Borderline Personality Disorder (BPD) and dissociative experiences are frequently co-occurring conditions. This study aimed to assess the relationship between DSM-5 Alternative Model of Personality Disorder (AMPD) maladaptive personality facets and self-report dissociation in a sample of patients with BPD.
MethodsOur sample consisted of 178 Italian adult patients who met the criteria for BPD diagnosed by Structured Clinical Interview for DSM IV-Axis II. They were administered the Personality Inventory for DSM-5 (PID-5) and the Dissociative Experiences Scale (DES). An agglomerative hierarchical cluster analysis was performed using facets as clustering variables. Multivariable regression analysis was performed to identify the PID-5 characteristics which could suggest a dissociative dimension.
ResultsOur results showed the potential of PID-5 to hypothesize a dissociative dimension towards DES scores. Therefore, we theorized a specific BPD phenotype characterized by high levels of Unusual Behaviors and Beliefs, high levels of Perceptual Dysregulation, high levels of Withdrawal, low levels of Impulsivity and Irritability, low levels of Callousness and low levels of Avoidance, for which it may be assumed a dissociative framework. Moreover, it could be postulated that patients with dissociative symptoms who will be diagnosed with BPD according to the AMDP would have the domain of Psychoticism as “specifier”.
Lastly, we highlighted the role of gender as a moderator between personality traits and dissociative symptoms.
ConclusionConsistently with this study, an initial assessment with PID-5 personality facets may detect an underlying dissociative psychopathology, suggesting significant clinical implications for both treatment and prognosis.
Borderline personality disorder (BPD) is a complex clinical entity, whose manifestations affect several aspects of life.1 BPD is characterized by instability which affects emotions, mood, behaviors, relationships and the sense of self. Such individuals suffer the loss of an integrated sense of identity and tend to develop dissociative spectrum disorders.2 Indeed, the presence of severe dissociative symptoms has been listed among the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria of BPD.3
Moreover, it is widely known the comorbidity with characteristic post-traumatic stress disorders (PTSDs), such as proper PTSD, complex-PTSD and dissociative-PTSD.2 The exposure to childhood adverse life events seems to be associated with the subsequent development of BPD.4 Some authors outlined a specific entity called “traumatic dissociative dimension”5 accounting for the symptom overlap found among BPD, dissociative disorders (DDs) and complex-PTSD.6 Regarding the interaction between dissociation and BPD, the most frequent dissociative experiences are observed in patients with DDs, followed by PTSD, and BPD.7 Furthermore, it was reported that up to 75–80 % of individuals with BPD experience symptoms that may be ascribed to the dissociative spectrum during their lifetime.8
Furthermore, considering the increasing spread and fortune of the DSM-5 Alternative Model of Personality Disorders (AMDP),9 we focused on the relevant clinical implications of dissociative symptoms in patients with a dimensionally oriented diagnosis of BPD. For instance, the facets of Depressivity and Perceptual Dysregulation (e.g. dissociation) seem to explain the high suicidal risk in patients with BPD and childhood trauma, and this association is even more specific if the severity of borderline symptomatology is measured through the Personality Inventory for DSM-5 (PID-5).10 Nevertheless, studies targeted to detect dissociative experiences in BPD, specifically in relation to AMDP, still seem to be lacking. To fill this gap, Yalch and Hopwood11 compared the PID-5 with the Computer Adaptive Test of Personality Disorder (CAT-PD), demonstrating strong convergent and discriminant validity for their common traits, while proving that CAT-PD traits that were not represented in the PID-5 system (e.g. Dissociation) could provide incremental validity over and above traits in the DSM-5 model. As a consequence, this statement paves the way for future research.
The aim of this study is to examine the occurrence of dissociation and related psychopathology in a sample of BPD patients, using as diagnostic instruments the Dissociative Experiences Scale (DES)12,13 and the Personality Inventory for DSM-5 (PID-5) .14 Particularly, we aimed to identify the potential of PID-5 facets to hypothesize a dissociative dimension towards DES score. We proposed to explain PID-5 facets as variables which contribute to dissociative experiences, focusing on a correlation between personality traits and dissociation. Lastly, we investigated the role of gender as moderator on the relationship between some PID-5 facets and DES scores.
Material and methodsDesign and settingThis cross-sectional study was conducted in Community Mental Healthcare Centers (CMHCs) of Bologna, from January 2017 to October 2022.
ParticipantsSubjects aged 18 or more referred to CMHC and satisfying DSM-5 diagnostic criteria for BPD were considered to participate in the study. Exclusion criteria were: schizophrenia spectrum disorders, intellectual disability, neurological disease, difficulty in understanding Italian.
