Intestinal failure is a rare pathology wich requires knowledge and highly specialised multidisciplinary management. Crohn's disease (CD) being one of the most frequent causes in adults.
Material and methodsSurvey format study carried out within the GETECCU group, included closed format questions about the diagnosis, management and current knowledge of intestinal failure in CD.
Results49 doctors participated, belonging to different Spanish centres (19 cities).
It was considered that a patient suffered from intestinal failure, in 67.3% (33/49 surveyed) when there was a disorder malabsorptive associated regardless of the intestinal length resected, with surgeries resective ileal repeated (40.8%, 20/49), the most frequent cause.
It highlights frequent ignorance about the pathology (24.5%) did not know if there were patients in their centre and also 40% did not know the pharmacological treatment.
A total of 228 patients were registered for follow-up due to intestinal failure of any aetiology, 89 patients (39.5%) were identified with CD.
Regarding the therapeutic management of patients with CD and intestinal failure (72.5%) were receiving total parenteral nutrition (NTP) and 24 patients (27%) with teduglitide. Regarding the response to the drug; 37.5% had no response to teduglutide, 37.5% partial response (reduce NTP) and 25% good response (withdrawal of home NTP).
In questions related to knowledge about intestinal failure, it was considered limited (53.1%) or very limited (12.2%) by the surveyed.
ConclusionIt is necessary to carry out a combined management of intestinal failure and CD in the context of a multidisciplinary approach.
El fracaso intestinal es una patología poco frecuente en nuestro medio, pero que requiere de conocimientos y manejo multidisciplinar altamente especializado, siendo la enfermedad de Crohn una de las causas más frecuentes en el adulto.
Material y metodosEstudio formato encuesta realizado en el seno de GETECCU, onsta de preguntas de formato cerrado sobre el diagnostico, manejo y conocimiento actual del fracaso intestinal en EC.
ResultadosParticiparon 49 médicos, pertenecientes a distintos centros españoles (19 provincias). Se consideró que un paciente sufría un fracaso intestinal, en el 67,3% (33/49 encuestados) cuando existía un trastorno malabsortivo asociado independientemente de la longitud intestinal resecada, siendo las cirugías resectivas ileales repetidas (40,8%, 20/49), la causa más frecuente.
Destaca frecuente desconocimiento sobre la patología: (24,5%) no sabían determinar si existían pacientes en su centro y un 40% desconocía el tratamiento farmacológico.
En total se registraron 228 pacientes en seguimiento por fracaso intestinal de cualquier etiología, se identificaron 89 pacientes (39,5%) en los que la causa era la EC.
Respecto al manejo terapéutico de los pacientes con EC y fallo intestinal (72,5%) se encontraba con nutrición parenteral domiciliaria (NTP) y 24 pacientes (27%) con teduglutida. El 37,5% no tuvo respuesta a teduglutida, el 37,5% respuesta parcial (disminuir NTP) y el 25% buena respuesta (retirada NTP domiciliaria).
En las cuestiones relativas a los conocimientos sobre el fracaso intestinal, se consideró limitado (53,1%) o muy limitado (12,2%).
ConclusionEs necesario realizar un manejo combinado del fracaso intestinal y la EC en el contexto del abordaje multidisciplinar.
Short bowel syndrome was initially defined as a disorder occurring in patients with insufficient length of bowel to enable adequate absorption of nutrients and/or fluids and electrolytes. However, it is now generally defined in anatomical terms, referring to patients who have undergone one or multiple surgical resections resulting in a remaining small bowel shorter than 200 cm (the length of intestine necessary to maintain nutritional autonomy varies).1
A broader concept based on functional criteria is currently used, that of intestinal failure.2 This includes patients with short bowel criteria and those with other causes of intestinal malabsorption. Intestinal failure is therefore defined as situations where, as a result of surgical resection, congenital defect or disease-related loss of absorption, intravenous supplementation is required to maintain optimal macronutrient, micronutrient and fluid and electrolyte balances.2,3
The actual prevalence of chronic intestinal failure in our setting is variable, although some European studies5 put it in the range of 5–20/106 population (including patients with parenteral nutrition beyond 90 days). However, the incidence of short bowel syndrome (mainly that not requiring prolonged parenteral nutrition) is not clearly established, probably because of the variability in outcomes and even in the definition.
