Faecal immunochemical tests for haemoglobin (FIT), as an adjunct to clinical information, assist in the triage of patients presenting in primary care with lower abdominal symptoms. Controversy remains regarding whether and which qualitative and quantitative FIT can be used, which groups of patients would benefit most from FIT, whether FIT should be done in primary and/or secondary care, and how FIT should be incorporated into diagnostic pathways. Controversy also exists as to the optimum cut-off used for referral for colonoscopy. A single sample of faeces may be sufficient. Reporting of results requires consideration. FIT provide a good rule in test for colorectal cancer and a good rule out test for significant bowel disease, but robust safety-netting is required for patients with negative results and ongoing symptoms. Risk scoring models have been developed, but their value is unclear as yet. Further evaluation of these topics is required to inform good practice.
Las pruebas inmunoquímicas fecales (PIF) para determinar la hemoglobina, como pruebas complementarias de la información clínica, ayudan a la selección de pacientes que acuden a Atención Primaria con síntomas abdominales inferiores. Sin embargo, continúa la polémica sobre si utilizar PIF y, en ese caso, si utilizar PIF cualitativas o cuantitativas, qué grupos de pacientes se beneficiarían más de las PIF, si las PIF deben realizarse en Atención Primaria o en el especialista, y cómo las PIF deben incorporarse a los protocolos de diagnóstico. También hay polémica sobre el valor de corte óptimo utilizado para la derivación a colonoscopia. Una sola muestra de heces puede ser suficiente. La notificación de los resultados exige análisis. Las PIF son un buen principio en la prueba del cáncer colorrectal y una buena prueba para descartar una enfermedad intestinal importante, pero se necesita una red de protección sólida para los pacientes con resultados negativos y síntomas continuos. Se han elaborado modelos de puntuación de riesgo, pero su valor aún no está claro. Se requiere una evaluación adicional de estos temas para lograr una buena práctica.
Faecal immunochemical tests for haemoglobin (FIT) are now widely used in asymptomatic colorectal (bowel) cancer screening since widely perceived as the best currently available non-invasive approach: participants with positive results are referred for further investigation, usually colonoscopy.1 Possibly because of (a) the positive publicity surrounding such programmes, (b) the information given that participants who experience lower abdominal symptoms between screening episodes should seek medical care and (c) the influence of well-known individuals in the media,2 the demand for colonoscopy has risen further over recent times. In addition, because more bowel disease is found, an increased requirement for colonoscopic surveillance after treatment has occurred, although there are early indications that FIT might be useful in this clinical setting as well as others.3 Further, there have been local, regional and national efforts in many countries encouraging people with abdominal symptoms to seek urgent medical attention in primary care, again leading to further demands on colonoscopy services.4
However, colonoscopy is often a limited resource and, in consequence, it would be of much benefit if a simple, inexpensive investigation would aid in deciding which of the many patients presenting with symptoms, particularly in primary care, would benefit from colonoscopy and which would not. This is particularly germane since, as pointed out some time ago by Jellema et al.5 and very well documented more recently by Vega et al.,6 diagnosis is a challenge, since there are often no specific symptoms and lower abdominal symptoms are very common and mostly related to problems other than significant bowel disease (SBD), which includes colorectal cancer (CRC), advanced adenoma (AA) that are sometimes precursors of CRC, and inflammatory bowel disease (IBD). Indeed, according to the National Institute for Health and Care Excellence (NICE) in England, common symptoms have a positive predictive value (PPV) for CRC of only 3–4%.7 Thankfully, there is ever growing evidence that FIT can be used to assist in the triage of patients presenting with symptoms of lower bowel disease.