ProcedureSuitable patients were informed about the study and asked to fill in the informed consent and a sociodemographic and clinical form. They were informed that data provided in the study would be anonymous and that their participation in the research would be voluntary.
The study started in 2013, so that the Structured Clinical Interview for DSM IV-Axis II15 was administered and conducted by trained personnel to confirm the diagnosis of BPD, Subsequently, the Structured Clinical Interview for DSM-5 was introduced and patients meeting DSM categorical BPD criteria received the diagnosis with both tools. Comorbidities were assessed through clinical diagnosis. Next, participants completed a set of multiple self-report questionnaires. Data from two research projects approved by the Ethical Committee (EC) of the Bologna Local Health Unit were included in the present database: EC code 0,002,045 (25/11/2013) and EC code: 297/2018 (06/15/2018).
MeasuresThe PID-5 is a self-administered psychometric questionnaire which consists of 220 items for the assessment of maladaptive personality traits14,16 according to the AMDP.9 Each item is constituted by a 4-point Likert score (from 0 = "always false / often false" to 3 = "always true / often true"), while the traits are described through 25 facets, grouped into 5 high-order domains: Negative Affectivity, Detachment, Antagonism, Disinhibition and Psychoticism. The PID-5 aims to develop a dimensional model consisting of dysfunctional variants of the main dimensions of personality: indeed, traits such as Emotional Lability, Anxiety, Separation insecurity, Depressivity, Impulsivity, Risk Taking and Hostility are consistent with the criteria used in the categorical diagnosis of BPD, additionally PID-5 highlights the relevance of Psychoticism and dissociative experiences.
The DES12,13 is a self-assessed scale consisting of 28 questions which describe various dissociative experiences, for which the subject must indicate how often they occur. It is a Likert scale, with the score given by the average of the scores of the individual items, ranging from 0 to 100. Scores 〈 20 are usually found in healthy patients or in patients without DDs, while scores 〉 30 are associated with a diagnosis of DD. This tool outlines three types of dissociation organized on a dimensional model: Absorption and Imaginative involvement, Depersonalization/Derealization, Dissociative Amnesia. We made a further distinction between Positive symptoms – such as flashbacks and intrusive thoughts - and Negative symptoms, defined by the inability to access one's own information and motor control processes.
DES - Taxon (DES-T)17 is a 8-item subscale developed as a screening tool to distinguish between pathological and non-pathological dissociation.
Statistical analysisStatistical analyses were performed with the R. An agglomerative hierarchical cluster analysis was conducted using facets as clustering variables. Agglomerative Hierarchical Clustering (HC) was performed to determine the best clustering of units. We performed several HC procedures. For those algorithms that require a distance matrix, we computed the Euclidean distance. The different algorithms used gave very similar results. Due to the high performance in partitioning and assigning units to groups, we present the partition obtained by the Ward procedure.
Using HC, we grouped patients in such a way that objects in the same group are more similar to each other in terms of personality traits. To study specific patient profiles, once the groups were identified, we analyzed the clusters in terms of DES scores.
For these scales, we used one-way analysis of variance (ANOVA) to explore the different cluster characteristics. Tukey's honest significant difference was used as a post-hoc test, and effect sizes were performed using partial eta squared (partial η2).
Multivariable regression analysis was performed to identify the PID-5 characteristics that predicted DES scores. We tested for the absence of outliers (Malhahobis distance) and distributional assumptions (Mardia test and Anderson-Darling test). These tests showed that the distribution of all DES scores was normal. Thus, a stepwise procedure was implemented to identify the models that best predicted each of the DES scores. This regression analysis allows us to identify PID-5 facets that contribute to the prediction of the forms of dissociation measured by DES. Basing on these results, a second cluster analysis was performed. The latter analysis was performed using PID-5 facets as variables that contributed to the prediction of DES scores in the regression analysis.
Finally, a multivariable regression analysis was repeated by introducing an interaction term between gender and individual traits into the models previously selected by the stepwise procedure. To keep the number of estimated coefficients acceptable, one interaction term was introduced at a time.
ResultsA total of 196 patients with BPD were included in the study (mean age =:31.05 ± 9.78, 80.1 % females).
