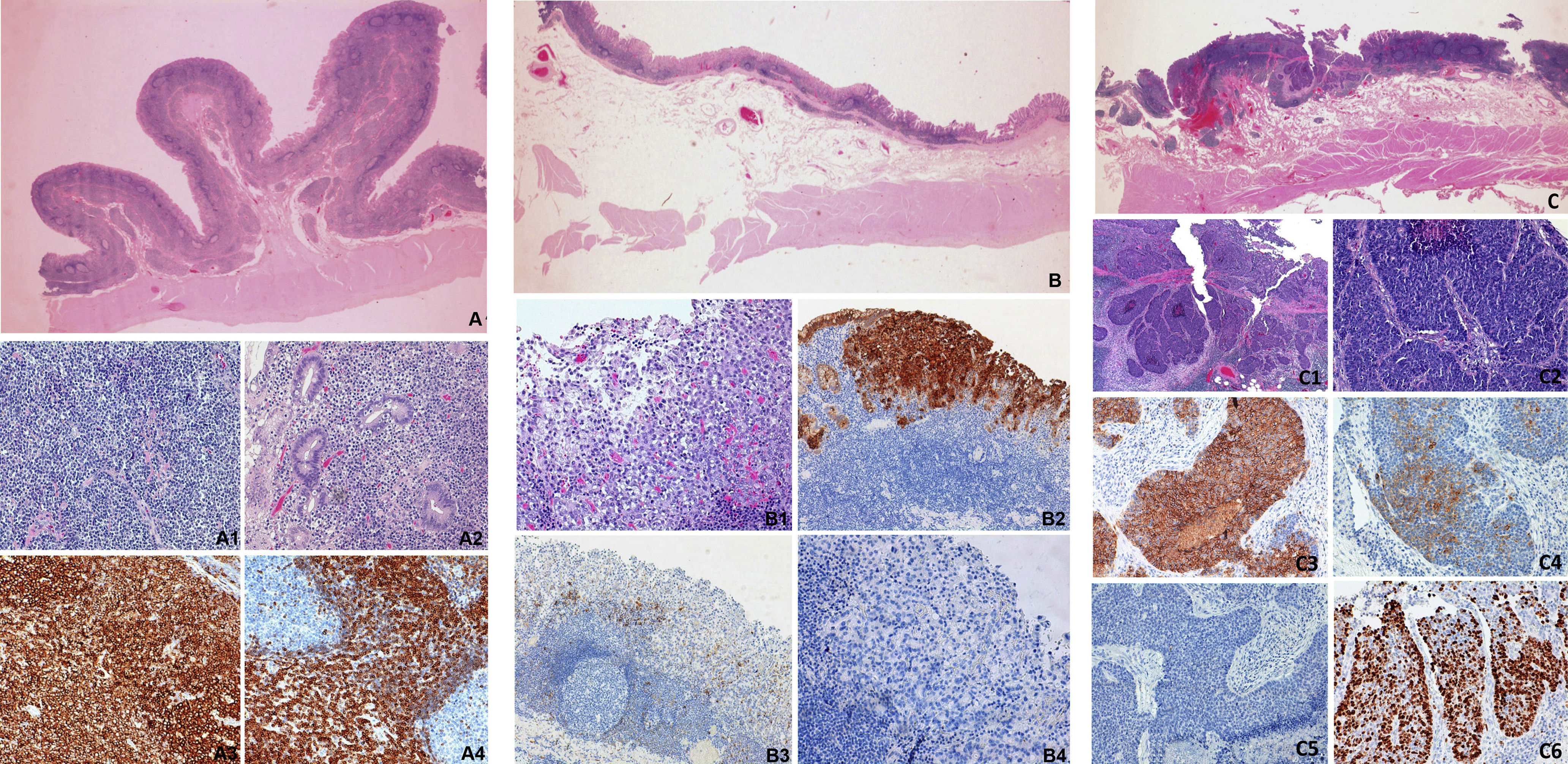
The internal surface of surgical specimen showed enlarged mucosal folds in the body of the stomach. Affecting the mucosa and submucosa, there was an infiltrate of intermediate size lymphocytes with a small nucleoli and scanty cytoplasm. Lymphoepithelial lesions and lymphoid follicles were observed. The immunophenotype was positive for CD20 and BCL-2 and negative for CD10, cyclin D1, BCL-6, CD-23 and CD-5 (Fig. 1). The transitional area between body and antrum showed a proliferation of epithelial cells with a diffuse or cord growth and signet ring cells. Although this tumor involved mainly the mucosa, isolated cells were also identified in the submucosa. Cells were immunoreactive for CKAE1/AE3, EMA and CEA. No expression of E-cadherin, CD56, NSE, chromogranin and synaptophysin was observed. A third tumor was diagnosed in the gastrectomy specimen. Between fundus and body, in mucosa and submucosa, a proliferation of homogeneous epithelial cells, with a nested growth and focal necrosis was observed. Mitotic index was 14 mitosis/10 HPF and the proliferation index (Ki67): >20%. The cells were immunoreactive cells for CKAE1/AE3, EMA, E-cadherin and CD56 and expressed chromogranin (30% of the cells) and synaptophysin (10% of the cells). No expression of NSE and CEA observed.