FIT in assessment of patients with lower abdominal symptomsThe evidence for the successful application of FIT in assessment of patients presenting in primary care with lower abdominal symptoms, and patients being seen in secondary care clinics after referral, has been very well documented in a number of recent reviews.8–11 Therefore, the fine details of the individual studies will not be repeated in detail in this review. Although it is known that there are a number of real-world pilots, feasibility studies and evaluations of FIT in the assessment of symptomatic patients underway and publications on this topic are in press or in preparation, there appears to have been only one further relevant publication12 since the most recent comprehensive review.11 This study investigated the value of a quantitative FIT in the diagnostic process of CRC and other SBD in individuals presenting with low risk symptoms in general practice, FIT being used as a rule-in test on patients aged ≥30 years with the faecal haemoglobin concentration (f-Hb) cut-off for referral to colonoscopy being 10μg Hb/g faeces: 3462 FIT were performed and 540 (15.6%) had positive results. Of these, 51 (PPV: 9.4%) individuals with a positive FIT result were diagnosed with CRC and 73 (PPV: 13.5%) with other SBD. The false negative test result rate for CRC was < 0.1%. It was concluded that FIT may be used as a supplementary diagnostic test in general practice in the diagnostic process of CRC and other SBD in individuals with low risk of CRC.
Even though it has been documented by NICE,13 a highly respected developer of guidelines, that quantitative FIT are recommended for adoption in primary care to guide referral for suspected CRC in people without rectal bleeding who have unexplained symptoms but do not meet the criteria for a suspected cancer pathway referral outlined in the NICE NG12 guideline,7 and that results should be reported using a f-Hb cut-off of 10μg Hb/g faeces, many controversies still exist: a number of these will be addressed in this review.
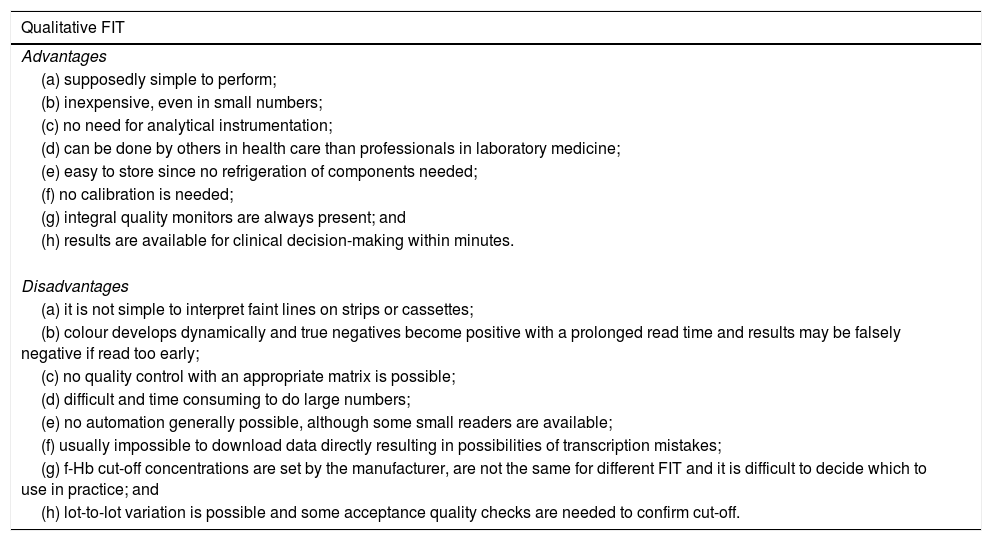
Qualitative or quantitative FITFIT are available in two formats.14 Qualitative FIT give a dichotomous, positive/negative result, usually using lateral-flow immunochromatographic cassettes or strips. Quantitative FIT usually involve automated immunoturbidimetry on small bench-top dedicated analytical systems and provide a numerical estimate of the f-Hb: such examinations can also be performed on larger routine laboratory medicine automated systems. As detailed previously,10,11 both constructs have been used to evaluate the use of FIT in assessment of patients with symptoms. Some of the advantages and disadvantages of qualitative and quantitative FIT are listed in Table 1.