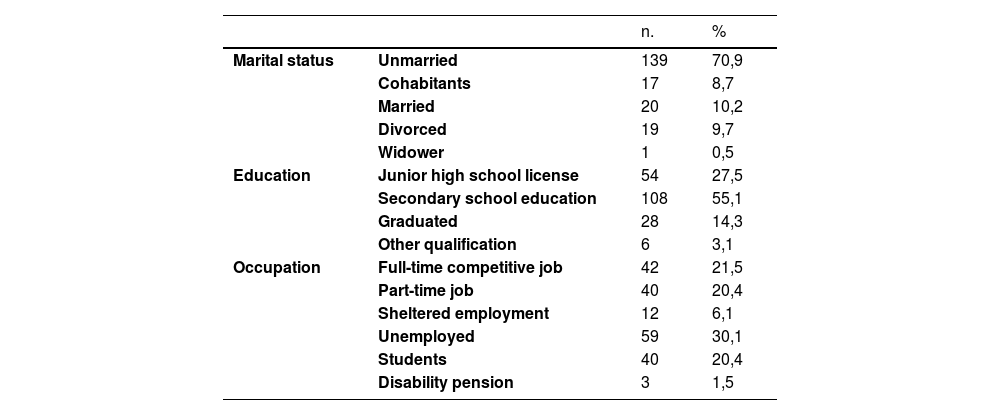
The sample was examined for sociodemographic characteristics [Table 1] and comorbidities [Table 2].
Sociodemographic characteristics of the sample.
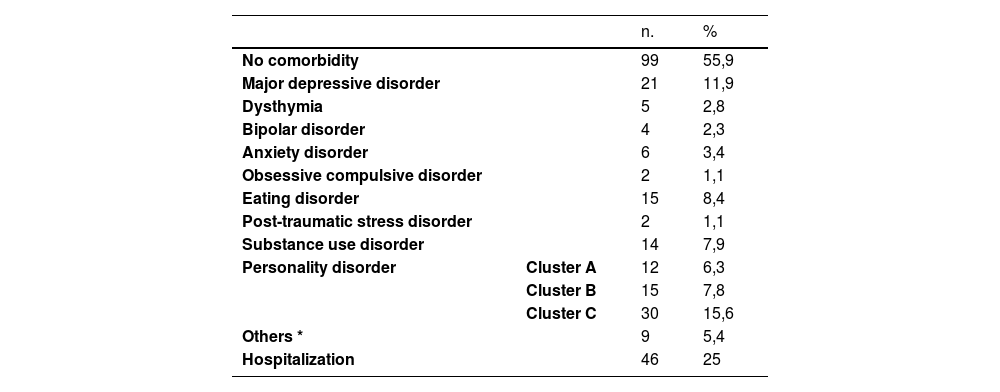
Comorbidities and history of hospitalizations in the past year after having received the evaluation.
*Others: adjustment or conduct disorder, gender disphoria, sleep disorder, disorders belonging to the sphere of hysteria and other nonorganic psychoses.
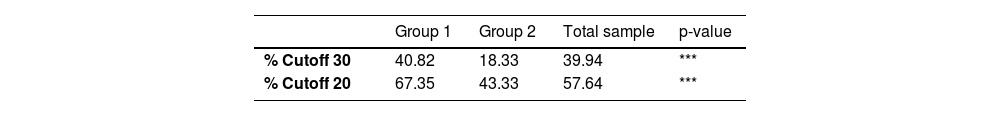
178 out of 196 patients completed the DES instrument (90.8 %). The total mean DES score was 22.52, with standard deviation of 15.76. Our data showed that 30 % of patients report low levels of dissociation (DES score < 10), 44 % moderate levels (DES score between 10 and 30) and 26 % severe levels (DES score > 30).
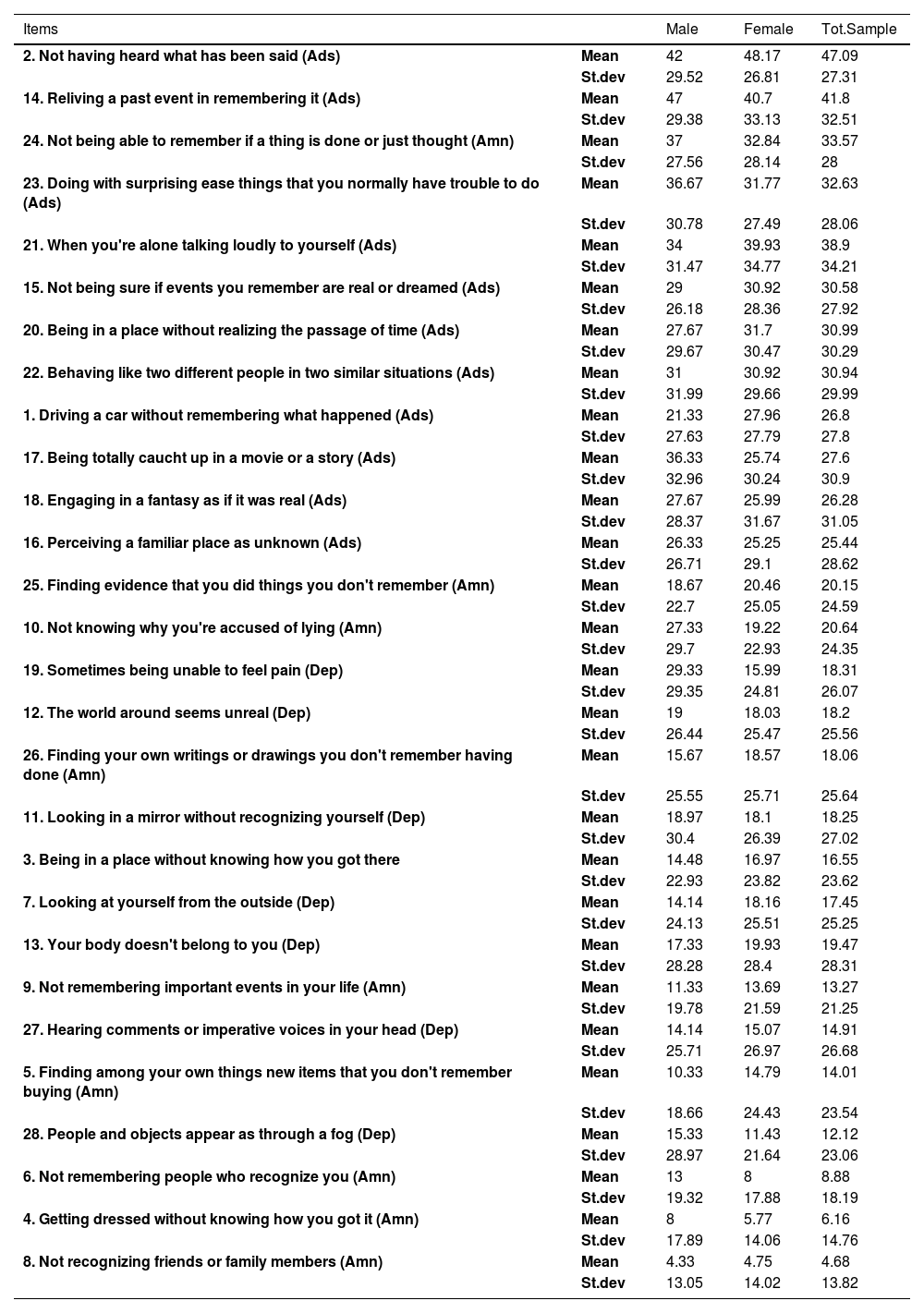
Frequency measures about individual DES items were considered for scores ≥ 20 and differentiated by gender. [Table 3].