In adults, the most common cause is short bowel syndrome related to extensive surgical resections resulting from mesenteric ischaemia, Crohn's disease (CD) or mesenteric (desmoid) tumours. In children, there can also be other causes, such as motor disorders (for example Hirschsprung's disease) or congenital disorders of the intestinal epithelium.3,4,6
It is estimated that CD may be the cause of around 5% of cases of intestinal failure, as the result of extensive or multiple bowel resections.7,8 However, the published series are old.9,10 These days, resection surgery is more conservative and less frequent in these patients (due to better clinical control of the disease and drug development), so we might expect short bowel syndrome to be less common.
A recent review11 established that the incidence of intestinal failure in patients with CD is 0.8% at 5 years, 3.6% at 10 years and 8.5% at 20 years (with a mean of 3.3 bowel resections among the patients included), and that it could affect up to a third of patients who have several bowel resection operations.
The aim of treatment in patients with intestinal failure is ultimately to help them achieve an adaptive mechanism through an intestinal rehabilitation programme.
Among the pharmacological measures available are teduglutide, a human glucagon-like peptide-2 (GLP-2) analogue, which acts as a specific trophic therapy,12–14 and which has proven to be a useful and safe treatment in this scenario, even in patients in whom the cause of the intestinal failure is CD.14
The aim of this study was to find out how patients with intestinal failure are managed in different hospitals in Spain, although in limited form, referring only to patients in whom the cause of the malabsorptive syndrome is CD. There is also a lack of quality and up-to-date scientific evidence on the actual prevalence of CD-related intestinal failure in our setting in the context of the use of biological drugs and close monitoring strategies for the disease.
Material and methodsThis was a cross-sectional, multicentre study in survey format.
The preparation of the study protocol and the contents of the survey were assessed and approved by both the Grupo Joven (Young Group; GETECCU members under 40 with an interest in IBD) and the Grupo Español de Trabajo en Enfermedad de Crohn y Colitis Ulcerosa (GETECCU) [Spanish Working Group on Crohn's Disease and Ulcerative Colitis] research area.
The survey consisted of 29 questions (Appendix B annex I, Supplementary material) and was sent out in January 2022 by email to GETECCU members through the technical secretary. Two emails were subsequently sent as reminders and to encourage the participation of the different centres.
The survey was designed with an online format through the platform http://www.surveymonkey.com/, with the results being entered anonymously by the collaborating researchers. The survey asked for data about their workplace and their dedication to inflammatory bowel disease (IBD), in order to have a profile of the participants, with the rest of the questions divided into four sections: diagnosis of intestinal failure (6 questions); prevalence (4 questions); therapeutic management (9 questions); and needs or areas for improvement in this scenario (6 questions).
The statistical analysis was performed from a descriptive analysis of the responses obtained in the survey. Mean and standard deviation were calculated for continuous variables and percentages and 95% confidence intervals for categorical variables. After verifying that the variables had a normal distribution (using the Shapiro-Wilk test), the categorical variables were compared using the χ2 test. A p value <0.05 was considered statistically significant. The analyses were carried out with the Stata® programme for Mac® version 15.
ResultsA total of 49 doctors took part. They were from 29 hospitals in 19 different provinces in Spain. Their mean age was 44.1 (SD: 9.12).
Among those surveyed, 87.7% (43/49) were gastroenterologists with full/part dedication to IBD, 2% (1/49) gastroenterologists without dedication to IBD, 8.2% (4/49) general surgeons and 2% (1/49) were paediatricians.
Most of them worked in tertiary level hospitals (65.3%), with a specialised IBD unit in 85.7% of cases. These units treated more than 1500 patients in 57.1% of the centres (28 hospitals), from 1000–1500 patients in 14.3% (7 hospitals), 500−1000 patients in 24.5% (12 hospitals) and fewer than 500 patients in 4.1% (2 hospitals).
Participants were asked when they considered a patient to be suffering from intestinal failure, with this being for most of them (67.3%, 33/49 respondents) when there was an associated malabsorptive disorder regardless of the length of bowel resected. Other responses to this question, in order of frequency, were: 20.5% (10/49 respondents) when, anatomically, a large segment of the small intestine had been resected (60–75% total length); 10.2% (5/49 respondents) when the remaining bowel is less than 200 cm in length; and 2% (1/49 respondents) only if the patient requires home parenteral nutrition.