Advantages and disadvantages of qualitative and quantitative faecal immunochemical tests for haemoglobin (FIT).
| Qualitative FIT |
|---|
| Advantages |
| (a) supposedly simple to perform; |
| (b) inexpensive, even in small numbers; |
| (c) no need for analytical instrumentation; |
| (d) can be done by others in health care than professionals in laboratory medicine; |
| (e) easy to store since no refrigeration of components needed; |
| (f) no calibration is needed; |
| (g) integral quality monitors are always present; and |
| (h) results are available for clinical decision-making within minutes. |
| Disadvantages |
| (a) it is not simple to interpret faint lines on strips or cassettes; |
| (b) colour develops dynamically and true negatives become positive with a prolonged read time and results may be falsely negative if read too early; |
| (c) no quality control with an appropriate matrix is possible; |
| (d) difficult and time consuming to do large numbers; |
| (e) no automation generally possible, although some small readers are available; |
| (f) usually impossible to download data directly resulting in possibilities of transcription mistakes; |
| (g) f-Hb cut-off concentrations are set by the manufacturer, are not the same for different FIT and it is difficult to decide which to use in practice; and |
| (h) lot-to-lot variation is possible and some acceptance quality checks are needed to confirm cut-off. |
| Quantitative FIT |
|---|
| Advantages |
| (a) high quality analyses with good reproducibility; |
| (b) easy to monitor quality using total quality management techniques to guarantee standards through International Standardisation Organisation (ISO) 15198 accreditation; |
| (c) high throughput of samples may be possible; |
| (d) no visual interpretation of results; |
| (e) download of data into LIS via middleware may be possible, eliminating transcription errors and facilitating record keeping; and |
| (f) linkage with other data, for example, age and sex, may be possible and may be important for the future for risk scoring or monitoring; and |
| (g) the cut-off f-Hb for referral for colonoscopy can be set locally. |
| Disadvantages |
| (a) expensive if few FIT analyses done; |
| (b) need for instrumentation, installation, training, etc.; |
| (c) the need to evaluate or validate for laboratory medicine accreditation systems and then prepare complex documentation; |
| (d) difficult to decide which FIT analytical system to use since many now available; |
| (e) only done by trained professionals in laboratory medicine; |
| (f) refrigeration required for latex reagent and quality control materials and calibrators; and |
| (g) issues around stability of haemoglobin in specimen collection devices. |
Although there are a large number of qualitative15 and qualitative16 FIT available, it could be argued that the available evidence suggests that both qualitative and quantitative FIT appear to give somewhat similar clinical outcomes10 and both could be used in assessment of patients presenting with lower abdominal symptoms if the disadvantages of the two rather different approaches were carefully kept in mind. However, it must be noted that the data available to support the use of FIT in this clinical setting was generated with only very few of the qualitative15 and quantitative16 FIT available. There are more data on quantitative than qualitative FIT and only the former were recommended by NICE.13 In consequence, it has been advocated that assessment of the benefits and harms of qualitative FIT being done by people in their own homes should be investigated,17 as should the use in general practice and in secondary healthcare settings, particularly in gastroenterology and other clinics evaluating patients before colonoscopy.10,11