Frequency measures about individual DES scores by gender.
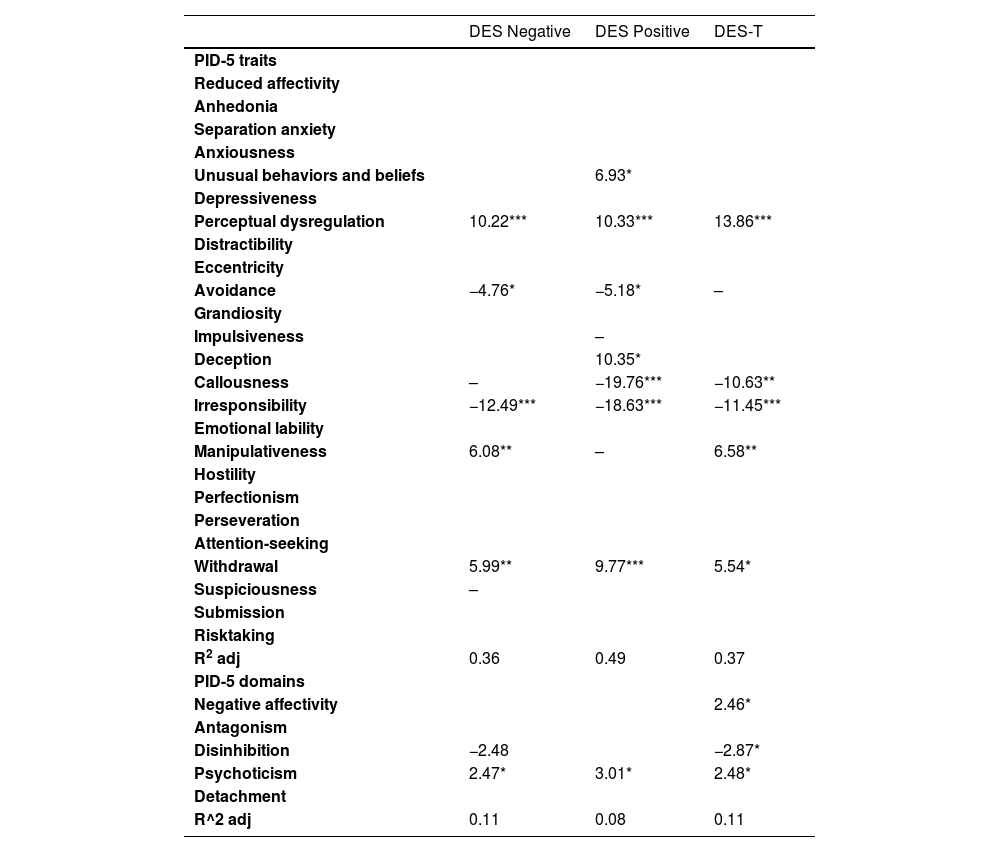
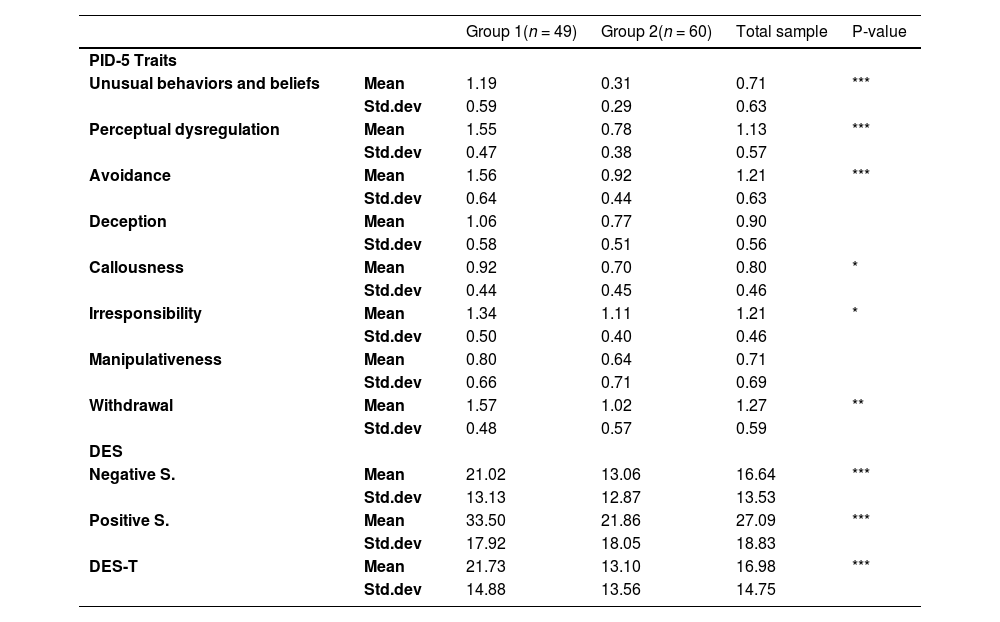
Finally, there were 110 patients with both PID-5 and DES data available. Multivariable regression analysis and cluster analysis were performed on this subsample. [Tables 4 – 5 - 6].
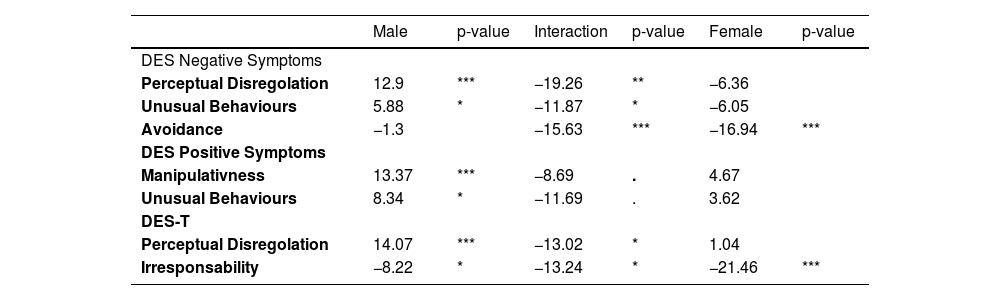
Multivariable regression analysis results.
Notes: Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05. Only statistically significant coefficients have been reported. Blank fields indicate that the trait was excluded from the model specification as a result of the stepwise procedure. Fields with "-" indicate that the trait was included in the model specification following the stepwise procedure but did not produce statistically significant results at the 5 % level.
Descriptive scores of PID-5 traits and DES scores in groups identified through cluster analysis. Differences in the scores between the groups.
The multivariable regression analysis reported that the PID-5 characteristics seemed to detect a high predictive power with for the DES scales, as evidenced by the high R-squared values, suggesting a predictive power of the personality facets in the Alternative Model. Examining the contributions of individual traits, Perceptual Dysregulation appeared to contribute strongly to the prediction of DES Negative and Positive Symptoms and DES-T subscale. Two other facets, Irresponsibility (with a negative coefficient) and Withdrawal, showed significant coefficients for all three DES scores. Manipulativeness was present in all three model specifications selected by the stepwise procedure, but it was not significant for the Positive Symptom score. Callousness also had two significant coefficients, contributing to the best model specification predicting DES Negative Symptoms, as did Avoidance, which had significant negative coefficients only for DES Negative and Positive Symptoms, but not for DES-T subscale.