The type of surgery respondents considered to be the highest risk for intestinal failure in patients with CD were: repeated ileal resections (40.8%, 20/49); extensive ileal resection (28.6%, 14/49); and jejunal resection surgery (24.5%, 12/49).
When asked how the diagnosis of short bowel and/or intestinal failure was made, the most recurrent response in 57.1% (28/49) was with biochemical/nutritional parameters. Interestingly, in this scenario 26.5% (13/49 respondents) request specific assessment by endocrinology to reach the diagnosis, while 4% (2/49 respondents) make the diagnosis purely from suggestive symptoms.
In response to the question asking how many patients with intestinal failure were currently being followed up at each centre, 12 of the respondents (24.5%) did not know how to find out whether or not there were such patients at their hospital. A total of 228 patients were registered as being under follow-up for intestinal failure of any aetiology, with a median of two patients per hospital (IQR: 1–5 patients).
When asked how many of the cases of intestinal failure were caused by CD, 89 patients (39.5%) under follow-up at all the centres were identified, with a median of two patients per hospital (IQR: 1–3 patients). The median time between the diagnosis of IBD and the development of intestinal failure was 12 years (IQR: 6–20 years).
In patients with CD, the most frequent cause of intestinal failure according to the participants was having undergone multiple resection operations in 73.91% of cases, a single extensive resection with decreased absorptive surface in 6.5%, complications other than Crohn's disease (for example, intestinal ischaemia) in 2.2% and, lastly, uncontrolled luminal activity affecting large sections of the small bowel in 2.2%. We should mention that 15.2% of the respondents reported causes other than those listed above, and none of the respondents stated that enteric fistulas in these patients could have been the main cause of their intestinal failure.
When asked about time of diagnosis, 46.5% (20/49) of the respondents said that the majority of cases had been diagnosed from the year 2000 onwards. Meanwhile, 30.2% (13/49) responded that only 25% of the patients at their hospital had been diagnosed with intestinal failure from 2000 on, 11.6% (5 /49) believed that half of the cases under follow-up at their hospital had, and 11.6% (5/49) less than half.
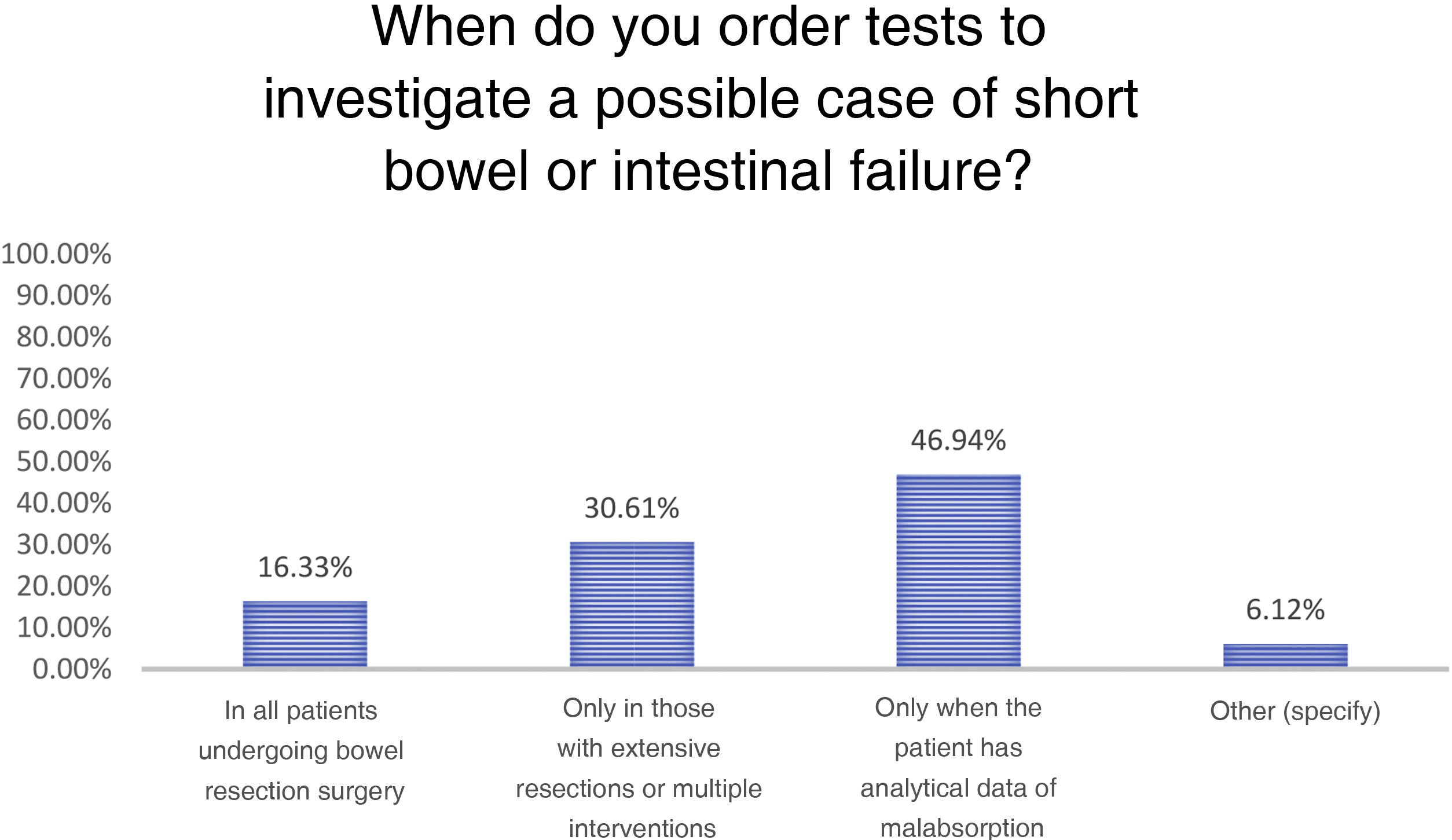
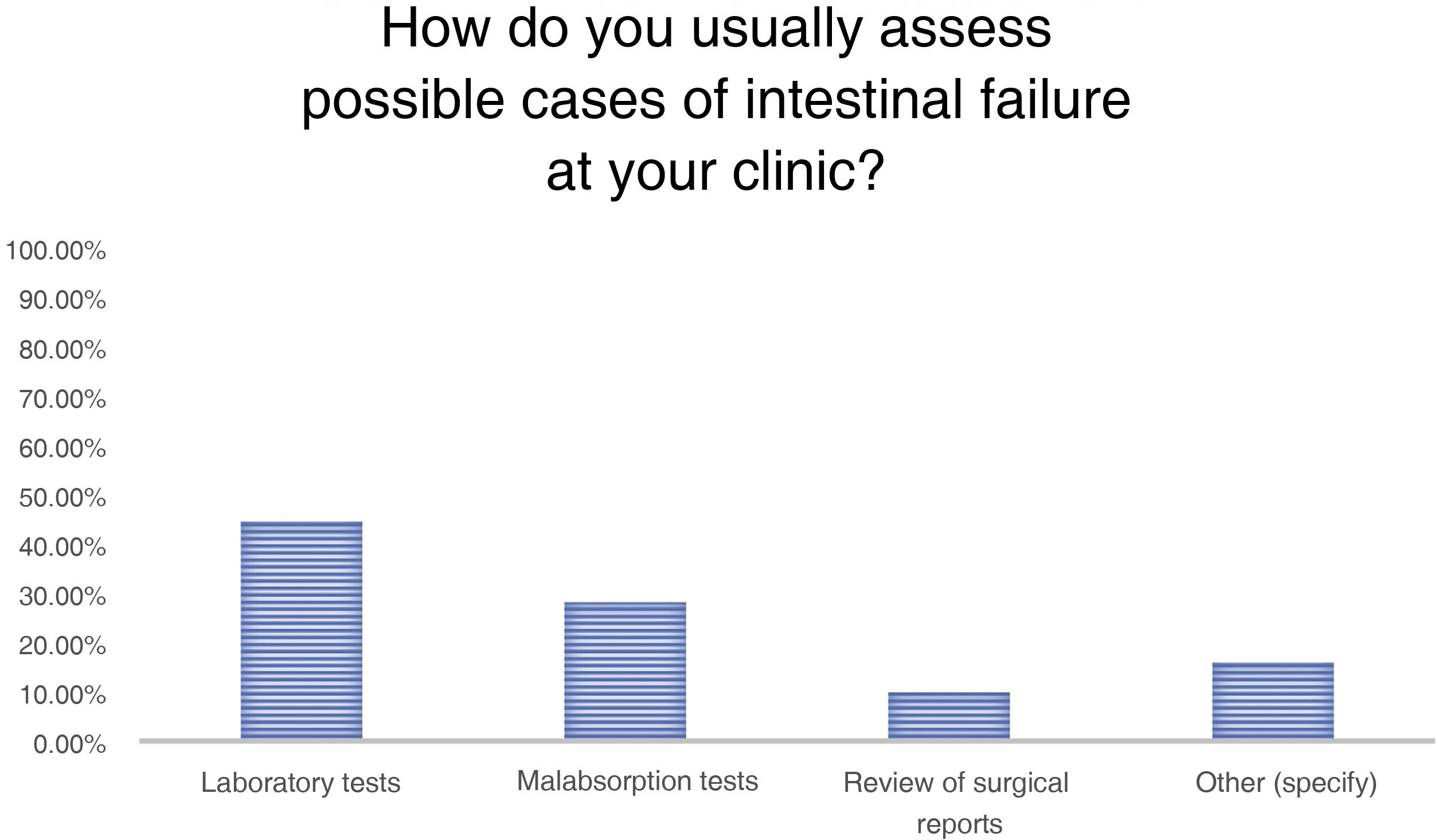
The responses in terms of which patients they order tests for to investigate possible intestinal failure and the actual tests ordered are shown in graph form in Figs. 1 and 2.
Lastly, for the therapeutic management of patients with CD and intestinal failure, when asked about the treatment of the malabsorption syndrome itself, 40% of those surveyed did not have this information. Among the remainder, most (72.5%, 64 patients) were receiving home parenteral nutrition (with macro and micronutrient supplements as required over the course of their disease).