It is important to note that the numerical results generated using different FIT may not be the same. Three quantitative FIT systems were recommended in NICE DG30, namely the OC-Sensor (Eiken Chemical Co. Ltd., Tokyo, Japan), the HM-JACKarc (Kyowa Medex Co., Ltd., Tokyo, Japan) and FOB-Gold (Sentinel Diagnostics, Milan, Italy)13; however, the evidence gathered to support the recommendation of these three FIT systems clearly does show differences in the clinical outcomes obtained. The main reason for the differences is probably that polyclonal antibodies are used, which may react differently to the spectra of intact haemoglobin (Hb) and early degradation products present in faecal samples collected for analysis. In addition, the analytical performance characteristics of the FIT systems show a number of marked differences, for example, the analytical range, the limit of detection, the lowest f-Hb that can be reliably distinguished from a sample with no f-Hb, and the limit of quantitation, the lowest f-Hb that can be reliably measured, differ between these three quantitative FIT systems.18 In addition, there are a number of pre-analytical and analytical aspects which differ between FIT and these include lack of harmonisation of the specimen collection devices, the intrinsic heterogeneity and variable consistency of faecal samples and the effect of these variables on faecal collection, the different recommended techniques for collection of faeces and the fact that no primary reference material or method is currently available to standardise FIT.19 Further, a very relevant concern is the transferability of already published data over time and geography: manufacturers of FIT continually evolve their products and, in consequence, outcomes may not be comparable over time. An example of change over time is that two of the quantitative FIT recommend by NICE13 have had improvements made to their buffers, supposedly to increase the stability of any haemoglobin present prior to analysis.20,21
Although there are a number of studies comparing different FIT in asymptomatic population-based screening applying different strategies,22 which do demonstrate differences between systems when the same cut-off f-Hb is used for referral to colonoscopy, which are minimised if the same positivity is used,23–25 there seem no head to head comparisons of FIT in assessment of patients with symptoms. This would be of considerable interest, since the same FIT are used in screening and assessment of the symptomatic and it has been amply demonstrated15,16 that there are many differences between available FIT used in screening.
Deciding which patients should undertake a FITThe clinical outcome characteristics will depend very much on the type of patients who have provided faecal samples for FIT analysis. The spectra of patients examined have varied from study to study.10,11 NICE DG30 specifically states,13 as detailed above, that FIT are to be applied in what might be termed low risk patients and those patients who have rectal bleeding and meet the criteria for a suspected cancer pathway referral outlined in NICE NG127 should be referred for further investigation without FIT. However, most evaluations have assessed the value of FIT in quite mixed populations including those at high risk of CRC and even those undergoing surveillance for previous disease.26 In addition, most studies, except for that of Mowat et al.27 and Juul et al.12 have not evaluated the use of FIT in primary care, but have examined patients who were already referred for colonoscopy through a variety of clinical pathways with different criteria for referral. Further studies on the routine application of FIT in primary care are urgently required, since this seems to be the most appropriate sector in which FIT should be requested. However, studies on the appropriate uses of FIT in secondary care, such as in gastroenterology clinics, would also be of considerable interest.
In addition, there has been some controversy about how FIT should be integrated into diagnostic pathways. One study, following on directly from an evaluation of point of care (POC) FIT and calprotectin in patients with symptoms,28 developed a multivariable diagnostic model for SBD with routine clinical information and subsequently extended this with faecal calprotectin testing and/or qualitative POC FIT.29 The results were said to underscore that a positive f-Hb result already implies the need for referral and that clinical data do not add much. However, it was suggested that these data are informative when the f-Hb result is negative. It was concluded that a diagnostic strategy with routine clinical data and f-Hb alone may safely rule out SBD and prevent unnecessary endoscopy referral in approximately one-third of patients. A contrasting editorial suggested that a single quantitative f-Hb result, without any clinical information, could be sufficient