The final analysis suggest that gender has a moderating effect on the relationship between some PID-5 facets and DES scores. Specifically, the effects of Perceptual Dysregulation, Unusual Behaviors, and Avoidance on DES Negative Symptoms are stronger in males. Additionally, there is a significant gender-related difference in the effects of Manipulativeness and Unusual Behaviors on DES Positive Symptoms, with a stronger effect observed in males. With respect to the DES-T score, our findings show that as Irresponsibility increased, the DES-T score decreased more in females than in males. [Table 7].
Gender effect on DES scores and PID-5 traits.
Just over half of BPD outpatients in our sample reported DES-scores indicating pathological dissociation (52.5 %). Positive Symptoms – e.g., flashbacks and intrusive thoughts of sensory, affective or cognitive nature – were the most frequent experiences. Our results seem to be considerably different from those attested in the literature, which state a general prevalence of dissociation in about 75–80 % of subjects with BPD.18,8 On one hand, these findings point out some methodological problems in assessing dissociation in BPD: the DES is not always used to detect pathological dissociation, but also contains items which represent normal dissociative experiences.19 Similarly to previous authors20 who stratified the severity of the three subtypes of dissociation in a sample of BPD inpatients, we found a lower prevalence of overall dissociative experiences because we chose a cut-off with the aim of detecting pathological dissociation; moreover, this is coherent with our distribution of dissociative phenomenology oriented towards a greater symptom severity. On the other hand, our sample consisted of BPD outpatients following treatment at CMHC, with an average age of 31 years: these variables could account for a relative clinical stability, and so that they could explain the lower prevalence of overall dissociative experiences. Further studies are needed to understand which DES model apply in different BPD samples, and its clinical and prognostic implications.
PID-5 and dissociative dimensionThe main purpose of this study was to theorize the clinical relevance of PID-5 as a tool to point out dissociative experiences in BPD patients, due to its potential to forecast the dissociative dimension scored by DES.
Our regression analysis showed that the PID-5 domain of Psychoticism and the facets of Perceptual Dysregulation, Withdrawal, and Irresponsibility - the latter with an inverse relationship – appeared to foretell both Negative and Positive Symptoms as well as the total score.
Besides, many other facets contributed to the best model specification, showing their effects on the variance of DES total score and DES subscales. Negative Symptoms seem to be related to Manipulativeness and Disinhibition, while Positive Symptoms are associated with Unusual Behaviors and Beliefs, Deception and, with an inverse relationship, to Callousness. Notably, Avoidance detected a negative correlation with both Negative and Positive Symptoms, likewise Irresponsibility reported a significant inverse relationship with all DES scores. As a consequence, our results suggested that PID-5 facets may own intrinsic discriminatory power and could be interpreted as drivers of dissociation.
The domain of psychoticism versus BPD core symptoms: a recurrent “specifier” in dissociationIt is remarkable to note that our results, while attesting the relevance of dissociative psychopathology in the sample, did not detect a strong relationship with the core BPD symptoms. It is well-known, indeed, that the Alternative DSM-5 Model for Personality Disorders (AMDP) requests for the diagnosis of BPD four or more pathological personality traits which are identified as the core symptoms of BPD; the facets are listed below: Emotional Lability, Anxiousness, Separation Insecurity, Depressivity, Impulsivity, Risk-taking, Hostility (Criterion B). On the contrary, our results highlighted the aforementioned personality traits which seem to explain better the model by foreshowing the DES score variance: Perceptual Dysregulation, Unusual Behaviors and Beliefs in Psychoticism domain; Withdrawal and Avoidance in Detachment domain; Irresponsibility in Disinhibition domain; finally, in the Antagonism domain, Manipulativeness, Deception and Callousness.