Immunostaing of triple synchronous gastric tumors. A. Panoramic view-slide with enlargement of the mucosal folds. Lymphoid follicles are observed. Mucosa and submucosa involvement. A1: Diffuse infiltrate of intermediate size lymphocytes with a small nucleoli and scanty cytoplasm. A2: Lymphoepithelial lesion. A3: Immunohistochemistry for CD20. A4: Immunohistochemistry for Bcl-2. B: Panoramic view-slide with adenocarcinoma. B1: Proliferation of epithelial cells with a diffuse growth and signet ring cells. B2: Immunohistochemistry for CEA. B3: Immunohistochemistry for CD56, absence of expression in tumor cells. B4: Immunohistochemistry synaptophysin, absence of expression.
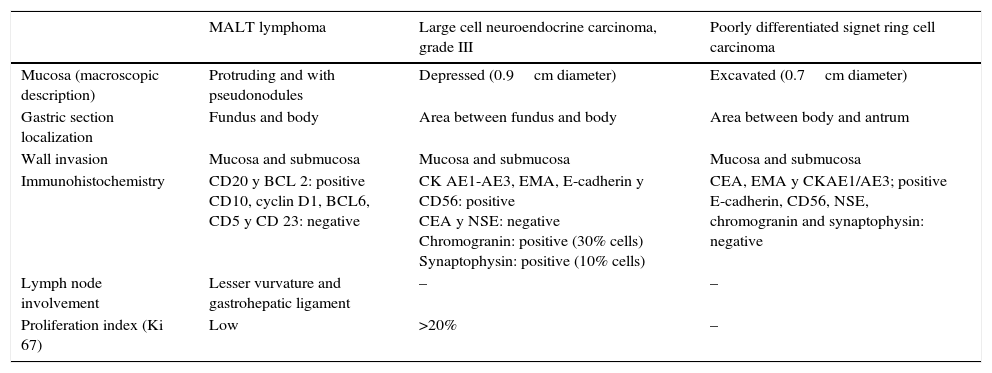
Based on histopathological and immunohistochemistry findings, a diagnosis of triple composite tumor of stomach: MALT lymphoma, NEC and diffuse carcinoma was made (Table 1).
Pathological characteristics of the triple synchronous gastric tumors.
| MALT lymphoma | Large cell neuroendocrine carcinoma, grade III | Poorly differentiated signet ring cell carcinoma | |
|---|---|---|---|
| Mucosa (macroscopic description) | Protruding and with pseudonodules | Depressed (0.9cm diameter) | Excavated (0.7cm diameter) |
| Gastric section localization | Fundus and body | Area between fundus and body | Area between body and antrum |
| Wall invasion | Mucosa and submucosa | Mucosa and submucosa | Mucosa and submucosa |
| Immunohistochemistry | CD20 y BCL 2: positive CD10, cyclin D1, BCL6, CD5 y CD 23: negative | CK AE1-AE3, EMA, E-cadherin y CD56: positive CEA y NSE: negative Chromogranin: positive (30% cells) Synaptophysin: positive (10% cells) | CEA, EMA y CKAE1/AE3; positive E-cadherin, CD56, NSE, chromogranin and synaptophysin: negative |
| Lymph node involvement | Lesser vurvature and gastrohepatic ligament | – | – |
| Proliferation index (Ki 67) | Low | >20% | – |
No metastasis of carcinoma was observed in lymph nodes but some of lymph nodes of lesser curvature and gastrohepatic ligament were affected by lymphoma. Atrophic gastritis with IMM and HP were observed in non-tumoral mucosa.
Postoperative period went without incidences. Complete CT-scan was performed with bone marrow and myelogram showing no abnormalities. Radiotherapy treatment was given to the patient after surgery. One year later, patient underwent surgery for a 2.4cm tumor in left lung in which pathological findings concluded a marginal MALT lymphoma. Rituximab, bendamustina and filgastrim were administrated and patient achieved remission and he is currently in stable disease.
HP infection is a common carcinogen causative of both gastric carcinoma and MALT lymphoma.4 Sakai et al.5 published a 100% positivity rate of HP infection among 13 reviewed cases of synchronous carcinoma and MALT lymphoma in the stomach. A Spanish multicenter study demonstrated in 2015 that IIM patients possessed a probability of 4.9% to develop gastric adenocarcinoma in a period of 12 years. In 649 individuals with premalignant gastric lesion only 0.15% of them developed a neuroendocrine tumor or MALT lymphoma.6
The most commonly reported double synchronous gastric malignancies include a combination of an carcinoma with stromal tumors,7 neuroendocrine carcinomas8 or lymphomas1,5 being MALT lymphoma the most common.9 A definitive characterization of synchronous gastric cancers requires diligent sampling and comprehensive immunostaining.
In 2014, Michalinos et al.10 reviewed 63 cases of gastric collision with double synchronous tumors. The precise mechanism of this neoplasms coexistence is unclear.
Only two cases of triple synchronous adenocarcinoma, hepatoid carcinoma and large cell NEC of stomach have been published.2,3 Here, we report a case of synchronous adenocarcinoma poorly differentiated with signet ring cell adenocarcinoma, MALT lymphoma and large cell neuroendocrine carcinoma in the stomach.
Our case includes the combination of NEC and MALT lymphoma as a gastric collision tumor. The NEC was focal and smaller than the MALT lymphoma. Moreover, both gastric carcinoma and large cell NEC were early tumors. The synchronous malignancies were associated with gastric preneoplastic lesions in non-tumoral mucosa.
Conflict of interestThe authors declare no conflict of interest.