to decide whom to refer for colonoscopy and, because of the significant overlap of symptoms in those with and without SBD, could be the primary investigation performed.30 This thesis has been supported in a recent study which compared the utility of FIT as the initial investigation with the original 2015 NICE NG12 symptom based guidelines.31 Data from three studies done in Scotland were included and overall diagnostic accuracy was also estimated by the area under the receiver operating characteristic (ROC) curve (AUC). The AUC for CRC was 0.85 for FIT versus 0.65 for NG12 and, for SBD, the AUC was 0.73 for FIT versus 0.56 for NG12. It was concluded that f-Hb provided a good rule-out test for SBD and had significantly higher overall diagnostic accuracy than the 2015 NG12 guidelines.7
Other approaches are possible10 and, according to a recent review on setting up a service for FIT for assessment of symptomatic patients, there appears to be no “best practice” that can be detailed at this particular time19: reports on the results of the use of FIT for the routine assessment of patients in primary care are awaited with interest, but informal current consensus seems to be that the f-Hb found should be taken into account along with symptoms and clinical findings, particularly chronic diarrhoea and the presence of an abdominal mass, and the results of the full blood count, particularly the detection of anaemia, as recently advocated by Hogberg et al.32
Selecting the cut-off faecal haemoglobin concentration (f-Hb) used for referral for colonoscopyA number of the evaluations of the use of quantitative FIT in assessment of the symptomatic have explored the relationship between f-Hb and clinical outcomes. Since it is very well documented that f-Hb is directly related to the severity of colorectal disease, and as confirmed recently,33 it is not surprising that, as the f-Hb cut-off is lowered, the sensitivity increases and the specificity decreases. A good example is provided in a supplementary table in the study of Rodríguez-Alonso et al.,34 where, at f-Hb cut-offs > 0, ≥10, ≥15 and ≥20μg Hb/g faeces, sensitivity for CRC was 100, 96.7, 96.7 and 93.3% with specificity of 43.3, 79.8, 83.1 and 86.1% and, for advanced neoplasia (AN: CRC + AA), sensitivity was 81.2, 61.7, 57.1 and 53.4%, while specificity was 45.5, 83.4, 86.6 and 89.4%. It is important to note that, at 20μg Hb/g faeces, a commonly used cut-off in asymptomatic population-based screening, and as used by Cubiella et al.,35 a small number of cases of CRC are missed. This has also been shown for AA and IBD at f-Hb cut-offs of 10μg Hb/g faeces, as recommended by McDonald et al.36 and Godber et al.37 This missing of cases of SBD was also found by Mowat et al.27 with a f-Hb cut-off of 10μg Hb/g faeces, but who also investigated “detectable” f-Hb as a cut-off (defined as >0μg Hb/g faeces) achieving sensitivities of 100, 82.5 and 85.3% for CRC, AA and IBD, respectively. Similarly, Widlak et al. stated that an undetectable FIT haemoglobin is sufficiently sensitive to exclude CRC, but they defined “undetectable” as f-Hb <7μg Hb/g faeces, the LoQ of the FIT system used.38
The publications on FIT in the assessment of patients with symptoms clearly demonstrate the current controversy of which f-Hb cut-off to use and also the dilemma of how to report the results of FIT analyses. This has been addressed in detail recently39 and a series of proposals made including the following40:
- •
f-Hb concentrations should not be reported to more significant figures than whole integers,
- •
f-Hb concentrations less than the limit of detection (LoD) of the FIT analytical system should be termed “not detected” or “undetectable”,
- •
for academic use: f-Hb greater than the LoD could advantageously be documented,
- •
for routine clinical use: numerical f-Hb should be reported only when greater than the limit of quantitation (LoQ): f-Hb less than the LoQ (x) should be reported as <x μg Hb/g faeces and
- •
if a more sophisticated reporting system is required, one option is to report:
- ∘
f-Hb<LoD=f-Hb not detected
- ∘
LoD<f-Hb<LoQ=f-Hb detected
- ∘
f-Hb≥LoQ=report the found f-Hb
Adherence to these proposals would result in harmonisation of the reporting of f-Hb data, which should facilitate understanding and transferability of information across geography and time.