In particular, no facets related to Psychoticism belong to the core symptoms and, therefore, in AMDP Psychoticism is considered a “specifier”, even if facets of Perceptual Dysregulation, Eccentricity, and Unusual Experiences and Beliefs seem to be the most akin to the dissociative spectrum. Given the transience and presumed less seriousness of delusional ideas of the subject with BPD, the literature has so far produced a stratification of the manifestations of delirium within three levels: "non-psychotic thought", "quasi-psychotic thought” and "true psychotic experiences”.21 Although only the first of these categories is often attributed to subjects with BPD, it is interesting to note that previous other studies attest the presence of effective productive symptoms22,23 :auditory, visual, olfactory and tactile hallucinations are frequently reported in BPD patients, and tend to arise with some peculiarities such as occurring in stressful situations, during interpersonal conflicts or when events related to a previous trauma are recalled to memory. These "trauma-intrusive hallucinations" reveal a correlation with childhood abuse experiences and are associated with high levels of derealization/depersonalization: since these psychotic experiences proper to BPD often prove a traumatic origin, the severity of dissociation may conceal a developmental trauma.22 In addition, such patients report the highest levels of self-harm, paranoid ideation, anxiety and dissociation.23 Consistently, our results on the PID-5 Psychoticism domain were in line with these findings of psychotic phenomena in BPD; nevertheless, according the purpose of AMDP to remove Psychoticism from the list of personality traits that characterize BPD subjects, we expect for the future a large number of BPD diagnosis with Psychoticism as a specifier.
Furthermore, the co-occurrence of psychotic features in BPD is considered as clinical indicator of illness severity, associated with high levels of psychopathology and poor prognosis, emphasizing therefore the detection of psychotic symptoms particularly at the onset of personality disorder.24 Consequently, detecting BPD diagnoses according to the AMDP with Psychoticism as specifier suggest relevant implications for both treatment and prognosis.
The detachment domain: Withdrawal and avoidance traits linked to dissociationAccording to our hypothesis on PID-5 as a model which forecast dissociative experiences in BPD patients, we focused on the domain of Detachment, and in particular on the contribution of Withdrawal and Avoidance traits. Withdrawal seemed to show the potential to outline all dissociative symptoms, even if data on this association is lacking in literature. Indeed, it is well-known that BPD patients are sensitive to abandonment, so that they react negatively when they perceive to be distanced or rejected by other people. As a result, they tend to withdraw, but this behavior only aggravates their social and internal stigma.25 Our results showed that Withdrawal could anticipate the occurrence of dissociative experiences in patients with BPD. Unexpectedly, we found an inverse correlation between Avoidance and Positive and Negative symptoms. This data was quite in contrast with previous findings in the literature, which reported that BPD subjects with high levels of emptiness and dissociation also exhibited emotional distress and attachment avoidance.26 Given that dissociation is keen to occur in stressful situations, we suggested that Avoidance could represent a defense mechanism, while Withdrawal would become a consequence of failure of the mechanism above.
Dissociation severity and facet cluster: clinical implicationsOnce identified the personality facets with the suggestive potential to pinpoint dissociation, we carried out a cluster analysis dividing the sample into two subgroups of patients: the first group reported moderate to severe level of dissociation, while the second one reported only mild levels. This clustering was assessed not only in relation to PID-5 facets, but also for DES scores.
These aspects may be useful at the diagnostic stage, suggesting further clinical implications. Thus, the interest of this study was to theorize the potentiality to assess dissociative experiences from PID-5 facets: with our analysis, we detected the contribution of each trait and outlined what appeared to be the drivers of dissociation. When a patient with BPD reports at PID-5 facets high levels of Unusual Behaviors and Beliefs score, high levels of Perceptual Dysregulation score, high levels of Withdrawal, but low levels of Avoidance and Impulsivity and Callousness score, the clinician may be led to hypothesize a dissociative framework. Consistently, this cluster analysis emphasized the opportunity to postulate an initial classification of dissociative symptomatology as early from the PID-5 assessment.
Our results suggested a negative association between dissociation and personality facets such as Impulsivity and Irresponsibility, establishing another peculiar finding compared to literature. Indeed, it is well known that adults exposed to adverse childhood experiences and patients with BPD share similar brain alterations in the amygdala, prefrontal cortex and hippocampus, resulting in neurocognitive impairments which involve increased impulsivity, altered inhibitory control and dissociative experiences.27
With respect such heterogeneity of BPD clinical presentation, some authors identified temperament-based BPD subtypes (Low-Anxiety subtype, Inhibited subtype, Emotional/Dishinibited subtype whom dissociative symptoms belong) and pointed out their different response to standard Dialectical Behavior Therapy (DBT).28 On the other hand, the frequent comorbidity between BPD and PTSD led to the necessity to develop more specific treatments integrating DBT with trauma-targeted approaches29 :several studies are showing the efficacy of DBT with trauma-focused cognitive-behavioral approaches such as DBT-PTSD,30 Eye Movement Desensitization and Reprocessing-DBT (EMDR-DBT)29 and DBT-Prolonged Exposure (PE) .31
Consequently, the possibility to detect a dissociative framework since the early PID-5 assessment could orientate clinicians in the diagnostic process as well in therapeutic strategies.
The role of genderConsidering the high prevalence of females in our sample (80,1 % of subjects), we investigated the role of gender as a moderator of dissociation.