Twenty-four patients (24/89, 27%) had been prescribed treatment with teduglutide. Of these, around 37.5% (9/24 patients) had no response, another 37.5% (9/24 patients) did show a response and were able to reduce parenteral nutritional requirements, and 25% (6/24 patients) responded well and are currently managing without home parenteral nutrition. The mean length of treatment was 24 months.
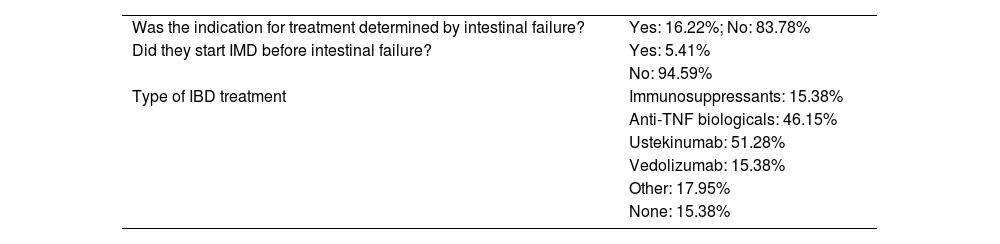
In terms of the baseline treatment of CD, a summary of the most relevant aspects is shown in Table 1.
Type of treatment for the inflammatory bowel disease.
| Was the indication for treatment determined by intestinal failure? | Yes: 16.22%; No: 83.78% |
| Did they start IMD before intestinal failure? | Yes: 5.41% |
| No: 94.59% | |
| Type of IBD treatment | Immunosuppressants: 15.38% |
| Anti-TNF biologicals: 46.15% | |
| Ustekinumab: 51.28% | |
| Vedolizumab: 15.38% | |
| Other: 17.95% | |
| None: 15.38% |
IBD: inflammatory bowel disease; IMD: immunomodulatory drug.
Once a patient was diagnosed with intestinal failure, regardless of the cause, in a third of the cases they were managed exclusively by an endocrine-nutrition team and in another third a coordinated multidisciplinary approach was used, although there was only a specific unit in 16.7% of cases. Only in 4.2% was follow-up and management carried out exclusively by gastroenterology. However, when the cause of intestinal failure was CD, a majority of the respondents (59.2%, 29/49) reported joint gastroenterology-nutrition management, having the possibility in 36.8% (18/49) of cases of presenting the case to a committee for multidisciplinary follow-up (for example, nutrition, surgery, gastroenterology).