A further controversy is whether the high sensitivity makes FIT a good rule-in test for CRC or the high negative predictive value (NPV) shown in many studies on use of FIT in assessment of the symptomatic10,11 demonstrates that FIT provides a good rule out investigation for SBD. In reality, f-Hb in patients presenting in primary carer with lower abdominal symptoms could be considered as a continuous variable. The most important use in colonoscopy constrained countries is likely to be to stop patients with vague symptoms and unlikely to have SBD being referred for colonoscopy. If the f-Hb is lower than the selected f-Hb cut-off and if the patient does not have what are sometimes termed red flag symptoms, then the risk of SBD is small: however, this does not simply mean informing the patient nothing is wrong. Many lower abdominal symptoms are transient, so it might be satisfactory to leave these patients without any immediate further investigation but, for others who continue to have symptoms, it is obligatory to have robust safety-netting procedures in place as recently described in a review of FIT in patients with symptoms,41 including watching and waiting, referral to gastroenterology in secondary care, and perhaps a repeat FIT, although there is no evidence to date that this is useful. This is important since, as discussed above, a few cases of CRC may be missed in addition to a few more cases of AA and IBD. Moreover, since it is well documented that f-Hb is related to disease severity,33 the higher the f-Hb, the greater the risk of SBD. In consequence, those with very high f-Hb might benefit from more rapid referral to colonoscopy than those who have slightly elevated f-Hb.
How many faecal samples should be taken for FIT?It is dogma that some neoplastic lesions in the colon bleed intermittently and so it is also dogma that more than one faecal sample should be collected. Although there is considerable literature on one versus two samples in asymptomatic population screening, the literature on the effect of number of FIT samples in assessment of patients with symptoms is sparse. A recent study assessed the use of three samples in patients with CRC and adenomas with high grade dysplasia (HGD) that initially presented with symptoms to primary care and completed FIT.42 Of 195 patients, 160 delivered three FIT. Using the 139 cases in which at least one sample was positive, the likelihood of detecting a positive sample upon analysis of only one of the three samples was 0.91, indicating that 13 positive cases may have been missed. It was concluded that use of one sample instead of three samples may result in missing about 10% of symptomatic CRC and adenomas with HGD. Unfortunately, this study was done with a visually read qualitative FIT and dipstick test, with f-Hb cut-off of 25–50μg Hb/g faeces, rather higher than f-Hb cut-offs used in the published studies using quantitative FIT. It may be unsurprising, therefore, that cases of SBD were missed. Auge et al.26 examined the clinical utility of one versus two samples for FIT samples in the detection of advanced colorectal neoplasia (ACRN: CRC + AA) in symptomatic patients using a quantitative FIT. It was found that the diagnostic yield, when two samples for FIT were collected (using f-Hb cut-off of 20μg Hb/g faeces), could be achieved with one sample, albeit using a lower f-Hb cut-off (10μg Hb/g faeces). With a different FIT analytical system, using two samples for each patient and choosing the highest result, the sensitivity for ACRN was 40.0%, with a specificity of 88.6%, and a similar diagnostic yield was again obtained using only one sample and decreasing the f-Hb cut-off.43 Moreover, when one sample and a 10μg Hb/g faeces cut-off was used, it was possible to rule out the majority of malignant lesions. Based on this small amount of evidence, since collecting multiple samples involves more funding and effort and might decrease the acceptability of the test for patients, it is likely that one sample combined with a low f-Hb cut-off would provide a cost-effective and clinically efficient service for patients presenting in primary care.