Cavelti and colleagues32 introduced the role of gender as a variable influencing the heterogeneous presentation of BPD. In a sample of adolescents, they attested that females presented more frequently childhood traumatic experiences, emotional dysregulation and internalizing psychopathology, whereas males showed high level of impulsivity, dissocial behavior personality trait and externalizing psychopathology. According to a line of research focused on psychopathology of adolescents in the juvenile justice system and their differences by gender, girls resulted to display higher scores on dissociative symptoms and BPD traits, while boys were higher on callousness33; on the other hand, polyvictimization was investigated as the underlying mechanism linking dissociation with BPD in girls and callousness-unemotional traits in boys.34 These findings were consistent with our own, supporting the inverse relation between Impulsivity or Callousness and dissociative symptoms outlined in our sample of predominantly female subjects.
Furthermore, this study hypothesized that gender would have a moderating effect on the relationship between further PID-5 facets and DES scores. In particular, the effects of Perceptual Dysregulation and Unusual Behaviors on DES Negative Symptoms seemed to be stronger in males, while the effects of Avoidance in females. Additionally, we delineated a significant gender-related difference in the effects of Manipulativeness and Unusual Behaviors on DES Positive Symptoms, with a stronger effect observed in males. Bach and Fjelsted,10 administering the PID-5 to their sample of BPD outpatients, pointed out the role of Perceptual Dysregulation (including features of dissociative proness) as a mediator between childhood trauma and current suicidal risk: specifically, they investigated how trauma disrupts the normal development of cognitive and affective processing, as well as the use of language to express emotional experiences; as a consequence, children will be lead to process traumatic events on a non-verbal level.35 In addition, in the literature is represented a majority of studies focusing on trauma in females rather than in males,36 while gender differences are reported to influence also the subjective response to traumatic experiences: women tend to show more defensive or emotion-focused coping mechanisms, while men more problem-focused coping style; consequently, women are more keen than men to seek social support, which is the great predictor of positive trauma outcomes.37
According to our cluster analysis, we postulated that BPD patients reporting at PID-5 facet high levels of Unusual Behaviors and Beliefs score, high levels of Perceptual Dysregulation score, high levels of Withdrawal score but low levels of Avoidance and Irresponsibility scores tend to show a dissociative framework: these results may be interpreted considering the role of gender in our sample. Thereby, the high female prevalence could explain the strong inverse relationship with Avoidance trait: the capacity of avoiding conflicts or stressful situations may be interpreted as a protective factor against the development of dissociative symptoms. On the other hand, the male subjects of the sample displayed higher level of Perceptual Dysregulation, which may conceal dysfunctional coping mechanism to underlying traumatic experiences. These preliminary findings highlight the effect of gender as a moderator of dissociation and, notably, suggest clinicians to investigate dissociative framework in BPD patients, to improve positive coping skills (e.g. Avoidance in females) or to target negative prognostic factors (e.g. Perceptual Dysregulation in males).
Strenghts and limitationsThis study presents several limitations. First, it was organized according to a cross-sectional rather than a longitudinal observational design that, as a result, did not allow us to assess the role of dissociation on the progress of BPD. Moreover, the intrinsic structure of the self-administered tests that we used has been another limitation: each patient may have been led to either overestimate or underestimate perceived symptoms. Lastly, the sample size was limited (122 patients), which would make the findings less robust especially for interaction analyses; our sample consisted predominantly of female subjects, as it is frequently reported in studies conducted on BPD population.38 On the other hand, the strengths of this research were the homogeneity of the sample which included outpatients with a low proportion of comorbidities.
In conclusion, this study hypothesized the potentiality of PID-5 to forecast dissociative experiences as recorded by DES scores. We theorized a BPD phenotype characterized by high levels of Unusual Behaviors and Beliefs, high levels of Perceptual Dysregulation, high levels of Withdrawal, low levels of Impulsivity and Irritability, low levels of Callousness and low levels of Avoidance, for which it may be suggested a dissociative framework. Moreover, we highlighted the role of gender as a moderator between personality facets and dissociative symptoms. Lastly, our analysis confirmed DES-T to be a screening tool consistent in its results with the extended scale.39 Indeed, DES-T subscale showed a coherent potential capacity to postulate the above PID-5 facets, such as Perceptual Dysregulation, Withdrawal, Manipulativeness and Avoidance.
The relevance of our research was to propose a specific constellation of personality facets which would be able to point out the presence of dissociative psychopathology, and for which we recommend a tailored approach in clinical practice.
Ethical disclosuresN/A.
FundingThere was no funding for this work.
None.
Location of the institution and place where the work was done:
Department of Biomedical and Neuromotor Sciences, University of Bologna, Viale C. Pepoli 5, 40,123 Bologna, Italy