Lastly, the survey respondents were asked questions relating to their knowledge about and training in intestinal failure, with knowledge generally being limited (53.1%) or very limited (12.2%). However, most of the participants considered it very necessary (38.8%) or quite useful (55.1%) to receive specific training in this subject.
Despite this, 83.3% of those surveyed did not know whether there was a specialised intestinal failure unit in their autonomous region where they could refer these patients, and 95.9% considered it necessary to have specialised units in Spain for this disease.
DiscussionCurrent clinical practice in the management of patients with CD suggests that secondary intestinal failure is a rare disorder nowadays.15 However, the management of these patients is complex, requiring a multidisciplinary approach due to the significant associated morbidity,16 and this is not always possible within IBD units here in Spain.
In fact, this is the first study to date to explore the current management of patients with intestinal failure secondary to a disease, and which also investigates the knowledge of the physicians responsible for these patients and possible areas for improvement.
There are recent series9,10 which even suggest that CD continues to be a common cause of intestinal failure, but these data have been extrapolated from the experience in other countries, and we do not have recent data in our setting.
The respondents who took part in the survey were mostly gastroenterologists dedicated to IBD who practiced in tertiary hospitals (65.3%) with a specialised IBD management unit (85.7%) and, in most cases, they dealt with a large number of patients with this disease (57.1% more than 1500 patients).
The diagnosis of intestinal failure was well established by most of the respondents, with 67.3% responding; intestinal failure being considered when there was an associated malabsorptive disorder regardless of the length of resected bowel, distinguishing it from the definition of short bowel as a purely anatomical concept.
Additionally, the risk of developing intestinal failure after a surgical procedure in CD is greater when it affects the jejunal-ileal region,17,18 this being acknowledged by most of those surveyed, who considered repeated ileal resections to be of greatest risk (40.8%), followed by extensive ileal or jejunal resections (28.6 and 24.5% respectively).
When asked about the management of patients with CD and intestinal failure, it is significant that 24.5% did not know whether there were patients with either any-cause or CD-related intestinal failure in the hospital where they worked. Moreover, if there were such patients attending their hospital, 40% of those surveyed did not know what treatment they were receiving, highlighting the possible general lack of knowledge or involvement of the gastroenterologist in the follow-up of intestinal failure. In fact, participation was higher in other surveys by the GETECCU group19,20 than in this study, despite us making several appeals via email, and we believe this may be related to the above-mentioned lack of regular dealing with this scenario.
We should point out that in our study, 228 patients were under follow-up for any-cause intestinal failure, and 89 patients (39.5%) for intestinal failure related to CD. Although the study design did not allow us to estimate the prevalence of intestinal failure here in Spain, we gained the impression that CD may be a common cause of intestinal failure in adults in our setting.
Of the drug treatments, teduglutide as a therapeutic option has revolutionised the management of this disease.21 We asked about the use of teduglutide specifically in patients with CD, with respondents reporting experience in 24 patients (27%), providing response rates in most cases (37.5% partial response and 25% complete, withdrawing home parenteral nutrition).
Finally, we consider it significant that the majority of the survey respondents (65.4%) reported having limited knowledge about the management of these patients, despite the fact that, as we mentioned, they are specialists in the management of IBD. There was also little knowledge (83.3%) about the existence of specialised units where these patients could be assessed.
Some studies22 suggest that care in specialised units improves different aspects of the management of complications or peculiarities in these patients. Previous studies23 have shown that the venous access catheter for home parenteral nutrition has greater durability, and in case of failure due to thrombosis it is more likely to be rescued, when patients are followed up in specialised centres.
One of the strengths of our study is that it provides a snapshot of the management of these patients in Spain which could point us to possible areas for improvement in this field. The main limitation is that the study design did not allow us to determine the actual incidence and prevalence of intestinal failure in patients with CD in our setting, which would have enabled a more exhaustive study on the management of this condition.
ConclusionsKnowledge about the management of patients with CD-related intestinal failure among physicians dedicated to inflammatory disease is in many cases limited, possibly because of the low incidence in our setting. However, there are areas for improvement that could benefit the management of these patients, the use of targeted medical treatment and, ultimately, their quality of life.
FundingNo funding was received for this work.
Conflicts of interestThe authors declare that they have no conflicts of interest.