FIT alone or in combination with other variablesRisk prediction models which take both symptoms and multiple risk factors into account might have potential to improve timely diagnosis of SBD. Williams et al.44 have systematically identified and compared the performance of models that predict the risk of primary CRC among symptomatic individuals: it was concluded that good approaches had been generated in both primary and secondary care populations. Most were said to contain variables that were easily obtainable in a single consultation. However, few of the models actually include f-Hb in the algorithm. Since it is well documented that f-Hb increase with age and is higher in men than women,45 although the actual f-Hb vary from country to country,46 Rodríguez-Alonso et al.34 created a simple risk score for AN based upon age, gender and f-Hb. The points attributed to each risk factor were weighted according to their respective coefficients in a multiple logistic regression model and the score had a range of 0–11 points based on the sum of the points in the individual patient. A simple chart to calculate the sum was published. In the population studied, if a risk score ≥ 5 was considered as the referral criterion for colonoscopy, only 36.4% of would be referred; no cases of CRC and only 5% of AA were undetected. A more complex approach was developed by Cubiella et al.47 using a multivariate logistic regression analysis to develop the model, with diagnostic accuracy of CRC detection as the main outcome: 1572 symptomatic patients were included in the derivation cohort and 1481 in the validation cohorts. The final prediction model included 11 variables: age, male sex, f-Hb ≥20μg Hb/g faeces, blood Hb <10g/dl, blood haemoglobin 10–12g/dl, carcinoembryonic antigen ≥3ng/ml, aspirin use, previous colonoscopy, presence of a rectal mass, benign anorectal lesion, rectal bleeding, and change in bowel habit. The AUC was 0.92. On the basis of the thresholds with 90% and 99% clinical sensitivity, the derivation cohort was divided into high, intermediate and low risk groups for CRC with PPV of 40.7, 4.4 and 0.2% respectively. It was concluded that the COLONPREDICT strategy developed was a highly accurate prediction model for CRC detection. Because of the complexity of this model, Cubiella et al. went on to develop the faecal haemoglobin concentration, age and sex test (FAST) score with data from five diagnostic test accuracy studies that evaluated quantitative FIT in symptomatic patients referred for colonoscopy48: 1572 and 3976 patients were examined in derivation and validation cohorts, respectively. The AUC for CRC detection was 0.88 and 0.91 in the derivation and validation cohorts. The FAST score was said to an easy to calculate prediction tool, highly accurate for CRC detection in symptomatic patients. Other variables affect f-Hb, such as deprivation,49,50 and it may be that these should be examined for incorporation into future risk scoring strategies. However, it is clear that further research is needed to assess the clinical utility of these risk scoring strategies and other complex approaches before they can be incorporated into routine practice.
ConclusionsAlthough there is much evidence from research studies that FIT, as an adjunct to clinical information and full blood count, can provide a very useful tool to assist with the triage of patients presenting in primary care with lower abdominal symptoms, there remain a number of issues which can only be resolved through further study and evaluation as FIT become more and more applied in real-world clinical practice.51 There remains some controversy regarding whether and which qualitative and quantitative FIT can be applied in this clinical setting, which particular groups of patients would benefit from FIT, and whether the investigation should be done in primary and/or secondary care settings and how it should be incorporated into diagnostic pathways. Controversy also exists as to the optimum f-Hb to be used for referral for colonoscopy, although it is known that sensitivity will increase and specificity decrease as the cut-off f-Hb is lowered. Harmonisation of approaches to defining the detectability characteristics of FIT analytical methods is required as is standardisation of the reporting of results. FIT, with high sensitivity, provide a good rule in test for CRC and, with high NPV, a good rule out test for SBD: however, no test is perfect and, irrespective of the f-Hb cut-off applied, a small number of CRC will be missed as will rather more AA and IBD: thus, robust safety-netting is required for patients who have negative FIT results but continue to experience symptoms. Some evidence exists that a single sample of faeces is sufficient in assessment of patients with symptoms. Risk scoring models incorporating f-Hb and other variables, particularly age and sex, have been developed, but further research is required as to their value in clinical practice. Further simple research studies on the value of FIT in assessment of patients with symptoms would seem somewhat redundant. What is required now are reports on the evaluation of the routine use of FIT in assessment of patients with symptoms, particularly on the controversial aspects which still remain as outlined here, and the many other challenges not discussed here, but explicitly addressed in previous reviews, including many analytical aspects concerning the current analysis of f-Hb.10,11,19
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestCGF undertakes consultancy with Kyowa Medex Co., Ltd, Tokyo, Japan, and receives support to attend conferences from Alpha Labs Ltd, Eastleigh, Hants, UK.